| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 6, June 2025, pages 232-237
Paraspinal Intramuscular Hemangioma at L5-S1 With Concurrent Disc Herniation
Hamza Mahdia, b, d, Pat Anthony Allevatob, Abdul Haseeb Naeemc
aSchulich School of Medicine and Dentistry, Windsor, Canada
bDepartment of Pathology and Laboratory Medicine, Windsor Regional Hospital, Windsor, Canada
cDepartment of Neurosurgery, Windsor Regional Hospital, Windsor, Canada
dCorresponding Author: Hamza Mahdi, Schulich School of Medicine and Dentistry, Windsor, Canada
Manuscript submitted April 21, 2025, accepted June 21, 2025, published online June 30, 2025
Short title: Paraspinal Hemangioma With L5-S1 Disc Herniation
doi: https://doi.org/10.14740/jmc5132
| Abstract | ▴Top |
Intramuscular hemangiomas are rare, benign vascular tumors, with very few reported cases arising in lumbar paraspinal muscles. We describe the seventh documented adult case involving a 39-year-old male presenting with acute severe right-sided S1 radiculopathy. Magnetic resonance imaging (MRI) identified an 8.0 × 3.0 × 3.3 cm lesion within the erector spinae muscles at the L5-S1 level, accompanied by concurrent right-sided L5-S1 disc herniation compressing the S1 nerve root. Conservative treatment initially alleviated radicular pain, but persistent back pain and diagnostic uncertainty necessitated further evaluation. Negative metastatic screening and an inconclusive computed tomography (CT)-guided biopsy led to surgical excision, revealing an intramuscular hemangioma with significant adipocytic stromal components. This case highlights diagnostic challenges and underscores the importance of including vascular lesions in the differential diagnosis of persistent back pain, particularly when coexisting spinal pathologies complicate clinical presentation.
Keywords: Intramuscular hemangioma; Lumbar paraspinal muscles; Erector spinae; Surgical excision; Histopathology; Vascular tumor; Literature review
| Introduction | ▴Top |
Intramuscular hemangiomas are rare benign vascular tumors that manifest as slow-growing, sometimes painful masses within skeletal muscle [1-3]. They represent < 1% of all benign vascular tumors, arise predominantly in adolescents and young adults, and show no clear sex predilection. Most occur in the lower limbs, head-and-neck region, or upper limbs, whereas the trunk is an uncommon site. Magnetic resonance imaging (MRI) is the diagnostic modality of choice, and management spans observation, sclerotherapy, and complete surgical excision, with the latter offering the lowest recurrence rates [5, 6, 8-10].
Paraspinal intramuscular hemangiomas are exceptionally uncommon, with only six well-documented adult lumbar cases published between 2000 and 2024 [11-15]. Their clinical picture often mimics more prevalent spinal disorders such as disc herniation, delaying diagnosis and complicating treatment planning. When symptomatic, surgical excision is generally favored, but operative strategy must accommodate the lesion’s vascularity, proximity to neural structures, and potential for recurrence.
We present the seventh reported adult case of a lumbar paraspinal intramuscular hemangioma, unique for its concurrence with an L5-S1 disc herniation, to illustrate diagnostic pitfalls and operative considerations.
| Case Report | ▴Top |
Initial presentation
A 39-year-old man presented to the emergency department with acute, severe right-sided S1 radiculopathy rated 8/10 and localized lower-back pain. MRI of the lumbosacral spine revealed an 8.0 × 3.0 × 3.3 cm well-circumscribed intramuscular mass within the right erector-spinae compartment at L5-S1 (Fig. 1a, arrow) together with a right-sided L5-S1 disc herniation compressing the S1 nerve root (Fig. 1b, arrow).
