| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 8, August 2025, pages 323-329
A Successful Treatment of Hemifacial Spasm After Flow Diverter Stent Placement for Ipsilateral Internal Carotid Artery Saccular Aneurysm
Ferda Selcuk Muhtaroglua, Belin Kamiloglua, Musa Muhtaroglub, c
aDepartment of Neurology, Dr. Burhan Nalbantoglu State Hospital, Nicosia 99010, North Cyprus
bDepartment of Anatomy, Faculty of Medicine, European University of Lefke, Mersin 10, Lefke 99728, Northern Cyprus, Turkey
cCorresponding Author: Musa Muhtaroglu, Department of Anatomy, Faculty of Medicine, European University of Lefke, Mersin 10, Lefke 99728, Northern Cyprus, Turkey
Manuscript submitted July 7, 2025, accepted August 11, 2025, published online August 22, 2025
Short title: Post-Stenting HFS in Carotid Aneurysm
doi: https://doi.org/10.14740/jmc5165
| Abstract | ▴Top |
Hemifacial spasm (HFS) is a neurological disorder characterized by involuntary, paroxysmal contractions of the muscles innervated by the facial nerve on one side of the face. While primary HFS is most often caused by vascular compression at the root exit zone (REZ) of the facial nerve, secondary causes such as tumors, arteriovenous malformations, and intracranial aneurysms are rare. The management of HFS due to aneurysmal compression remains challenging, and the literature on endovascular treatment, particularly with flow diverter stents, is limited. We report the case of a 56-year-old woman with a history of diabetes mellitus type 2, hypertension, and hypercholesterolemia, who presented with progressive right-sided HFS. Imaging revealed a saccular aneurysm of the right internal carotid artery (ICA) at the cavernous-ophthalmic segment. The patient underwent successful endovascular treatment with a Derivo embolization device (DED) flow diverter stent. Her HFS resolved completely post-procedure, with no neurological deficits or recurrence at 6-month follow-up. This case highlights the efficacy of flow diverter stent placement for HFS caused by ICA saccular aneurysm and represents the first such report from Northern Cyprus. The case underscores the importance of considering secondary etiologies in atypical HFS and demonstrates the therapeutic potential of endovascular flow diversion in this context.
Keywords: Hemifacial spasm; Internal carotid artery; Saccular aneurysm; Flow diverter; Endovascular treatment; Imaging
| Introduction | ▴Top |
Hemifacial spasm (HFS) is a movement disorder characterized by paroxysmal, involuntary contractions of the muscles innervated by the facial nerve, usually on one side of the face. The majority of cases are primary, resulting from vascular compression of the facial nerve root exit zone (REZ), most often by tortuous or ectatic arterial loops [1, 2]. Secondary causes, including tumors, arteriovenous malformations, and aneurysms, are less common but clinically significant. While vertebrobasilar aneurysms are more frequently implicated in secondary HFS, ICA aneurysms are exceedingly rare as a cause [3, 4]. The pathophysiology of HFS involves chronic pulsatile compression of the facial nerve at its REZ, leading to focal demyelination and ephaptic transmission, which results in abnormal muscle responses and involuntary contractions [1, 5, 6]. Advances in neuroimaging, such as high-resolution magnetic resonance imaging (MRI) and computed tomography (CT) angiography, have improved the detection of neurovascular conflicts and secondary causes of HFS [2, 4, 7]. Treatment options for HFS include botulinum toxin injections, microvascular decompression (MVD), and, in cases of secondary HFS due to aneurysm, endovascular or surgical intervention [1, 8-11].
Here, we present a rare case of HFS secondary to a right internal carotid artery (ICA) saccular aneurysm, successfully treated with flow diverter stent placement and coil embolization, and review the relevant literature.
| Case Report | ▴Top |
A 56-year-old woman presented to the neurology outpatient clinic with a 6-month history of involuntary contractions around her right eye, progressively increasing in frequency. Initially confined to the orbicularis oculi muscle, the contractions gradually extended to the ipsilateral zygomatic and periorbital muscles (Fig. 1). These episodes recurred multiple times throughout the day, were exacerbated by stress and fatigue, and resolved completely during sleep. Her past medical history included type 2 diabetes mellitus for 15 years, hypertension, and hypercholesterolemia. Neurological examination revealed intact cranial nerve functions; however, an HFS episode affecting the right side was clinically observed. Cranial MRI was performed to investigate potential structural causes. No space-occupying lesion or vascular malformation was identified in the cerebellopontine angle. However, a suspicious vascular structure was noted in close proximity to the REZ of the facial nerve. Subsequent magnetic resonance angiography (MRA) revealed a saccular aneurysm in the paraclinoid segment of the right ICA, demonstrating inferomedial projection (Fig. 2). The aneurysm measured approximately 4.8 mm in diameter and was anatomically adjacent to the optic nerve and the oculomotor nerve (cranial nerve III).
