| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 9, September 2025, pages 381-386
A Forty-Three-Year-Old Male With Penile and Cavernous Metastases From Rectal Cancer
Dina Quannouni El Moumouhia, b, Ignacio Calleja Durana, Jose Emilio Hernandez Sancheza
aDepartment of Urology, Hospital Universitario General de Villalba, Collado Villalba, Madrid, Spain
bCorresponding Author: Dina Quannouni El Moumouhi, Department of Urology, Hospital Universitario General de Villalba, Collado Villalba, Madrid, Spain
Manuscript submitted August 5, 2025, accepted August 25, 2025, published online September 17, 2025
Short title: A Case of Penile and Cavernous Metastases From CRC
doi: https://doi.org/10.14740/jmc5181
| Abstract | ▴Top |
Metastasis to the cavernous bodies from colorectal cancer (CRC) is an exceptionally rare condition, typically associated with systemic dissemination and an ominous prognosis. It often presents synchronously with liver and lymph node involvement. A 43-year-old male presented with perineal pain, rectal bleeding, and urinary obstructive symptoms. Imaging studies revealed a KRAS-mutated rectal adenocarcinoma, classified as stage IV, with synchronous metastases to the cavernous bodies and liver. Treatment was initiated with FOLFOXIRI (folinic acid, 5-fluorouracil, oxaliplatin and irinotecan) chemotherapy but was discontinued due to tumor lysis syndrome and toxicity linked to a UGT1A1 mutation. Despite modified FOLFOX (folinic acid, fluorouracil, oxaliplatin) plus bevacizumab, the disease progressed rapidly, prompting transition to palliative care and subsequent death. Cavernous body involvement in CRC reflects advanced disease, frequently accompanied by synchronous metastases and a limited life expectancy. This case underscores the poor prognostic significance of such metastases, suggests pelvic lymphatic spread as a likely mechanism, and highlights the critical impact of pharmacogenetics on treatment tolerance and outcomes. A review of the literature emphasizes the aggressive biology of such presentations. Penile metastases from CRC are rare but devastating, indicating disseminated disease. Multidisciplinary management should prioritize symptom control, with targeted therapies reserved for select cases. This case illustrates the need for heightened clinical suspicion in patients with a history of malignancy presenting with urological symptoms.
Keywords: Penile metastasis; Corpora cavernosa; Rectal cancer; Pharmacogenetics
| Introduction | ▴Top |
Colorectal cancer (CRC) ranks among the most prevalent malignancies worldwide, holding the third position in global incidence [1, 2]. While its most common metastatic sites include the liver, lungs, and peritoneum [3], atypical dissemination sites such as the cavernous bodies - though exceptionally rare - carry an ominous prognosis [1, 3-5]. From the first case reported by Eberth in 1870 [1, 4] to the present day, penile metastases from CRC remain extraordinary findings, with only a handful of cases documented in the medical literature [4]. They typically indicate widespread, aggressive disease and are associated with a very limited survival [5, 6].
This report presents a case of CRC with synchronous penile and liver metastases, analyzing its aggressive clinical course, the diagnostic challenges, and the available therapeutic options. Through a subsequent literature review, we aim to contribute to the understanding of this rare yet devastating complication.
| Case Report | ▴Top |
A 43-year-old male with no significant medical history was referred from the emergency department due to perianal, perineal, and suprapubic pain lasting approximately 1 month, accompanied by recurrent hematochezia. The patient also reported urinary voiding symptoms and noted a testicular lesion causing discomfort during erection.
On physical examination, the patient was afebrile with stable vital signs. No pallor, icterus, or significant peripheral lymphadenopathy was noted. Abdominal examination revealed a soft, non-distended abdomen with no palpable masses or organomegaly; mild suprapubic tenderness was noted on deep palpation. Urogenital examination revealed a circumcised penis with two firm, fixed, and non-tender nodules, each approximately 1.5 cm in diameter, located at the dorsolateral base of the penile shaft. No inguinal hernias or palpable lymphadenopathy were detected.