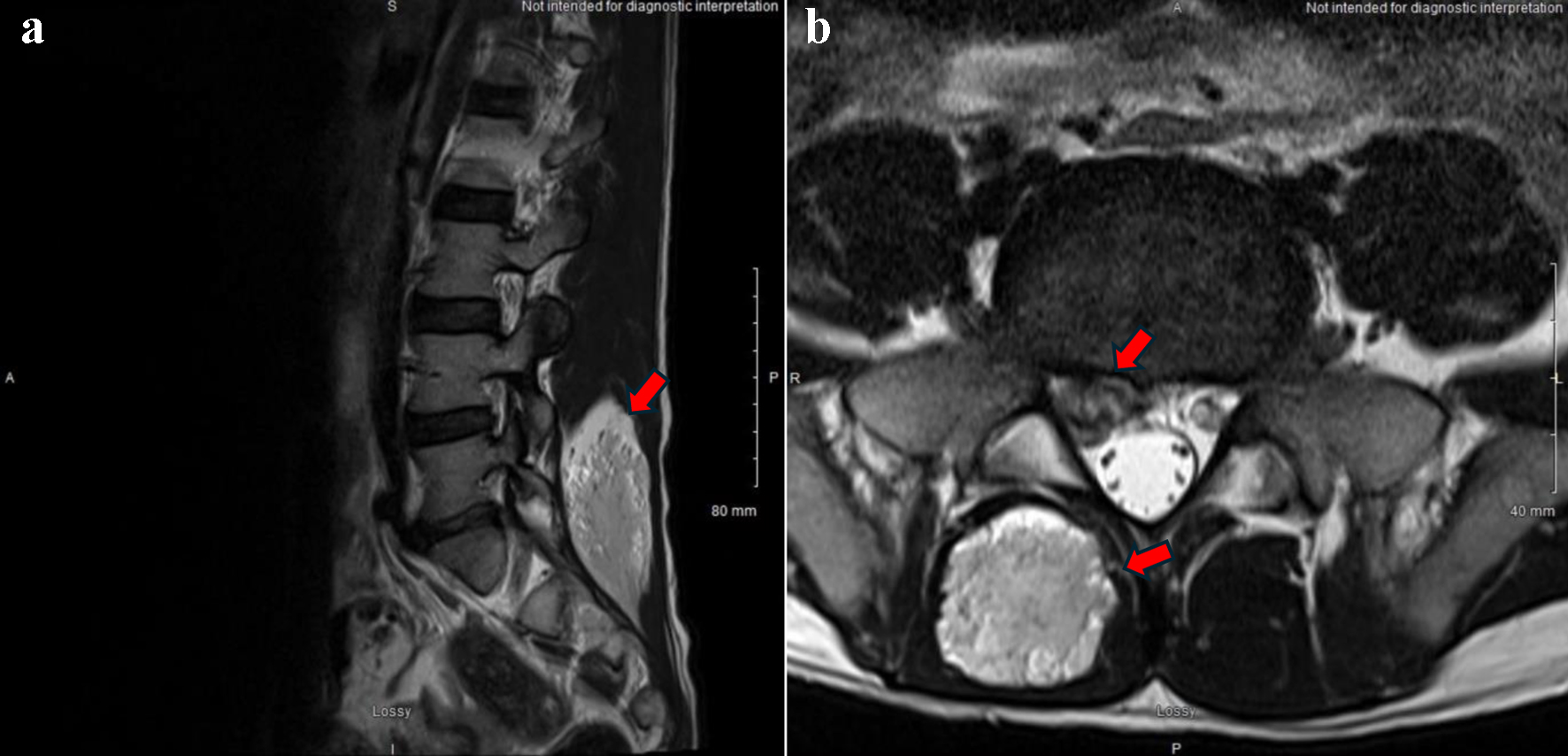 Click for large image | Figure 1. (a) Axial and (b) sagittal T2-weighted MRI show a well-defined mass at L4/L5 extending to L5/S1 (arrows). MRI: magnetic resonance imaging. |
Physical examination
The patient was alert and oriented to person, place, and time. Language function was intact with respect to naming, repetition, and following three-step commands. Cranial-nerve examination showed pupils that were equal and reactive to light with intact accommodation; no visual-field deficits; full extra-ocular movements; normal facial sensation and strength; and hearing that was grossly intact. The tongue protruded in the midline, the uvula elevated symmetrically, and shoulder-shrug strength was full. Motor strength was 5/5 in all major muscle groups of both upper and lower extremities. Sensory examination was intact to light touch and pin-prick. Cerebellar testing revealed no dysmetria or dysdiadochokinesia, and gait was normal.
Diagnostic workup
Computed tomography (CT) of the chest, abdomen, and pelvis showed no evidence of metastatic disease. On unenhanced CT, the paraspinal lesion appeared mildly hypodense relative to skeletal muscle and demonstrated early hyperenhancement after contrast administration, features typical of intramuscular hemangioma. MRI characteristics of such lesions classically include iso- to mildly hyperintense signal on T1-weighted images, moderate T2 hyperintensity with possible intra- or perilesional flow voids, and homogeneous, robust gadolinium enhancement [16].
