Chronic Disseminated Intravascular Coagulation in Patient With Metastatic Gastrointestinal Stromal Tumor: Treating Bleeding With Anticoagulation
DOI:
https://doi.org/10.14740/jmc5164Keywords:
Disseminated intravascular coagulation, Gastrointestinal stromal tumor, Tyrosine kinase inhibitor, Thromboembolism, AnticoagulationAbstract
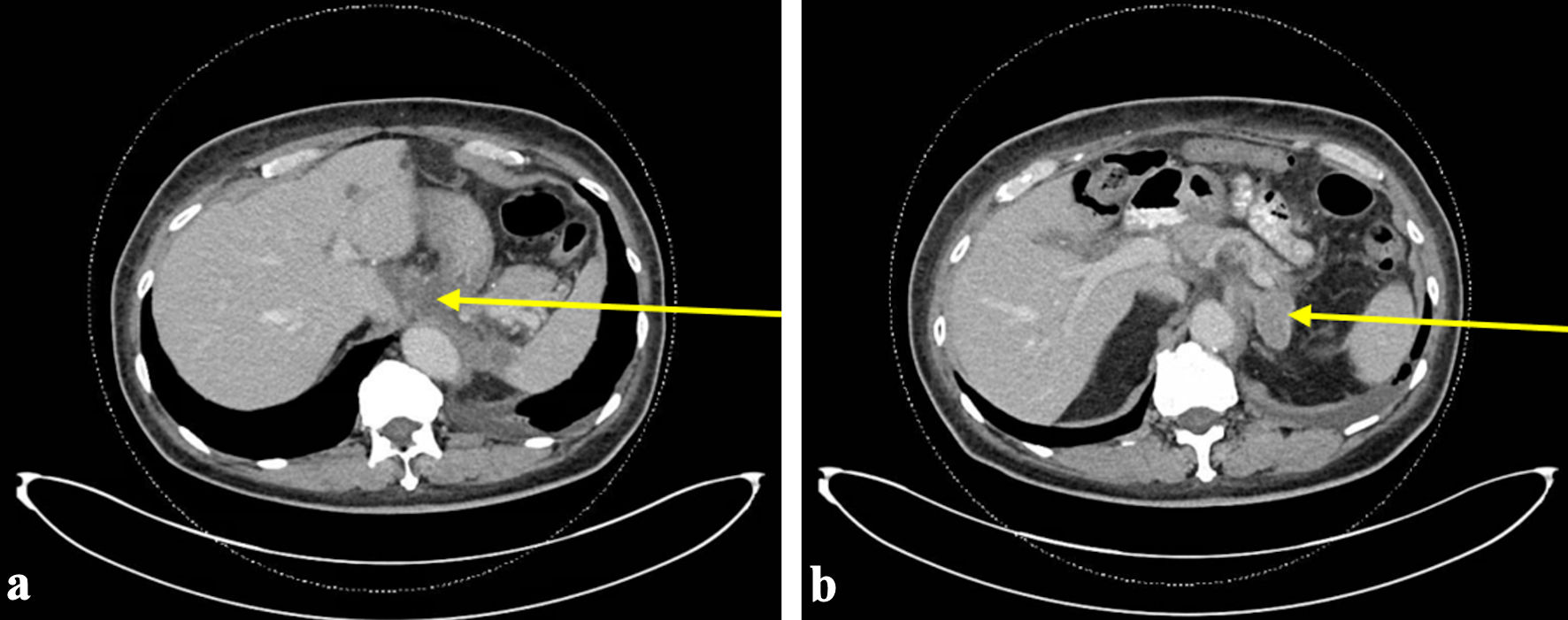
Disseminated intravascular coagulation (DIC) is an uncontrolled activation of the coagulation cascade which is often a complication observed in patients with malignancies. DIC can occur in both hematologic and solid malignancies. Management of DIC is often focused on treating the underlying cause and supportive care, which varies based on thrombotic versus bleeding-predominant phenotypes. We report a case of a 69-year-old man with metastatic malignant gastrointestinal stromal tumor (GIST) diagnosed 9 years prior and actively on imatinib, who presented to the emergency department (ED) with gingival bleeding. On presentation, he was hypertensive with active gingival bleeding and was found to have anemia, thrombocytopenia, and mildly elevated coagulation parameters. His initial bleeding was thought to be due to poor dental hygiene and thrombocytopenia, which may be a side effect of imatinib. His imatinib was discontinued, yet he returned to the ED within 2 days with hematuria and melanic stools. He developed multiple sources of bleeding with worsening bicytopenia, progressive coagulopathy, and high levels of fibrin degradation products. He was diagnosed with DIC. He went on to have four additional hospitalizations for bleeding from various sites and abdominal pain. His DIC was attributed to malignancy with findings of disease progression, tumor thrombi, pulmonary embolism, and intracranial hemorrhage through his course. This case represents a rare occurrence of chronic DIC in metastatic GIST and is only the second known report of chronic DIC in a patient with GIST. Despite adjustments to his cancer therapies and anticoagulation, he continued to have episodes of DIC with frequent hospitalizations and ultimately death. Further research is warranted on the selection of and potential variability in bleeding risks of different anticoagulants in DIC. The complexity of tumor-induced coagulopathy and impact of cancer therapies on coagulation highlights the need for additional research into tailored management to improve outcomes in similar cases.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.