Initial imaging included a testicular Doppler ultrasound, which showed no pathological findings, and a penile ultrasound that identified multiple solid nodules in both cavernous bodies, highly suggestive of secondary metastatic involvement (Fig. 1). These findings, along with persistent hematochezia, prompted urgent referral for a complete colonoscopy.
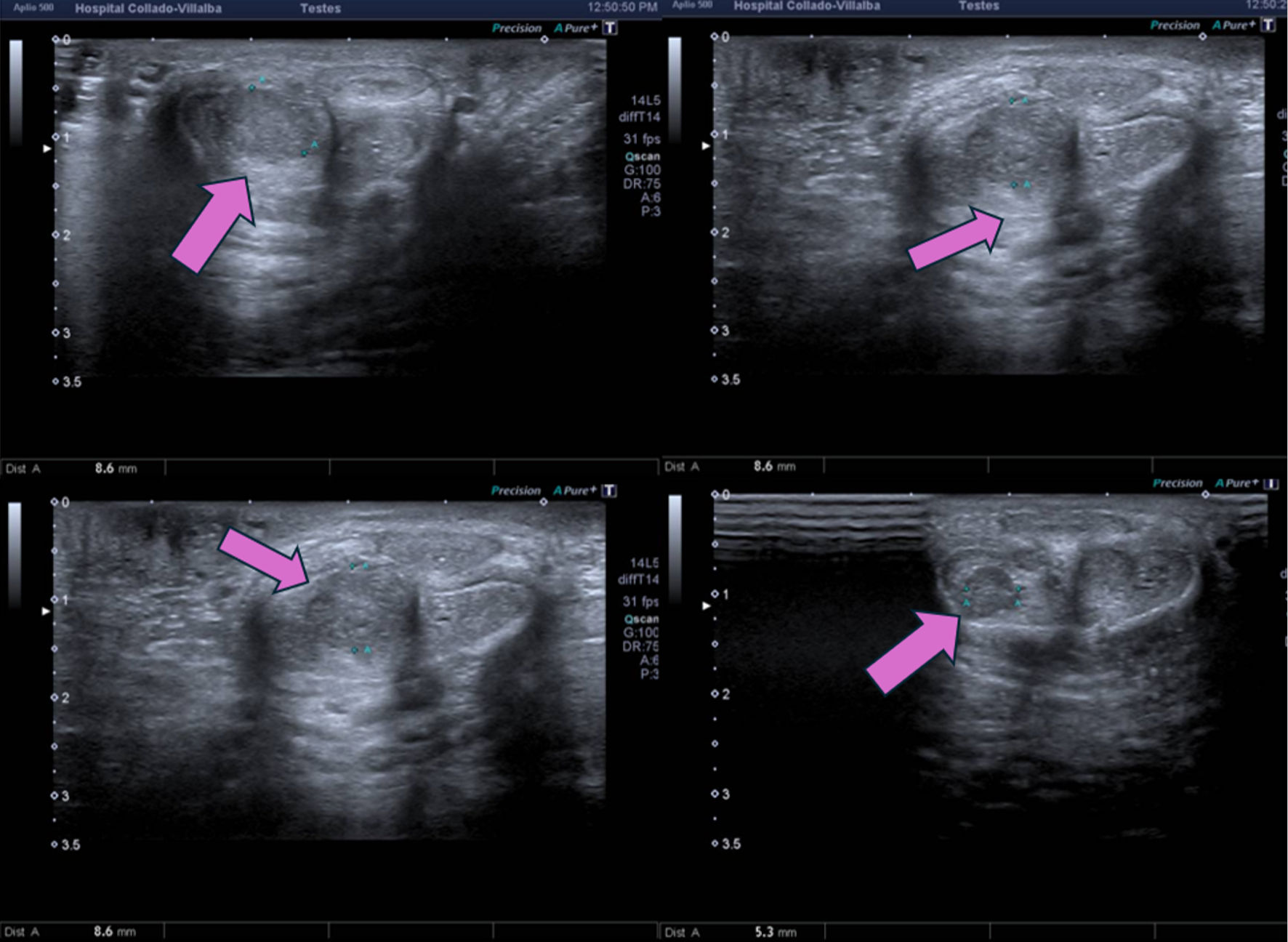 Click for large image | Figure 1. Penile ultrasound showing solid nodules in both corpora cavernosa (arrows), highly suggestive of metastatic involvement. |
Colonoscopy revealed a mamillated mass with degenerative areas in the distal rectum, from which multiple biopsies were taken. Histopathological analysis confirmed infiltrating colorectal adenocarcinoma with a KRAS mutation (exon 2, codon 12, p.G12V) and preserved NRAS and BRAF genes.