 Click for large image | Figure 1. Appearance consistent with hemifacial spasm (HFS) prior to the patient’s treatment. |
 Click for large image | Figure 2. (a, b) Magnetic resonance angiography (MRA) reveals a saccular aneurysm arising from the cavernous-ophthalmic segment of the right internal carotid artery (ICA), as indicated by the red arrow. |
These findings were confirmed by digital subtraction angiography (DSA) (Fig. 3). Moreover, MRA fusion imaging clearly demonstrated inferomedially oriented arterial contact at the level of the facial nerve REZ.
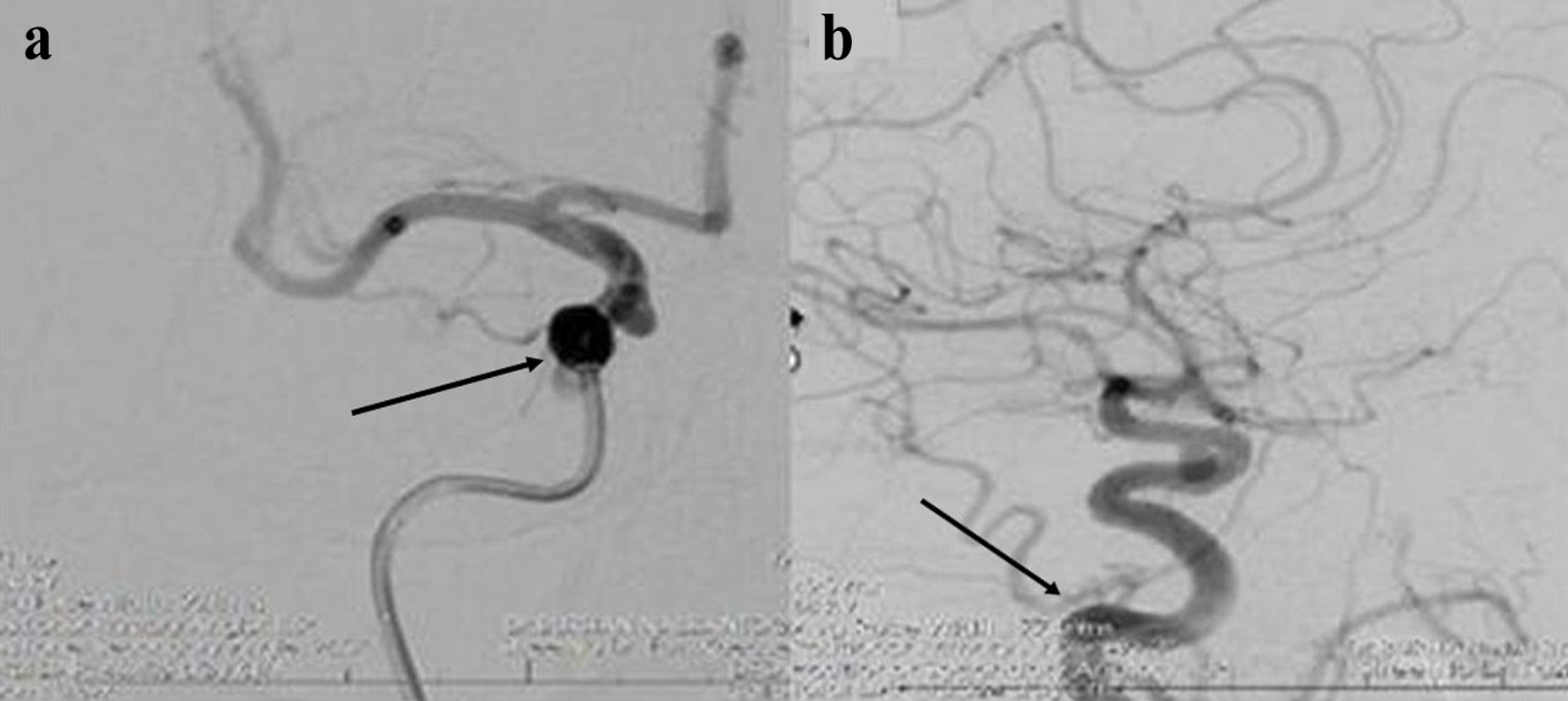 Click for large image | Figure 3. (a, b) Digital subtraction angiography (DSA) images demonstrate a saccular aneurysm located in the cavernous-ophthalmic segment of the right internal carotid artery (ICA). The aneurysmal dome is marked with black arrows in both panels. |
Treatment
Before the endovascular procedure, the patient was started on dual antiplatelet therapy with aspirin 100 mg daily and ticagrelor 90 mg twice daily, which was continued postoperatively. The procedure was performed under general anesthesia via a right femoral artery approach. A Derivo embolization device (DED) (Acandis GmbH & Co. KG, Pforzheim, Germany), a new-generation nitinol flow diverter stent with proven efficacy in the treatment of intracranial aneurysms, was selected. The stent was successfully deployed across the neck of the aneurysm in the right ICA, ensuring complete coverage and optimal wall apposition (Fig. 4). Post-deployment angiography showed contrast stagnation within the aneurysm sac, indicating effective flow diversion. No procedural complications occurred. The patient tolerated the procedure well and was monitored in the neurocritical care unit for 48 h (Fig. 5). Dual antiplatelet therapy was maintained. Remarkably, her HFS resolved completely within 48 h. She was discharged on postoperative day 4 with instructions to continue dual antiplatelet therapy for 6 months, followed by aspirin monotherapy. At 6-month clinical and radiological follow-up, the patient remained free of HFS, with no new neurological deficits or evidence of aneurysm recurrence.
 Click for large image | Figure 4. Digital subtraction angiography (DSA) demonstrates the deployment of a flow diverter stent across a saccular aneurysm located in the cavernous-ophthalmic segment of the right internal carotid artery (ICA). The stent position and covered aneurysmal segment are indicated by black arrows. |
 Click for large image | Figure 5. The patient’s symptoms regressed after treatment. |
| Discussion | ▴Top |
Mechanisms of HFS
