| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 9, September 2025, pages 387-391
Life-Threatening Calcium Chloride Ingestion
Ki-Kwan Kanga, Hyoung-Jong Kima, Dong-Yoon Kimb, Nam-Seon Beckc, Sang-Sin Jund, Eun-Mi June, Joung-Il Imf, Sae-Yong Hongg, h
aDepartment of Emergency Medicine, Chung-Ang Jeil Hospital, Chungbuk, South Korea
bDepartment of Chemistry and Biochemistry, UCLA, Los Angeles, CA, USA
cDepartment of Pediatrics, Chung-Ang Jeil Hospital, Chungbuk, South Korea
dDepartment of Neurology, Chung-Ang Jeil Hospital, Chungbuk, South Korea
eDepartment of Nursing, Chung-Ang Jeil Hospital, Chungbuk, South Korea
fDepartment of Orthopedic Surgery, Chung-Ang Jeil Hospital, Chungbuk, South Korea
gDepartment of Nephrology, Chung-Ang Jeil Hospital, Chungbuk, South Korea
hCorresponding Author: Sae-Yong Hong, Department of Nephrology, Jincheon Joongang Jeil General Hospital, Chungbuk 27832, South Korea
Manuscript submitted August 6, 2025, accepted September 9, 2025, published online September 17, 2025
Short title: Calcium Chloride Ingestion
doi: https://doi.org/10.14740/jmc5183
| Abstract | ▴Top |
Calcium chloride dihydrate (CaCl2·2H2O), a common component in household dehumidifiers in South Korea, poses a significant risk of toxicity upon ingestion. We present a case of life-threatening hypercalcemia following intentional calcium chloride dihydrate ingestion, with a focus on electrolyte homeostasis and physiological adaptation. An 86-year-old Korean woman presented with transient unconsciousness after ingesting dehumidifier fluid. She exhibited drowsiness and developed sinus tachycardia 10 h later. Severe hypercalcemia (19.4 mg/dL) was the main biochemical disturbance. Parathyroid hormone was initially suppressed but later rose, facilitating renal calcium excretion and phosphorus regulation. Electrolyte levels normalized by day 4. Prompt treatment, including gastric lavage and cardiac management, led to a full recovery. A rapid parathyroid hormone response played a crucial role in restoring calcium balance.
Keywords: Calcium chloride dihydrate; Hypercalcemia; Dehumidifiers; Deliberate ingestion; Parathyroid hormone
| Introduction | ▴Top |
Exposure to common household or industrial chemicals, whether accidental or intentional, poses a significant risk to human health [1]. Calcium chloride (CaCl2) is a chemical with diverse applications, including de-icing, construction, and food production [1]. In South Korea, it is also widely used as a dehumidifying agent in consumer products to mitigate humidity-related problems in closed environments. These dehumidifiers contain pure CaCl2·2H2O, in concentrations ranging from 50% to 75%, and are readily available without regulatory restrictions, making them a common household item. This accessibility, however, carries a significant risk, particularly in the case of intentional ingestion, such as suicide attempts.
While isolated cases of calcium chloride poisoning have been reported, most of the existing literature focuses on localized organ damage, including gastric necrosis, metabolic acidosis, and cardiovascular complications [2-4].
This case report presents a detailed analysis of a case of severe CaCl2 intoxication, with a unique focus on the in-hospital course and its impact on systemic electrolyte homeostasis, including calcium, phosphorus, and parathyroid hormone. This case provides a rare observation of the physiological adaptation of the endocrine and renal systems to an acute, severe hypercalcemic state, offering a perspective not typically documented in previous reports.
| Case Report | ▴Top |
Investigations
This case report protocol was reviewed and approved by the Public Institutional Review Board of the Ministry of Health and Welfare of South Korea (approval no. P01-202501-01-027) [5].
In late October 2024, an 86-year-old Korean female (height, 158 cm; weight, 55 kg) was presented to the emergency department of our hospital with a primary complaint of altered consciousness after an intentional ingestion of a few hundred milliliters of liquid dehumidifier. The patient’s family reported that the patient had ingested the liquid approximately 1 h before arrival at the hospital in a deliberate attempt to commit suicide.
Upon arrival, her vital signs were as follows: blood pressure 175/95 mm Hg, heart rate (HR) 60 bpm, and temperature 35.5 °C. She was lethargic, with no focal neurological signs, and pica behavior was not noted in her personal history.