Staging with thoraco-abdominopelvic computed tomography (CT) scan demonstrated a lower rectal tumor with locoregional lymphadenopathy and extensive infiltration of adjacent structures, including direct contiguous spread to the pelvic floor muscles and distinct metastatic deposits within the cavernous bodies, predominantly on the right side. Additionally, multiple hepatic metastases were identified in segments VIII, VII (two lesions), VI, and IVb (Fig. 2). A complementary pelvic magnetic resonance imaging (MRI) confirmed these findings, revealing a necrotic rectal lesion and well-defined metastatic masses in the cavernous bodies with right-sided predominance (Fig. 3).
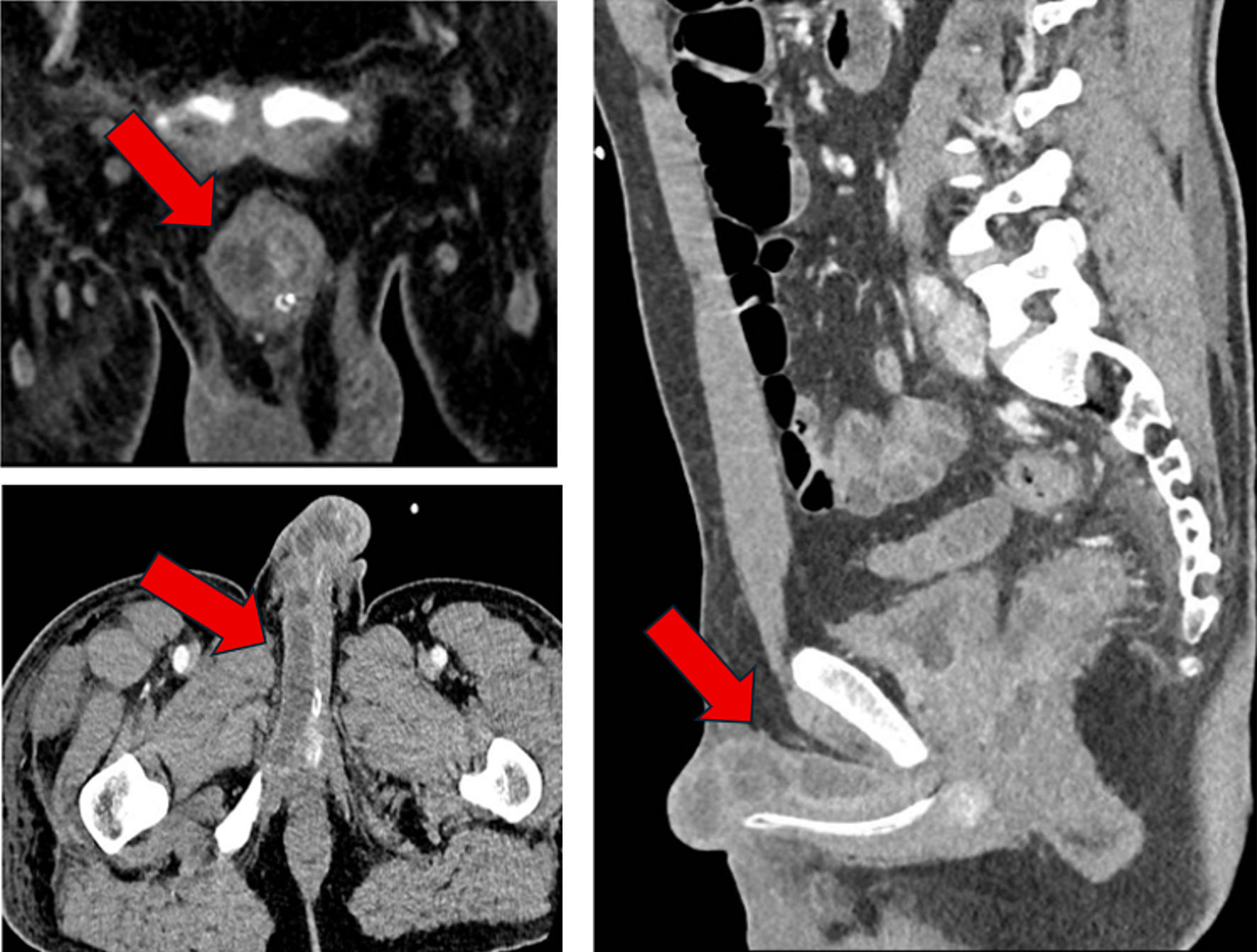 Click for large image | Figure 2. Computed tomography (CT) scan showing diffuse involvement of the corpora cavernosa and pelvic floor musculature, predominantly on the right side (arrows). |
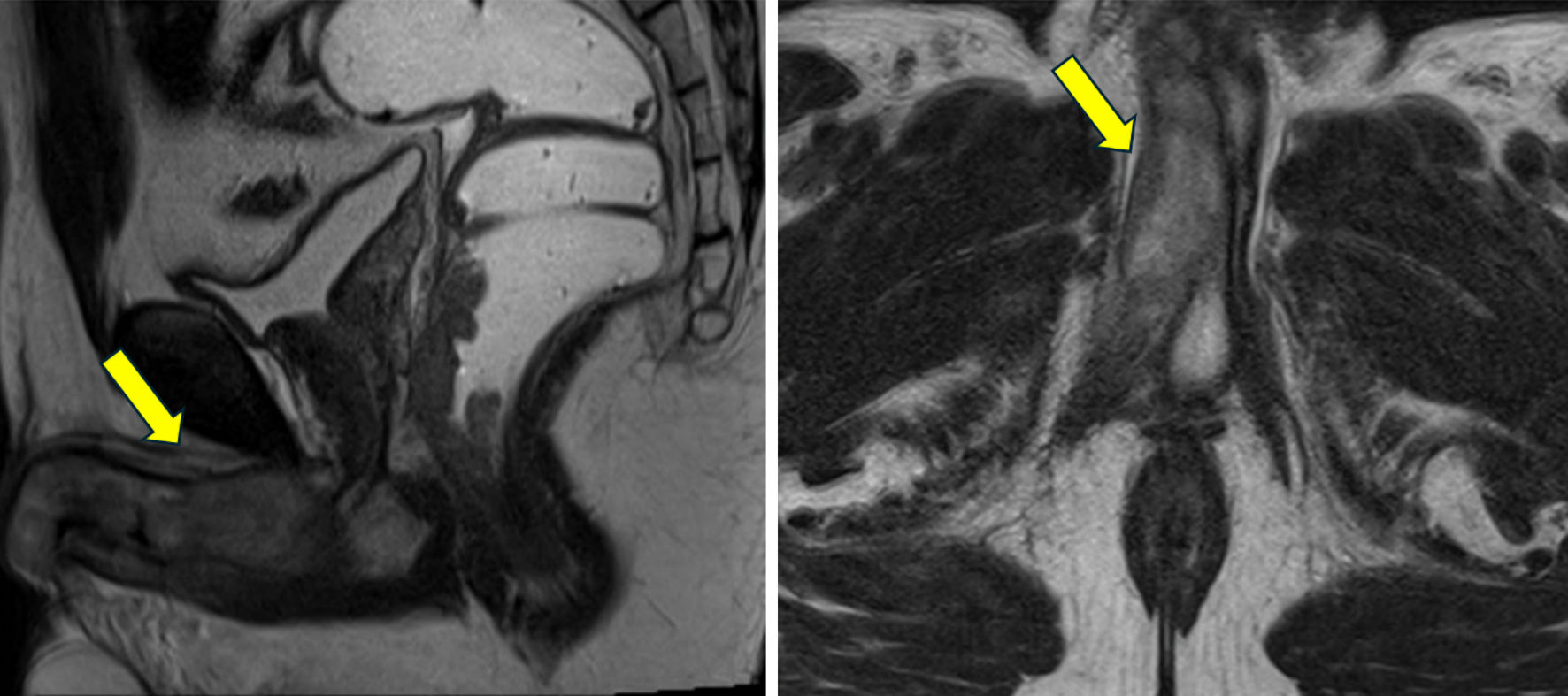 Click for large image | Figure 3. Magnetic resonance imaging (MRI) showing necrotic rectal lesion and well-defined metastatic masses in the corpora cavernosa (arrows). |