HFS is most commonly attributed to neurovascular contact (NVC) at the REZ of the facial nerve, where the central myelin transitions to peripheral myelin, rendering the nerve particularly susceptible to pulsatile vascular compression [1]. The offending vessel is typically an ectatic or tortuous artery, most frequently the anterior inferior cerebellar artery (AICA), posterior inferior cerebellar artery (PICA), or vertebral artery (VA) [1, 12]. Chronic pulsatile compression leads to focal demyelination, ephaptic transmission, and hyperexcitability of the facial nerve fibers, resulting in the characteristic involuntary contractions [1]. Secondary HFS, while rare, can result from a variety of structural lesions, including tumors, arteriovenous malformations, and aneurysms [2]. In the context of aneurysms, the mechanism is thought to involve direct compression of the facial nerve at or near the REZ, or, less commonly, distortion of the brainstem or adjacent neurovascular structures [2, 13]. The precise pathophysiological mechanisms may vary depending on the size, location, and growth dynamics of the aneurysm.
Differential diagnosis: primary vs. secondary HFS
Distinguishing primary from secondary HFS is critical, as management strategies and prognoses differ. Primary HFS is overwhelmingly more common and is typically diagnosed based on clinical presentation and neuroimaging demonstrating vascular contact at the REZ without other structural lesions [1]. Secondary HFS should be suspected in patients with atypical features, such as rapid progression, onset at a young age, bilateral involvement, or associated neurological deficits [2, 14]. Neuroimaging, particularly high-resolution MRI and MRA, is essential for identifying secondary causes [15]. In the present case, the detection of a saccular aneurysm at the cavernous-ophthalmic segment of the ICA, in the absence of other lesions, strongly supported a diagnosis of secondary HFS.
Literature review: aneurysm-related HFS
A comprehensive review of the literature from 1970 to 2023 identified only 22 previously reported cases of HFS caused by intracranial aneurysms (Table 1 [4-6, 8-26]). The majority of these cases involved aneurysms of the vertebral artery or its branches, with saccular morphology in 11 cases, fusiform in seven cases, and dissecting in four cases [5, 8-11, 16-26]. The present case is unique in that the aneurysm was located at the cavernous-ophthalmic segment of the ICA, a rare site for HFS-related aneurysms. Treatment modalities in prior cases have included parent artery occlusion (PAO), coil embolization, surgical clipping, MVD, and, more recently, flow diversion [5, 8-11, 16-26]. Outcomes have generally been favorable, with most patients experiencing resolution of HFS following treatment of the aneurysm. However, recurrence has been reported, particularly in cases where the aneurysm was not completely excluded from the circulation or where persistent neurovascular contact remained [8].