A CT-guided core biopsy of the paraspinal mass was non-diagnostic. Conservative therapy with analgesics and physiotherapy improved radicular symptoms to 3-4/10 over 2 weeks, yet the paraspinal mass remained painful and of uncertain etiology. After multidisciplinary discussion, operative excision was recommended.
Surgical management
Tumor excision was performed via a right-sided paramedian incision centered over the identified lesion. Upon dissection through the muscle tissue, a reddish mass was visualized. Under intraoperative microscopic guidance, the mass was carefully isolated and excised in a single, intact specimen using a Penfield #1 dissector. The lesion was quite vascular. Hemostasis was maintained and the incision was closed in a standard fashion.
Pathology analysis
Microscopic findings
Histopathological examination (Fig. 2) revealed a combination of skeletal muscle, mature adipose tissue, fibrous connective tissue, and large, thick-walled smooth muscle-containing blood vessels, characteristic of a hamartoma. No cartilaginous tissue or bone was identified. Fascicles of mature skeletal muscle were infiltrated and surrounded by adipose tissue. The lesion contained a variety of blood vessels, including thick-walled vessels, hybrid vessels resembling arteries, and dilated cavernous blood vessels. Large, thick-walled inter-anastomosing vascular channels were lined by flattened endothelial cells, some of which were occluded by recent and organizing thrombi. Areas of stromal fibrosis and degenerative changes were noted, as well as degenerative-regenerative alterations within the myofibers of the striated muscle fascicles. Vascular congestion and patchy stromal hemorrhage were also evident.
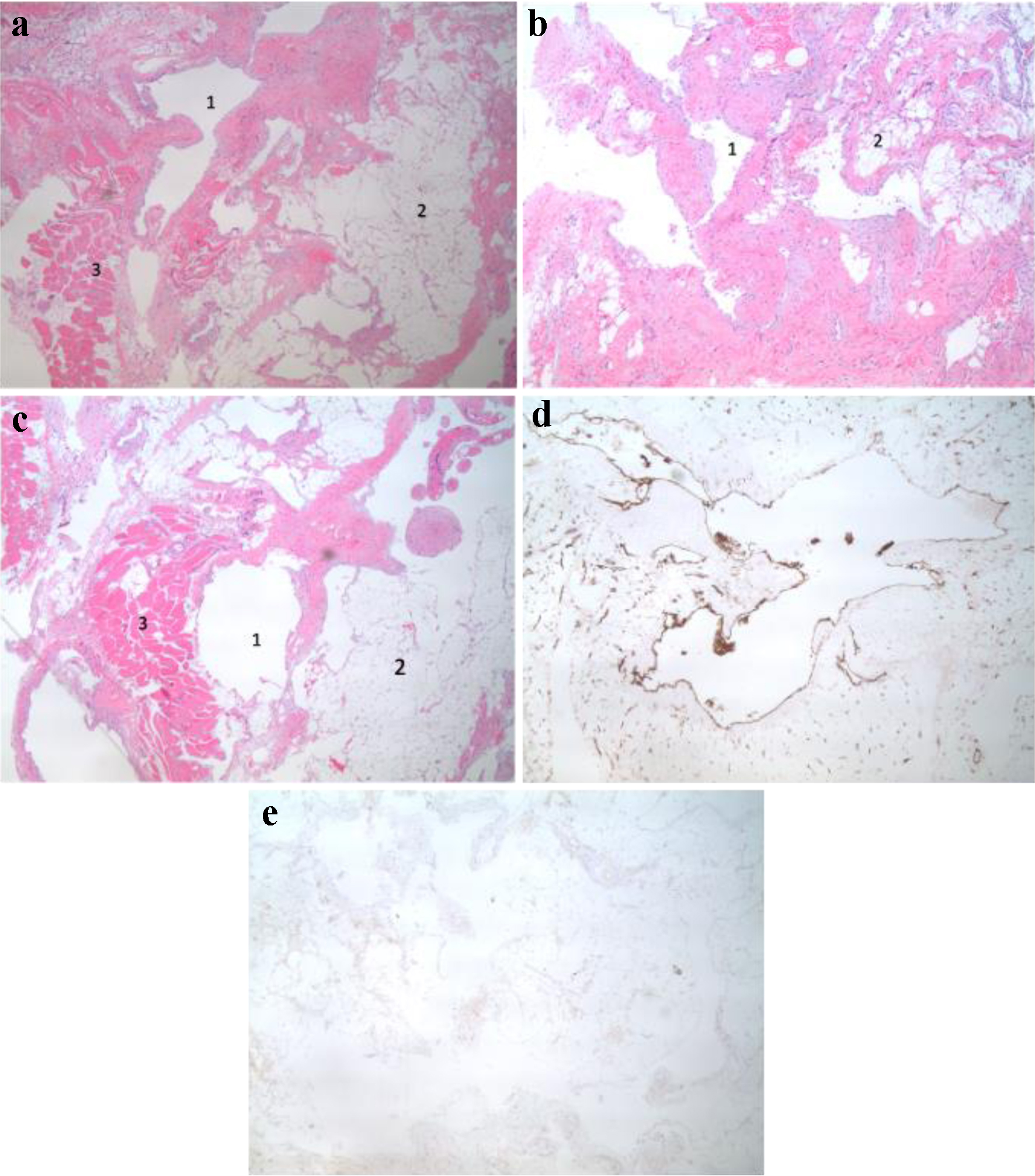 Click for large image | Figure 2. Pathology microscopic and immunohistochemical analysis. (a) Thick wall vascular channels (1) are associated with mature adipose tissue (2) and skeletal muscle (3). (b) Variable sized vascular channels (1) associated with mature adipose tissue (2). (c) Vascular channels (1) associated with lipomatous tissue (2) and skeletal muscle (3). (d) The lining cells express CD31 and represent vascular endothelial cells. (e) D2-40 (podoplanin) is negative ruling out a lymphangioma. |
Immunohistochemical analysis