Given the diagnosis of stage T4bN2bM1 lower rectal adenocarcinoma with hepatic and penile metastases, systemic treatment with FOLFOXIRI (folinic acid, 5-fluorouracil, oxaliplatin and irinotecan) was initiated. However, the patient exhibited poor tolerance during the first cycle, developing severe neutropenia, febrile neutropenia, and laboratory findings consistent with tumor lysis syndrome (TLS). Subsequent pharmacogenetic testing identified homozygosity for the UGT1A1*28 allele, explaining the extreme sensitivity to irinotecan. This adjusted protocol was better tolerated, and the patient completed five cycles.
Upon completion of chemotherapy, a follow-up CT scan revealed disease progression, including enlargement of the primary rectal mass, new mesorectal lymphadenopathy, and significant growth of hepatic metastases. In light of these findings and the poor prognosis, active oncologic treatment was discontinued, and the patient was referred to the Palliative Care Unit for symptom management and passed away 2 months later, approximately 7 months after initial diagnosis.
| Discussion | ▴Top |
Penile metastases represent a rare manifestation of advanced malignancies, with the majority originating from genitourinary tumors such as prostate, bladder, and kidney. Only approximately 13% of cases derive from CRC, according to recent reviews [1, 2, 4, 5, 7-9]. Our case of rectal adenocarcinoma with synchronous metastases to both the cavernous bodies and liver exemplifies this exceptional yet clinically significant scenario [1, 2, 4, 10].
To better contextualize our findings, we conducted a narrative review of the literature, summarized in Table 1 [1, 2-4, 6, 7, 9-11]. Analysis of 10 reported cases from 1961 to the present [1-4, 6, 7, 9-11] reveals a consistent profile: this complication predominantly affects older individuals (mean age 64 years) and shows a strong predilection for primary tumors located in the rectum (90% of cases). The disease is overwhelmingly systemic at diagnosis, with 60% of cases presenting synchronously with metastases to other sites, most commonly the liver and lungs. The prognosis is invariably poor, with a median survival of less than 6 months from the diagnosis of penile involvement, despite heterogeneous treatment approaches [2, 4]. However, isolated cases of late-onset metastases appearing months or even years after treatment of the primary tumor have been documented [3, 11].
