| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 11, November 2025, pages 461-466
Management of Multilevel Mid-Cervical Fractures in an Adult With Osteopetrosis
Hamza Mahdia, b, c, Abdul Haseeb Naeemb
aSchulich School of Medicine and Dentistry, London, ON, Canada
bDepartment of Neurosurgery, Windsor Regional Hospital, Windsor, ON, Canada
cCorresponding Author: Hamza Mahdi, Schulich School of Medicine and Dentistry, London, ON, Canada
Manuscript submitted September 13, 2025, accepted October 11, 2025, published online October 31, 2025
Short title: Cervical Fracture Management in Osteopetrosis
doi: https://doi.org/10.14740/jmc5205
| Abstract | ▴Top |
Osteopetrosis is a rare inherited osteoclast dysfunction disorder that produces bone that is both abnormally dense and brittle, complicating fracture management and internal fixation. Most cervical spine injuries reported in osteopetrosis involve the craniovertebral junction (C1-C2) and are treated surgically because of presumed instability. Reports of multilevel mid-cervical fractures with ligamentous injury successfully treated nonoperatively are exceedingly scarce. We present the case of a 22-year-old man with longstanding osteopetrosis who sustained high-energy trauma resulting in a displaced posterior-inferior C4 body fracture with associated left C4 lateral-mass involvement, nondisplaced left C3 inferior-facet and C6 pedicle fractures, and magnetic resonance imaging (MRI) evidence of focal cord T2 signal, posterior longitudinal ligament injury, and a small epidural hematoma. Despite this constellation - which, in normal bone, would often mandate operative stabilization - the patient remained neurologically intact, with acceptable alignment and negative vascular imaging. Given the unique surgical hazards of osteopetrotic bone (poor screw purchase, intraoperative fracture risk, delayed union), conservative management was chosen using a rigid cervical orthosis (Miami J®, Ossur ehf., Reykjavik, Iceland) and serial imaging follow-up. At 1 year, flexion-extension computed tomography demonstrated complete osseous bridging of the C3 facet and C4 body fractures, partial but stable bridging across the C4 facet and lamina and preserved alignment. The patient remained asymptomatic and neurologically intact. This case expands the evidence base for nonoperative management of cervical fractures in adult osteopetrosis beyond C1-C2 patterns. It highlights that rigid-collar immobilization, when neurological function and alignment are preserved and vascular injury is excluded, can yield stable union without surgery. Flexion-extension computed tomography provides a practical endpoint, supporting acceptance of stable partial radiographic healing when dynamic stability is maintained.
Keywords: Osteopetrosis; Cervical spine fracture; Conservative management; Rigid cervical collar; Computed tomography
| Introduction | ▴Top |
Osteopetrosis is an osteoclast failure disorder marked by diffuse skeletal sclerosis and paradoxical fragility. In the cervical spine, dense brittle cortex, scant cancellous bone, and delayed remodeling complicate both fracture biology and fixation, increasing risks of instrumentation failure and nonunion. Adult reports largely cluster into 1) unstable C1-C2 patterns (type II odontoid, chronic hangman’s) treated with fusion and prolonged external immobilization; and 2) stable injuries treated nonoperatively with immobilization. Guidance for conservative management in adults, particularly for multilevel mid-cervical with ligamentous injury, minor cord signal, and transverse-foramen involvement but intact neurology, is sparse.
We present an adult with osteopetrosis and multilevel mid-cervical trauma who was managed nonoperatively in a rigid collar, with longitudinal imaging confirming osseous bridging and stable alignment. This case delineates practical selection criteria (intact neurology, acceptable alignment, negative vascular imaging) and a surveillance template (serial (computed tomography) CT, including flexion-extension), extending successful conservative care beyond C1-C2 pathology and informing decision-making when operative fixation carries high risk.
| Case Report | ▴Top |
Initial presentation
A 22-year-old male with a significant history of osteopetrosis presented to the emergency department as a trauma patient. He had been involved in a high-velocity motor vehicle collision after losing control of his vehicle while intoxicated.