A panel of immunostains was conducted to further characterize the lesion. The endothelial cells of the large inter-anastomosing blood vessels were positive for CD31 (Dako clone JC70A RTU) and factor VIII-related antigen (Dako polyclonal RTU), and negative for CD34 (Dako clone QB End 10 RTU), D2-40 (podoplanin) (Dako clone D21-40 concentrate), pancytokeratin AE1/3 (Dako RTU clone AE1/AE3 RTU), and S-100 protein (Dako RTU polyclonal). Immunostaining for smooth muscle actin (Dako RTU clone 1A4) and desmin (Dako RTU clone D33) confirmed the presence of smooth muscle fibers within the walls of the large vascular channels. Cytogenetic fluorescence in situ hybridization (FISH) for MDM2 amplification, performed on four FFPE slides with the Vysis MDM2 dual-color probe and 200 interphase nuclei counted, showed no amplification, excluding a lipoma-like atypical lipomatous tumor/well-differentiated liposarcoma.
In summary, the morphological and immunophenotypic findings are consistent with a diagnosis of intramuscular angioma with prominent adipocytic stromal components.
| Discussion | ▴Top |
Intramuscular hemangiomas of the trunk are uncommon, and those arising in lumbar paraspinal musculature are rarer still. Our patient is notable for several reasons: 1) at 39 years he is among the oldest reported adults with a paraspinal intramuscular hemangioma, extending the typical age spectrum that is said to peak before 30 years; 2) trunk lesions constitute only approximately 17% of intramuscular hemangiomas, yet this tumor arose in the erector-spinae compartment at L5-S1; and 3) it is the first documented case complicated by a concurrent L5-S1 disc herniation. The dual pathology generated overlapping radicular and local pain that initially obscured the diagnosis and created a unique operative challenge.
Histologic classification of intramuscular hemangiomas
Allen and Enzinger’s landmark review of 89 skeletal-muscle hemangiomas delineated three variants, i.e., small-vessel, large-vessel, and mixed, reporting local-recurrence rates of 20%, 9%, and 28%, respectively [9]. Beham and Fletcher expanded the schema in 74 cases, classifying lesions as venous, capillary, cavernous, arterio-venous malformation, lymphangioma, cavernous-capillary, and complex malformation; adipocytes were present in 90% of tumors, and > 50% recurred after incomplete excision [8]. Bella et al later showed that wide or marginal excision achieved a 5-year recurrence-free survival of 93% compared with 33% when tumor remained [10]. The thick-walled and cavernous vascular channels with abundant adipose tissue in our specimen align with a complex pattern, reinforcing the importance of complete resection and long-term follow-up.