 Click to view | Table 1. Summary of Selected Reported Cases of Penile Metastasis From Colorectal Cancer |
Our patient’s presentation aligns with this literature, confirming the association with synchronous metastases and a rapidly fatal outcome. However, several aspects of this case provide novel and instructive insights. At 43, our patient was significantly younger than the typical demographic, suggesting that underlying aggressive tumor biology can override conventional age-related risk factors. This is further evidenced by the development of TLS, an exceptional event in solid tumors that highlights an extreme proliferative rate and tumor burden.
The radiological pattern of dissemination, featuring extensive locoregional lymph node involvement (N2b) alongside discrete cavernous nodules and hepatic metastases, strongly suggests retrograde lymphatic spread as the primary mechanism for penile involvement [6], concurrent with hematogenous portal dissemination to the liver.
A paramount learning point is the essential role of pre-emptive pharmacogenetic screening. The identification of a homozygous UGT1A1*28 genotype in our patient provides a clear molecular explanation for the life-threatening toxicity (febrile neutropenia, TLS) to first-line FOLFOXIRI [12]. This underscores the necessity of integrating such testing into clinical practice to guide personalized therapy selection in advanced CRC, thereby avoiding severe toxicity and optimizing the safety of palliative treatment.
Therapeutic management for penile metastases remains predominantly palliative, focused on symptom control and quality of life [1-4]. Our patient’s transient response to modified chemotherapy is a common experience, reflecting the treatment-resistant nature of the disease in this advanced setting.
The role of surgery is highly selective and primarily palliative, aimed at managing local complications such as intractable pain, ulceration, hemorrhage, or urinary obstruction unresponsive to conservative measures [13, 14]. Surgical options range from local excision to partial or total penectomy, with the choice depending on the lesion’s characteristics and the patient’s overall condition [3, 13, 14]. While isolated reports describe patients with metachronous, solitary metastases achieving prolonged survival after aggressive resection [3, 13], such outcomes are exceptional. In the vast majority of cases, like ours with synchronous multisystem dissemination, surgery on the primary penile lesion is not indicated, as it does not alter the disease course and can add unnecessary morbidity. Therefore, the decision to operate must be made within a multidisciplinary framework, carefully weighing the potential for local symptom relief against the procedural risks and the patient’s overall prognosis [13, 14].
A notable limitation of this case is the lack of postmortem examination to definitively confirm the dissemination mechanism. Furthermore, the conclusions from our literature review are constrained by the inherent heterogeneity of individual case reports. Future efforts should focus on the molecular characterization of such aggressive cases to identify potential therapeutic targets. Moreover, the establishment of international, multi-institutional registries is crucial to collect standardized data on genomics, treatment sequences, and outcomes. This collaborative approach is the only viable path to moving beyond isolated reports and developing evidence-based strategies for these challenging clinical scenarios.
Conclusions
Penile metastasis from rectal adenocarcinoma is an exceptionally rare yet devastating manifestation of advanced, systemic disease, consistently associated with a profoundly poor prognosis, as confirmed by our literature review and the rapid progression in our case [1, 4, 6]. This case transcends its rarity to deliver several critical clinical lessons. First, it demonstrates that such a presentation can signal exceptionally aggressive tumor biology, even in young patients, warranting a high index of suspicion in any patient with a history of CRC presenting with urological symptoms [1, 4]. Second, it powerfully illustrates the non-negotiable role of pharmacogenetics in modern oncology; pre-emptive screening for variants like UGT1A1*28 is essential to personalize palliative chemotherapy, avoid life-threatening toxicity, and preserve quality of life [12]. Finally, it underscores the strictly palliative role of local therapies, including surgery, which must be reserved for symptom control in select cases and decided within a multidisciplinary framework, as it does not alter the inevitable progression of widespread disease [3, 13, 14].
The study of these rare cases remains vital. Future progress hinges on moving beyond isolated reports through collaborative international registries that can aggregate molecular and clinical data to uncover patterns, identify therapeutic targets, and ultimately improve outcomes for patients facing this formidable clinical challenge.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from the patient for the publication of his clinical information.