With regards to his osteopetrosis, it had been previously characterized by diffuse skeletal sclerosis, H-shaped vertebrae, and prior posterior-element fractures at T12-L1. Genetic testing was performed to clarify the underlying subtype. Prior, mutation analysis of the CLCN7, TCIRG1, and OSTM1 genes - each associated with distinct forms of osteopetrosis - was conducted at the Connective Tissue Gene Tests Laboratory (Allentown, Pennsylvania, USA). No pathogenic variants were detected in any of these genes. The absence of detectable mutations may reflect a variant in an untested region or another gene yet to be identified. No congenital segmentation anomalies or other metabolic bone diseases were present.
Physical examination
Upon initial and subsequent examinations, the patient was consistently found to be neurologically intact. He had intact cranial nerves and demonstrated full 5/5 motor strength in all four extremities, had normal sensation, despite the severity of his injuries found on imaging.
Investigations and diagnosis
A comprehensive diagnostic workup revealed multiple severe injuries to the cervical spine.
CT identified a displaced fracture of the posterior C4 vertebral body and a complex fracture of the left C4 lateral mass (involving the pedicle, lamina, transverse foramen, and both articular facets). It also showed nondisplaced fractures of the left C6 pedicle and the left C3 inferior facet (Fig. 1).
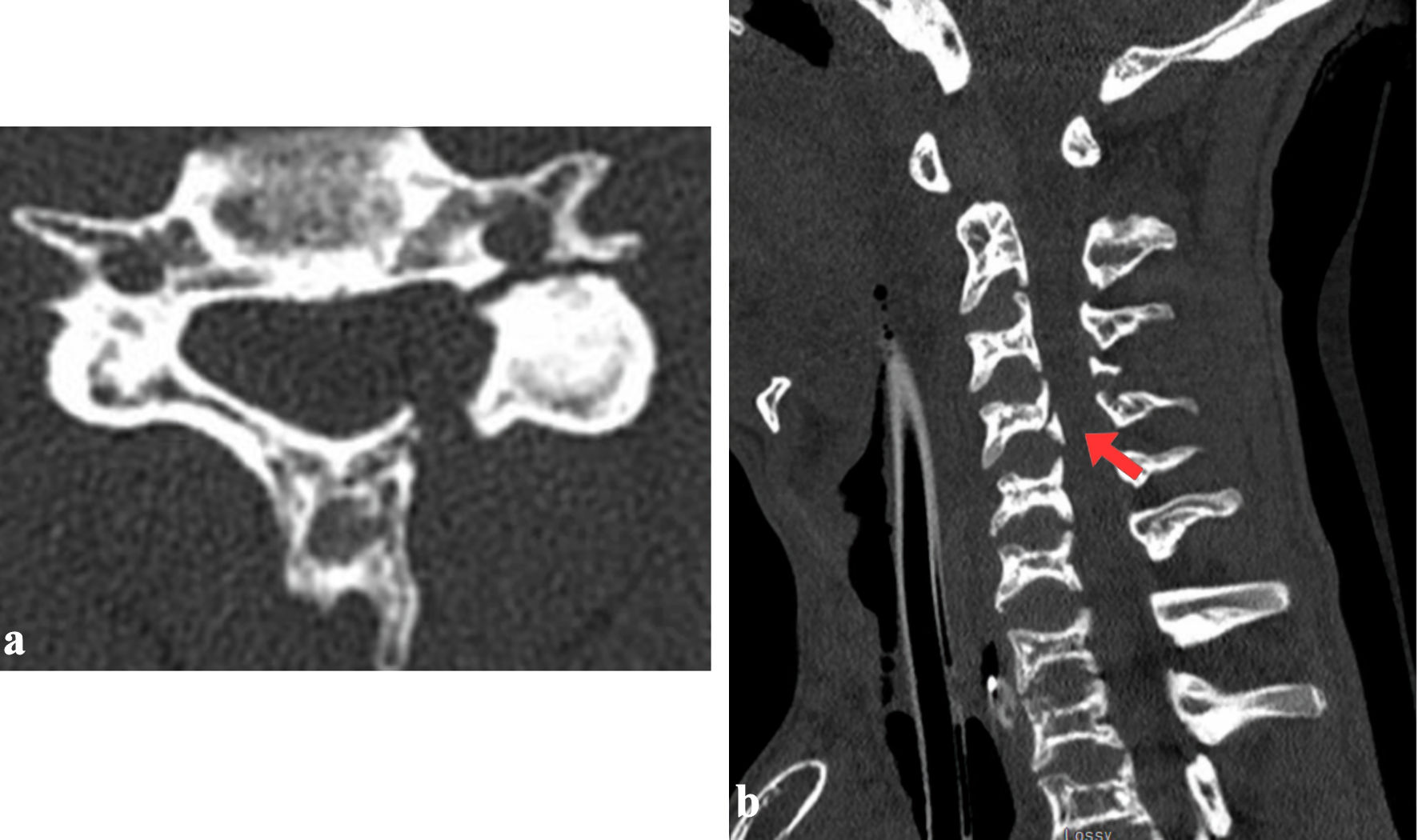 Click for large image | Figure 1. Axial (a) and sagittal (b) views of C4 vertebral body showing displaced fracture involving the posterior aspect of the C4 vertebral body and left lateral mass of C4, with involvement of the pedicle, lamina, transverse foramen and the superior and inferior articular facets. A nondisplaced fracture of the left inferior articular facet of C4 (red arrow) and pedicle of C6 (not shown) is also present. |
Magnetic resonance imaging (MRI) confirmed a spinal cord contusion at the C3-4 level, evidenced by a focal T2-hyperintense signal. It also revealed significant ligamentous injury, including damage to the posterior longitudinal ligament at C4, attenuation of the ligamentum flavum at C3-4, traumatic widening of the left C3-4 facet joint, and a small C4-5 epidural hematoma (Fig. 2).
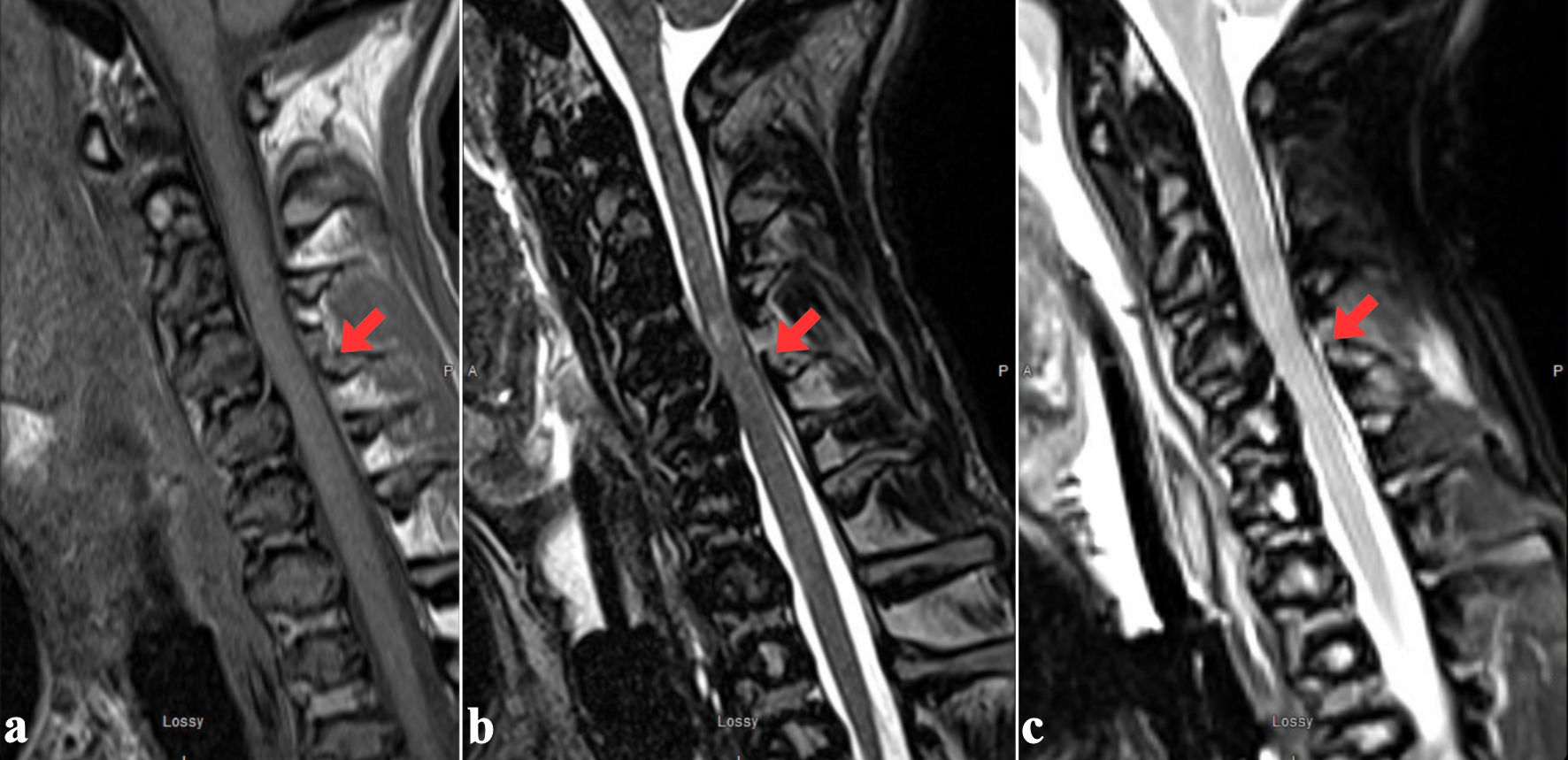 Click for large image | Figure 2. T1- (a), T2- (b) and STIR-weighted (c) magnetic resonance (MR) images showing mild spinal cord edema at the C3-C4 level and the left ventral aspect of the cord with thin posterior epidural hematoma. Posterior longitudinal ligament injury is seen at C4, with suspected ligamentum flavum injury at C3-C4. Interspinous ligamentous injury extends from C3 to C6 with left facet capsular injury from C3-C4 and C4-C5 (red arrows). STIR: short tau inversion recovery. |
Treatment