Paraspinal intramuscular hemangiomas in the literature
Our literature review retrieved six adult lumbar cases published between 2000 and 2024 [11-15] (Table 1) (Supplementary Material 1, jmc.elmerpub.com). Patients were aged 19 - 39 years with equal male-to-female distribution (3:3). Five lesions arose in paraspinal muscles; one involved the gluteus medius, contiguous with the lower back. Tumor sizes ranged 3 - 15 cm. Earlier reports (e.g., [12]) described painless masses, whereas mid-2000s to early-2020s cases [11, 14, 15] often presented with pain mimicking disc herniation, sometimes leading to initial misdiagnosis. All patients underwent surgical excision, with only Swaroop et al reporting recurrence at 2 years, underscoring the necessity for long-term surveillance.
 Click to view | Table 1. Summary of All Lumbar Paraspinal Intramuscular Hemangiomas in Adults Found in the Literature Search |
Diagnostic and therapeutic considerations
The diagnostic challenges encountered in this case are noteworthy. Despite utilizing advanced imaging modalities including MRI and CT, and even pursuing CT-guided biopsy, a definitive pre-operative diagnosis remained elusive. Diagnostic challenges in intramuscular hemangiomas are well documented in the literature, with definitive pre-operative diagnosis often being difficult to achieve. The well-defined appearance on MRI with heterogeneous T2 signal intensity is characteristic but not pathognomonic, necessitating careful differentiation from other soft tissue tumors.
Surgical management of this case presented unique challenges due to both the lesion’s vascularity and its proximity to the herniated disc. Previous case reports have emphasized the importance of complete surgical excision, but none have addressed the additional complexity of managing concurrent disc pathology. The need for meticulous dissection and careful hemostasis was particularly critical given the lesion’s highly vascular nature, consistent with its histopathological classification as a complex malformation with hybrid vessel morphology.
Across the limited literature, consensus on optimal management of asymptomatic intramuscular hemangiomas is lacking. Given the paucity of cases, decisions must be individualized, weighing lesion size, anatomical constraints, patient age, comorbidities, and access to follow-up imaging.
Histopathology and recurrence risk
The mature adipose tissue interspersed with thick-walled, hybrid vascular channels in our case imparted a complex morphology. Such architecture can mimic malignancy radiologically and histologically, yet recurrence is chiefly related to margin status rather than histologic subtype. Our negative margins and planned MRI surveillance align with best-practice recommendations from Bella et al and others.
Conclusion
This case report presents a rare case of paraspinal intramuscular hemangioma in a 39-year-old male, complicated by concurrent L5-S1 disc herniation. It highlights the diagnostic challenges of these lesions, particularly when presenting with overlapping symptoms from spinal pathology. The successful surgical outcome demonstrates that complete excision remains the treatment of choice for symptomatic lesions, even in cases with dual pathology. This report contributes to the limited literature on paraspinal intramuscular hemangiomas by documenting an unusual presentation in an older patient and providing insights into the management of concurrent spinal pathology.
Learning points
Age > 30 years does not exclude hemangioma; maintain it in the differential for paraspinal masses.
Dual spinal pathologies can mask one another; persistent or atypical pain warrants advanced imaging and multidisciplinary review.
MRI features are suggestive but not pathognomonic; a non-diagnostic biopsy should prompt definitive management when feasible.
Complete excision with negative margins offers the best chance of cure and minimizes recurrence risk.
Long-term surveillance is advisable, given documented recurrences up to 2 years after surgery.
| Supplementary Material | ▴Top |
Suppl 1. Search Terms on PubMed for the Literature Review.
Acknowledgments
The authors would like to express their gratitude to Dr. S. Vukmirov-Popovic, pathologist, Hamilton Regional Laboratory Medicine, Hamilton, ON for reviewing the case.
Financial Disclosure
No funding was received for this work.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Informed consent was obtained from the patient.
Author Contributions
Dr. Abdul Naeem was responsible for managing the surgical case and performing the surgery as well as supervising the write up of this case report and guiding the literature review. Dr. Pat Allevato was the pathologist responsible for diagnosing the mass as well as providing the pathology slides shown in this report along with descriptors. Hamza Mahdi was responsible for the write up of the case report as well as performing and writing up the literature review.