Diagnosis
Laboratory findings at the time of arrival (approximately 2 h post ingestion) are shown in Table 1.
 Click to view | Table 1. Initial Laboratory Findings |
Electrolytes were measured using an autoanalyzer (Beckman Coulter AU 689; Tokyo, Japan), and serum calcium levels were specifically assayed using the Arsenazo III method.
Chest computed tomography revealed no specific abnormalities in the lungs, pleura, or chest wall. The primary clinical manifestation upon admission was drowsiness, and the Glasgow Coma Scale score [6] decreased from 9 on hospital day 1 to 8 on hospital day 2 but subsequently improved to 13 - 14 by hospital day 4. Similarly, the Medical Research Council Muscle Strength Grading Scale score [7] declined from 5 to 3 during the first 3 days, followed by a steady recovery.
Electrocardiography revealed a normal sinus rhythm with intermittent premature ventricular beats, a QRS duration of 106 ms, and flat T waves in all leads, accompanied by a shortened QT interval (QTc = 395 ms), but without J waves. Over the next 10 h, the patient’s heart rate spiked, from 60 beats/min upon admission to 130 beats/min, and a repeat electrocardiography revealed sinus tachycardia with a further shortened QTc interval (375 ms) but no changes in the QRS complex.
Sequential changes in serum calcium, phosphorus, intact parathyroid hormone, and renal excretion of calcium and phosphorus during the observation period are shown in Figure 1. The combination of severe hypercalcemia and hyperphosphatemia during the early admission period suggests a dual effect: cellular release of phosphorus due to hypercalcemia-induced cellular damage [8] and reduced renal phosphate excretion resulting from suppressed parathyroid hormone. This hypothesis is supported by elevated lactate dehydrogenase level on hospital day 2 (349 U/L; reference 140 - 271).
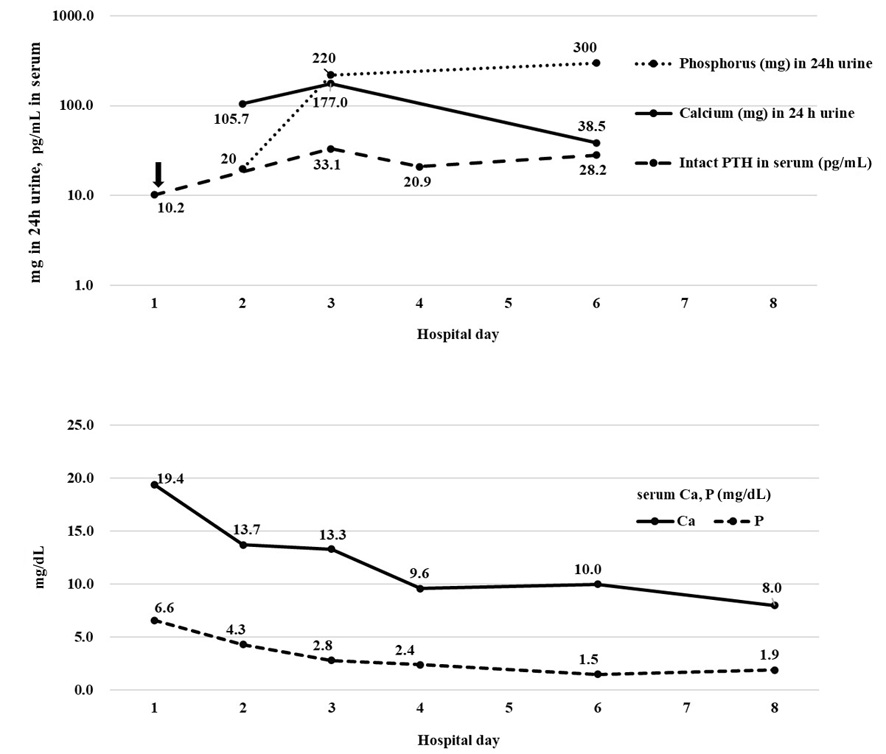 Click for large image | Figure 1. Sequential measurement of (upper; Y-axis is a logarithmic scale) serum levels of intact parathyroid hormone (pg/mL) and 24-h urine calcium and phosphorus (mg in 24-h urine), and (lower) serum calcium and phosphorus (mg/dL). Notably, the initial parathyroid hormone level, indicated by the downward arrow, was much lower than the levels measured after recovery. This result suggests that parathyroid hormone levels decreased immediately after CaCl2 ingestion, accompanied by increased renal calcium and decreased renal phosphorus excretion. In parallel, serum calcium and phosphorus levels gradually normalized by the fourth day of hospitalization. The normal reference ranges were as follows: 24-h urine phosphorus < 250 mg (females), 24-h urine calcium 400 - 1,300 mg, and serum intact parathyroid hormone 15 - 65 pg/mL. Reference values for serum calcium and phosphorus are shown in Table 1. Creatinine clearance, measured by 24 h urine on day 2, 3, and 6, was 41.7, 37.5, and 46.7 mL/min, respectively. |
Ionized calcium levels were also elevated at 6.1, 6.5, and 5.3 mg/dL on hospital days 1, 4, and 6, respectively (reference range: 4.0 - 5.6 mg/dL). Magnesium levels remained within the normal range (1.80 - 2.60 mg/dL) during the observation period.