Given the patient’s stable neurological status and the biological risks of fixation in osteopetrotic bone, a nonoperative management strategy was adopted. While a halo vest was initially entertained, he had declined halo fixation due to personal preferences. He was immobilized in a rigid cervical orthosis (Miami J® collar) and monitored with serial imaging.
Follow-up and outcomes
At a follow-up approximately 3 months post-injury, he remained asymptomatic with stable cervical alignment. A final dynamic flexion-extension CT of the cervical spine performed 1 year post-injury showed interval healing, with complete bone fusion of the C3 and C4 body fractures but incomplete fusion of the C4 facet and lamina (Figs. 3, 4). Alignment was stable in flexion and in extension. At his final clinical assessment, the patient remained pain-free, maintained full neurological function, and was subsequently discharged from routine neurosurgical care.
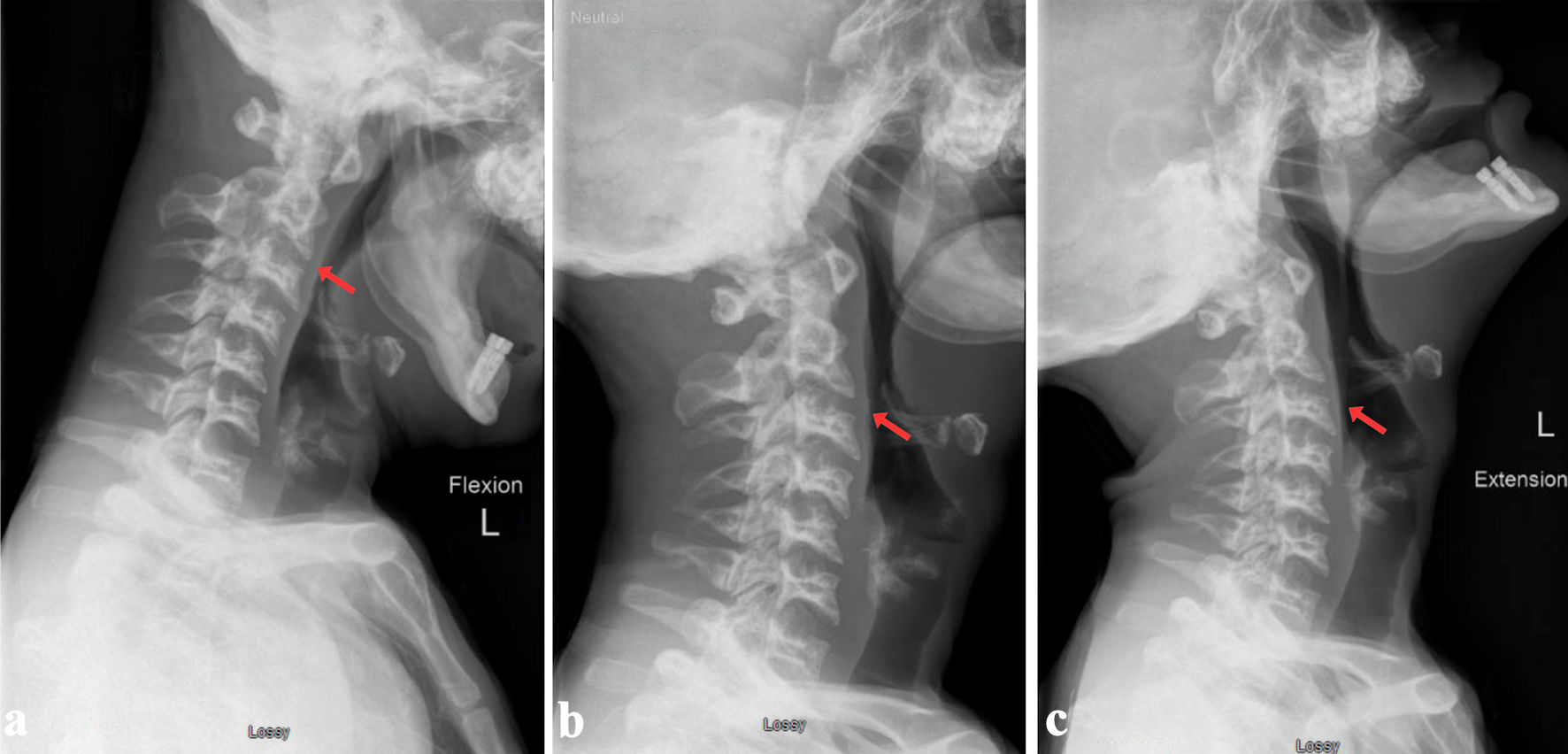 Click for large image | Figure 3. Radiographic follow-up at 1 year showing flexion (a), neutral (b) and extension (c) positions with no dynamic instability (red arrows). |
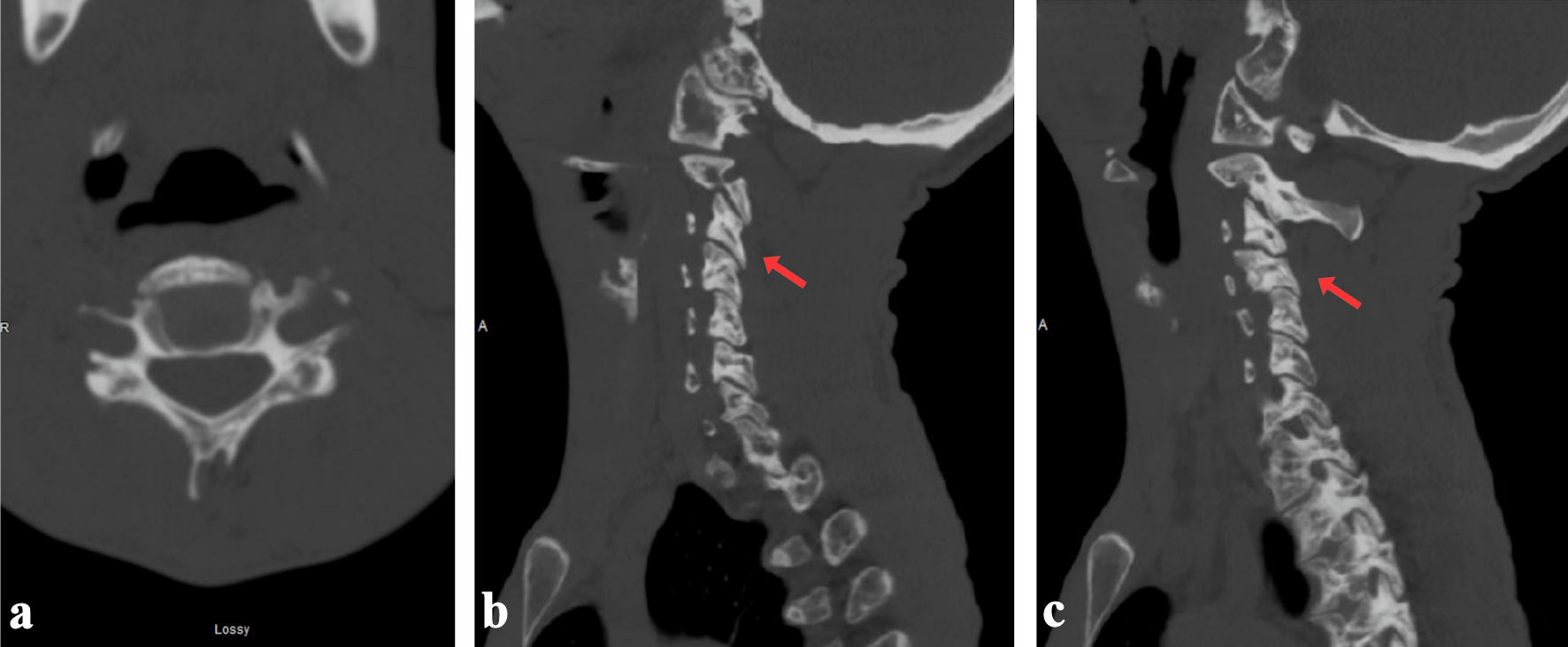 Click for large image | Figure 4. Final CT at 1-year follow-up demonstrating healed C4 fracture and lateral mass alignment in axial view (a), right (a) and left (c) side (red arrows). CT: computed tomography. |