Data Availability
The authors declare that data supporting the findings of this study are available within the article and its supplementary information file.
Abbreviations
18F-FDG: 18F-fluorodeoxyglucose; AE1/3: pancytokeratin AE1/3 antibody cocktail; CD31: cluster of differentiation 31 (endothelial marker); CD34: cluster of differentiation 34 (hematopoietic/endothelial marker); CT: computed tomography; D2-40: podoplanin (D2-40 monoclonal antibody); FISH: fluorescence in situ hybridization; HRAS: Harvey rat sarcoma viral oncogene homolog; L5: fifth lumbar vertebra; L5-S1: intervertebral level between the fifth lumbar (L5) and first sacral (S1) vertebrae; MDM2: mouse double minute 2 homolog gene; MRI: magnetic resonance imaging; PET: positron emission tomography; S1: first sacral vertebra/sacral nerve root; US: ultrasound; WHO: World Health Organization
| References | ▴Top |
- WCoTE B. WHO classification of tumors: soft tissue and bone tumors. 2020.
- Yilmaz S, Kozakewich HP, Alomari AI, Fishman SJ, Mulliken JB, Chaudry G. Intramuscular capillary-type hemangioma: radiologic-pathologic correlation. Pediatr Radiol. 2014;44(5):558-565.
doi pubmed - Diogo R, Wood B. Soft-tissue anatomy of the primates: phylogenetic analyses based on the muscles of the head, neck, pectoral region and upper limb, with notes on the evolution of these muscles. J Anat. 2011;219(3):273-359.
doi pubmed - Enzinger FM. Soft tissue tumors. In: Inflammatory Fibrosarcaoma. 1995; p. 288-289.
- Orly J, Bisdorff A, Joly A, Edee AE, Tavernier E, Herbreteau D, Boccara O, et al. Characteristics, natural course and treatment of intramuscular capillary-type haemangioma: a systematic literature review. Acta Derm Venereol. 2023;103:adv00893.
doi pubmed - Wierzbicki JM, Henderson JH, Scarborough MT, Bush CH, Reith JD, Clugston JR. Intramuscular hemangiomas. Sports Health. 2013;5(5):448-454.
doi pubmed - Hein KD, Mulliken JB, Kozakewich HP, Upton J, Burrows PE. Venous malformations of skeletal muscle. Plast Reconstr Surg. 2002;110(7):1625-1635.
doi pubmed - Beham A, Fletcher CD. Intramuscular angioma: a clinicopathological analysis of 74 cases. Histopathology. 1991;18(1):53-59.
doi pubmed - Allen PW, Enzinger FM. Hemangioma of skeletal muscle. An analysis of 89 cases. Cancer. 1972;29(1):8-22.
doi pubmed - Bella GP, Manivel JC, Thompson RC, Jr., Clohisy DR, Cheng EY. Intramuscular hemangioma: recurrence risk related to surgical margins. Clin Orthop Relat Res. 2007;459:186-191.
doi pubmed - Swaroop A, Chaudhury S, Chakraverty U, Singh D. Lumbar para-spinal haemangioma as a rare differential diagnosis of lumbar disc prolapse. Internet J Orthop Surg. 2008;11(1).
- Kim YC, Park HJ, Cinn YW. A case of intramuscular hemangioma of the back. J Dermatol. 2000;27(9):612-614.
doi pubmed - Xue S, Li M, Zhang X, Ning P, Dong C, Guo X, Liu Q. Intramuscular hemangioma capillary type with HRAS mutation: Expanding the molecular genetic spectrum with an emphasis on overlap with arteriovenous malformations and distinct from infantile hemangioma. Hum Pathol. 2024;153:105672.
doi pubmed - Li Y, Chou K, Xiong J, Zhu W, Yu M. Easily misdiagnosed intramuscular hemangioma: a case report. J Int Med Res. 2020;48(12):300060520966897.
doi pubmed - Shin CH, Cho BK, Yoon SH, Hwang SH, Yoon JH. Incidentally found intramuscular hemangioma, mimicking traumatic hematoma after military training: a case report. Korean J Neurotrauma. 2020;16(2):326-331.
doi pubmed - Feger J, Ranchod A, Campos A, et al. Intramuscular hemangiomas. Reference article, Radiopaedia.org (Accessed on Jun 11, 2025).
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.