Blood gas analysis on hospital day 1 was compatible with metabolic acidosis, a finding inconsistent with calcium-alkali syndrome.
Treatment
Given the early presentation to the emergency department, approximately 1 h after ingestion, a gastric lavage was performed using a large-bore orogastric tube (28 Fr, 9.3 mm).
The most striking electrolyte abnormality on admission was severe hypercalcemia, with a serum calcium level of 19.4 mg/dL. Extensive parenteral hydration was initiated using 2 L of normal saline. The patient’s tachycardia was treated with adenosine and diltiazem, with the heart rate normalized to 60 - 70 beats/min within 48 h.
Follow-up and outcomes
By hospital day 10, the patient reported feeling as healthy as before the ingestion of CaCl2 and was discharged. A 3-month follow-up phone call revealed that she was recovering well, with the main issue being back pain.
| Discussion | ▴Top |
This case provides a detailed, sequential account of the physiological response to life-threatening hypercalcemia from acute CaCl2 ingestion. Unlike other case reports [2-4] that focus primarily on the corrosive and necrotic effects of this chemical, our report highlights the remarkable and rapid hormonal and renal adaptations that can facilitate homeostatic recovery.
The central observation of this case is the dynamic interplay between the parathyroid gland, serum electrolytes, and renal function, as visually demonstrated in Figure 1.
Upon admission, the patient’s severely elevated serum calcium (19.4 mg/dL) led to the expected suppression of parathyroid hormone, which was initially measured at a low level (10.2 pg/mL). As the systemic calcium load began to decrease following treatment, a compensatory rise in parathyroid hormone was observed, peaking at 33.1 pg/mL on hospital day 3. This hormonal response triggered enhanced renal excretion of calcium and suppressed renal excretion of phosphorus. The 24-h urine collection data clearly show this process: urinary calcium levels increased significantly from 105.7 to 177.0 mg and then decreased to 38.5 mg, while urinary phosphorus levels dropped to a nadir of 20.0 mg on hospital day 3 before rising to 300.0 mg by hospital day 6. This synchronized physiological response, even in an elderly patient with diminished physiological reserve, was highly efficient, allowing for the normalization of serum calcium and phosphorus levels by hospital day 4. This finding is significant as it demonstrates that a robust endocrine-renal axis, even in advanced age, can effectively manage an acute, severe calcium overload.
The patient’s relatively benign clinical course, despite the ingestion of an estimated 300 g of CaCl2, which far exceeds the reported lethal dose (LD50) in rats (1,000 - 1,400 mg/kg orally, European Chemicals Agency, Registration Dossier for Calcium Chloride; CAS No. 10043-52-4 [9]), is a crucial point of discussion.
Several factors contributed to this outcome. First, the patient’s early presentation to the hospital, within 1 h of ingestion, allowed for prompt gastric lavage, which limited the systemic absorption of the CaCl2. Second, the patient’s surprisingly efficient hormonal and renal response was instrumental in clearing the remaining calcium from the system within a few days.
Gastric lavage is a contentious procedure in toxicology [10-12], but its role in the management of this patient warrants discussion. Gastrointestinal decontamination is a crucial intervention in South Korea, where a considerable number of patients are affected by acute chemical intoxication from suicide attempts [13] and specific antidotes are often unavailable.
In this case, the liquid nature of the ingested solution may have made it more easily removable by the large-bore orogastric tube used. The favorable clinical outcome that followed the procedure raises the possibility that gastric lavage may be beneficial in highly selected cases with early presentation. This case illustrates the need for context-specific clinical decision-making and underscores the importance of conducting further controlled studies to clarify the role of gastric decontamination in various types of intoxication.