| Discussion | ▴Top |
Adult cervical involvement in osteopetrosis is rare and the literature is limited to case reports describing both conservative and operative strategies dictated by fracture stability and neurological status. Our literature review identified five adult cases of cervical osteopetrosis published between 1984 and 2025 [1-5] (Table 1), with patient ages ranging from 21 to 76 years and a sex distribution of three females to two males. Search terms used on PubMed to retrieve results can be found here (Supplementary Material 1, jmc.elmerpub.com).
 Click to view | Table 1. Summary of Management of All Cervical Fractures in Adults With Osteopetrosis Found in the Systematic Literature Search, Including the Present Case |
Two cases reported conservative management. Ahmadpour et al reported a 55-year-old woman with multilevel traumatic cervical injuries (C1 anterior arch plus C3-C6 pedicle fractures with a comminuted C5 body fracture) managed with external halo immobilization. At 4-year follow-up, she was pain-free, with CT showing stable alignment and sclerosis along prior fracture margins [1]. Ishihama et al described a 63-year-old man who developed a spontaneous C1 anterior arch fracture 1 week after C1 and C4-6 laminectomies for osteopetrosis-related stenosis; with an intact transverse ligament and no instability, he was treated in a Philadelphia collar, evolving to painless nonunion at 5 years without further intervention [3]. Together, these cases support nonoperative care when neurology is intact and dynamic stability is preserved.
With regards to surgical management, Auerbach et al treated a 21-year-old woman with a subacute, unstable type II odontoid fracture with C1-C2 instability using posterior C1-2 transarticular screws with interspinous wiring and iliac-crest autograft. At 2-year follow-up, she had a solid arthrodesis with only mild motion loss, underscoring the need for rigid constructs in sclerotic bone [2]. Yamane et al reported a 76-year-old woman with chronic unstable type II hangman’s fracture managed by anterior C2-3 interbody fusion and plating; despite technical difficulties inherent to dense, brittle bone, radiographic union was achieved by 1 year [5]. Sabacinski et al presented a 27-year-old patient with osteopetrosis and central cord syndrome, without fracture, who underwent C3-7 laminoplasty, with stable hardware on follow-up, illustrating that decompression is feasible when indicated for myelopathy in this population [4].
Across reports, stable injuries can be managed nonoperatively with external immobilization (halo or collar), whereas mechanically unstable patterns (e.g., type II odontoid, chronic hangman’s) are typically treated with fusion using the stiffest construct safely achievable. Decompression is reserved for myelopathic presentations without fracture.