Author Contributions
DQEM contributed to the writing of the case report, preparation of the figures, revisions, and management of the submission process. JEHS and ICD contributed to the revisions of the text and the analysis of images.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
CRC: colorectal cancer; FOLFOX: folinic acid, fluorouracil, oxaliplatin; FOLFIRI: folinic acid, fluorouracil, irinotecan; CAPEOX: capecitabine, oxaliplatin; RT: radiotherapy; Sx: surgery; NA: not available; Dx: diagnosis
| References | ▴Top |
- Kaminskas A, Patasius A, Kincius M, Sapoka V, Zilevicius R, Garnelyte A, Dulskas A. A case report and review of the literature of penile metastasis from rectal cancer. Front Surg. 2022;9:814832.
doi pubmed - Nasrallah OG, Fawaz MW, Mahdi JH, Armache AK, El Sayegh N, Nasr RW. Peno-scrotal metastasis of colorectal adenocarcinoma: A case report and review of the literature. Int J Surg Case Rep. 2024;122:110078.
doi pubmed - Wang Z, Shan J, Zhou X, Wang J, Yu G, Dong W, Huai F, et al. Surgery, radiotherapy, chemotherapy, targeted therapy, and immunotherapy of rectal adenocarcinoma with penile metastasis: a case report. J Gastrointest Oncol. 2023;14(2):1155-1165.
doi pubmed - Lee TG, Son SM, Kim MJ, Lee SJ. Penile metastasis in rectal cancer with pathologic complete response after neoadjuvant chemoradiotherapy: The first case report and literature review. Medicine (Baltimore). 2020;99(29):e21215.
doi pubmed - Cocci A, Hakenberg OW, Cai T, Nesi G, Livi L, Detti B, Minervini A, et al. Prognosis of men with penile metastasis and malignant priapism: a systematic review. Oncotarget. 2018;9(2):2923-2930.
doi pubmed - Efared B, Ebang GA, Tahirou S, Tahiri L, Sidibe IS, Erregad F, Sow A, et al. Penile metastasis from rectal adenocarcinoma: a case report. BMC Res Notes. 2017;10(1):564.
doi pubmed - Hizli F, Berkmen F. Penile metastasis from other malignancies. A study of ten cases and review of the literature. Urol Int. 2006;76(2):118-121.
doi pubmed - Paquin AJ, Jr., Roland SI. Secondary carcinoma of the penis; a review of the literature and a report of nine new cases. Cancer. 1956;9(3):626-632.
doi pubmed - Abeshouse BS, Abeshouse GA. Metastatic tumors of the penis: a review of the literature and a report of two cases. J Urol. 1961;86:99-112.
doi pubmed - Zang S, Yang Y. Isolated penile metastasis from rectal carcinoma after abdominoperineal resection: a case report and review of the literature. ANZ J Surg. 2021;91(6):E411-E412.
doi pubmed - Gomez-de la Fuente FJ, Martinez-Rodriguez I, Alonso-Martin J, Jimenez-Bonilla J, Banzo I. A case report of penile metastases from rectal carcinoma. Cir Esp. 2017;95(2):116-118.
doi pubmed - Innocenti F, Undevia SD, Iyer L, Chen PX, Das S, Kocherginsky M, Karrison T, et al. Genetic variants in the UDP-glucuronosyltransferase 1A1 gene predict the risk of severe neutropenia of irinotecan. J Clin Oncol. 2004;22(8):1382-1388.
doi pubmed - Yin GL, Zhu JB, Fu CL, Ding RL, Zhang JM, Lin Q. Metachronous isolated penile metastasis from sigmoid colon adenocarcinoma: A case report. World J Clin Cases. 2022;10(31):11658-11664.
doi pubmed - Dong Z, Qin C, Zhang Q, Zhang L, Yang H, Zhang J, Wang F. Penile metastasis of sigmoid colon carcinoma: a rare case report. BMC Urol. 2015;15:20.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.