In addition to the endocrine and renal responses, the patient’s initial laboratory results suggest a significant systemic reaction to the chemical ingestion. The complete blood count upon admission revealed an elevated white blood cell count (18,540/µL) and neutrophil count (80.9%) that were both well above the normal reference range (Table 1). This finding, which is often a secondary consideration in electrolyte disturbances, indicates a generalized inflammatory response, likely triggered by localized gastric mucosal injury from the concentrated CaCl2 solution. This inflammatory cascade would also contribute to the cellular damage that led to the release of cellular phosphorus, causing the initial hyperphosphatemia.
The primary limitation of this case report is that it reflects the findings of a single elderly patient, and further case studies are needed to confirm the observed physiological responses and treatment effects. Additionally, vitamin D levels were not measured during the patient’s hospitalization. Despite these limitations, the detailed, real-time documentation of the patient’s hormonal and renal adaptations makes this report a valuable contribution to the sparse literature on this topic.
Learning points
The primary “take-away” lesson from this case report: Ingestion of calcium chloride-containing liquid from a dehumidifier can cause life-threatening hypercalcemia. In this case of deliberate ingestion, unconsciousness developed, and severe hypercalcemia, peaking at 19.4 mg/dL, led to suppressed parathyroid hormone level that facilitates rapid renal calcium excretion and phosphorus regulation.
Early gastric lavage and aggressive medical management contributed to the patient’s survival. A robust parathyroid hormone response, even in an elderly patient, may be crucial for survival in acute CaCl2 toxicity when renal and endocrine systems are intact.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare that they have no competing interests.
Informed Consent
Written informed consent was obtained from the patient.
Author Contributions
Conceptualization: SH and DK; data curation: KK and HK; formal analysis: SH; funding acquisition: JI; investigation: SH, NB, and SJ; methodology: SH; supervision: JI; validation: SH; visualization: EJ; writing - original draft: SH; writing - review and editing: SH. All authors read and approved of the final manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Tinwell H, Colombel S, Blanck O, Bars R. The screening of everyday life chemicals in validated assays targeting the pituitary-gonadal axis. Regul Toxicol Pharmacol. 2013;66(2):184-196.
doi pubmed - Nakagawa Y, Maeda A, Takahashi T, Kaneoka Y. Gastric necrosis because of ingestion of calcium chloride. ACG Case Rep J. 2020;7(8):e00446.
doi pubmed - Cho K, Seo B, Koh H, Yang H. Fatal case of commercial moisture absorber ingestion. BMJ Case Rep. 2018;2018:bcr-2018-225121.
doi pubmed - Shin SJ, Kim YJ. Cardiac manifestations after ingestion of a commercial desiccant: a case report. Medicina (Kaunas). 2023;60(1).
doi pubmed - http://irb.or.kr/menu02/summary.aspx
- Shaywitz BA. Management of acute neurologic syndromes in infants and children. Yale J Biol Med. 1984;57(1):83-95.
pubmed - Amidei C. Measurement of physiologic responses to mobilisation in critically ill adults. Intensive Crit Care Nurs. 2012;28(2):58-72.
doi pubmed - Dong Z, Saikumar P, Weinberg JM, Venkatachalam MA. Calcium in cell injury and death. Annu Rev Pathol. 2006;1:405-434.
doi pubmed - https://echa.europa.eu/registration-dossier/-/registered-dossier/15461/7/3/2
- Vale JA. Position statement: gastric lavage. American Academy of Clinical Toxicology; European Association of Poisons Centres and Clinical Toxicologists. J Toxicol Clin Toxicol. 1997;35(7):711-719.
doi pubmed - Caravati EM, Megarbane B. Update of position papers on gastrointestinal decontamination for acute overdose. Clin Toxicol (Phila). 2013;51(3):127.
doi pubmed - Liskow DS, Pinson RDP. Gastric lavage in the management of acute poisoning: a meta-analysis. Journal of Emergency Medicine. 2001;21(2):129-136.
- Lee JW, Hwang IW, Kim JW, Moon HJ, Kim KH, Park S, Gil HW, et al. Common pesticides used in suicide attempts following the 2012 paraquat ban in Korea. J Korean Med Sci. 2015;30(10):1517-1521.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.