In this young adult with osteopetrosis, we chose rigid-collar-only management despite radiographic features that would typically meet thresholds for operative stabilization in normal bone. Imaging showed a displaced posterior-inferior C4 body fracture with left C4 lateral-mass involvement (pedicle, lamina, both facets, and transverse foramen), additional fractures at C3 (inferior facet) and C6 (pedicle), and soft-tissue injury on MRI - cord T2 signal, posterior longitudinal ligament injury, ligamentum flavum attenuation, facet widening, and a small epidural hematoma. In a non-osteopetrotic patient, this constellation (bony displacement plus ligamentous disruption and cord signal) would commonly prompt instrumented stabilization. Here, the surgical calculus was different: dense, brittle cortex raised the risks of poor screw purchase, iatrogenic fracture, thermal injury, and pseudoarthrosis; graft harvest/incorporation was uncertain; and achieving stability might have required multilevel fixation with real potential for hardware/graft failure and early revision with extended long fusion. In a young adult, the morbidity of a long fusion (loss of motion segments, potential adjacent-level fractures, and high reoperation risk) outweighed its theoretical benefits. Given intact neurology, acceptable alignment, and negative vascular imaging despite foraminal breach, we elected conservative care with predefined imaging milestones. At approximately 1-year follow-up, flexion-extension CT demonstrated complete bridging (C3 facet; posterior-inferior C4 body) and partial but stable bridging (C4 facet/lamina) with no dynamic instability. The strategy therefore prioritized avoiding high-risk fixation at present, accepting stable partial radiographic healing in sclerotic bone, and reserving surgery for clear triggers (progressive translation/kyphosis, painful nonunion, or new neurologic deficit).
Anatomically, this case extends the spectrum beyond C1-C2. A mid-cervical pattern involving a C4 body component and lateral mass injuries was successfully treated nonoperatively, complementing reports where odontoid or hangman’s lesions required fusion.
Conclusions
In adult osteopetrosis, select multilevel mid-cervical fractures can be safely managed with rigid collar alone when neurology is intact, alignment is acceptable, and vascular imaging is negative despite the presence of soft-tissue injury (cord T2 signal, posterior longitudinal ligament injury, ligamentum flavum attenuation). Flexion-extension CT provides practical endpoints: accept stable partial radiographic healing if dynamic stability is preserved. This case broadens successful conservative management beyond C1-C2 patterns and offers a simple selection-and-surveillance template for surgeons when operative fixation risks are high.
Learning points
This case illustrates that rigid-collar immobilization alone can succeed for select multilevel mid-cervical fractures in adult osteopetrosis when neurological function and alignment are preserved. Conservative care should be reserved for reliable patients with intact neurology, acceptable dynamic stability, and negative vascular imaging despite transverse-foramen involvement. Limited cord signal or ligamentous injury on MRI need not mandate surgery if alignment remains stable. Flexion-extension CT can provide practical confirmation of dynamic stability and acceptable partial radiographic healing.
| Supplementary Material | ▴Top |
Suppl 1. Keywords used for PubMed search.
Acknowledgments
None to declare.
Financial Disclosure
No funding was received for this work.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Informed consent was obtained from the patient.
Author Contributions
Dr. Abdul Haseeb Naeem was responsible for managing the surgical case and performing the surgery as well as supervising the write up of this case report and guiding the systematic review. Hamza Mahdi was responsible for the write up of the case report as well as performing and writing up the systematic review.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Ahmadpour A, Goodarzi A, Lee DJ, Panchal RR, Kim KD. Cervical spine fractures in osteopetrosis: a case report and review of the literature. J Biomed Res. 2018;32(1):68-76.
doi pubmed - Auerbach JD, McCormick FL, Mehta S, Brummett RS, Rushton SA. Posterior cervical arthrodesis for subacute odontoid fracture in a patient with osteopetrosis: case report. Spine (Phila Pa 1976). 2007;32(1):E34-38.
doi pubmed - Ishihama Y, Ikeda T, Iemura S, Toriumi K, Goto K. Spontaneous anterior arch fracture of the atlas following C1 laminectomy in a patient with osteopetrosis: a case with five years of follow-up. Cureus. 2025;17(2):e79471.
doi pubmed - Sabacinski K, Booth M, Bramer M. Managing osteopetrosis in the complex polytrauma orthopedic patient. Cureus. 2022;14(2):e21886.
doi pubmed - Yamane K, Kai N. Anterior cervical arthrodesis for chronic hangman's fracture in a patient with osteopetrosis: a case report. Arch Orthop Trauma Surg. 2018;138(6):783-789.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.