 Click to view | Table 1. Summary of Reported Cases of Hemifacial Spasm Associated With Intracranial Aneurysms (n = 23) |
Unique aspects of flow diverter stents in HFS
Flow diverter stents represent a significant advance in the endovascular management of complex intracranial aneurysms. These devices, composed of tightly braided nitinol wires, are designed to redirect blood flow away from the aneurysm sac, promoting thrombosis and eventual occlusion while preserving flow through the parent vessel and adjacent branches. The DED used in this case has demonstrated high rates of aneurysm occlusion and favorable safety profiles in large series [2]. The use of flow diverter stents in the context of HFS is particularly appealing for several reasons. First, these devices can achieve complete and durable exclusion of the aneurysm from the circulation, thereby eliminating the source of neurovascular compression. Second, flow diversion avoids the need for open surgical approaches, which carry higher risks of morbidity, particularly in anatomically challenging locations such as the cavernous-ophthalmic ICA. Third, the minimally invasive nature of endovascular therapy allows for rapid recovery and early resolution of symptoms, as observed in the present case. While the literature on flow diverter stents for HFS is limited, several reports have documented successful outcomes with this approach, particularly in cases where traditional surgical or endovascular techniques were not feasible or had failed [2, 17, 26]. The present case adds to this growing body of evidence, demonstrating the efficacy and safety of flow diversion in the management of aneurysm-related HFS.
Clinical decision-making rationale
The decision to proceed with flow diverter stent placement in this case was based on several factors. The aneurysm was unruptured, saccular, and located at the cavernous-ophthalmic segment of the ICA, making it amenable to endovascular therapy. The patient’s comorbidities (diabetes, hypertension, hypercholesterolemia) increased the risks associated with open surgical approaches. Furthermore, the rapid progression and severity of her HFS symptoms warranted prompt intervention. Multidisciplinary discussion involving neurology, neurosurgery, and interventional neuroradiology teams concluded that flow diversion offered the best balance of efficacy and safety. The patient was counseled regarding the risks and benefits of the procedure, including the need for prolonged dual antiplatelet therapy and the potential for delayed aneurysm occlusion. Although diabetes mellitus is a known contributor to cranial neuropathies through chronic microvascular changes [27, 28], in this case, it was considered a secondary factor rather than a primary cause of HFS. The anatomical compression of the facial nerve REZ by the adjacent aneurysm provided a clear and sufficient explanation for the patient’s symptoms. Nevertheless, the presence of diabetes was taken into account during treatment planning, as it contributed to the patient’s overall perioperative risk and further justified the choice of a less invasive endovascular approach.
Long-term management and follow-up
Long-term management of patients treated with flow diverter stents includes regular clinical and radiological follow-up to monitor for recurrence of symptoms, aneurysm occlusion, and device-related complications. Dual antiplatelet therapy is typically continued for 6 months, followed by aspirin monotherapy, to minimize the risk of in-stent thrombosis [2]. In the present case, the patient remained symptom-free at 6 months, with no evidence of aneurysm recurrence or device-related complications. The durability of symptom resolution following flow diversion is supported by the literature, with most patients experiencing sustained relief of HFS [17, 18]. However, longer-term follow-up is necessary to assess for late recurrences or delayed complications.
Evolution of flow diverter technology
Flow diverter technology has evolved significantly, with newer-generation devices providing improved deliverability, safety, and efficacy for complex aneurysms. Recent advances include the development of dissolvable flow diverters, which may reduce the need for long-term dual antiplatelet therapy (DAPT), thereby minimizing bleeding risks and improving patient compliance [29]. These innovations expand the therapeutic options for patients with challenging aneurysm anatomies and comorbidities.
Conclusions
This case represents the first reported instance in Northern Cyprus of successful treatment of HFS due to a saccular aneurysm of the cavernous-ophthalmic segment of the ICA using a flow diverter stent. The case underscores the importance of considering secondary causes in patients with atypical HFS and highlights the therapeutic potential of endovascular flow diversion in this context. Flow diverter stents offer a safe and effective alternative to open surgery, with the potential for rapid and durable symptom resolution. Ongoing follow-up is essential to ensure long-term efficacy and safety.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
This investigation was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from the patient for the publication of this case report and any accompanying clinical images.
Author Contributions
Conceptualization: FSM and BK; methodology: FSM; validation: FSM and BK; investigation: MM; resources: FSM; data curation: MM; writing - original draft preparation: MM; writing - review and editing: BK and FSM; visualization: MM; supervision: BK; project administration: BK. All authors have read and agreed to the published version of the manuscript.
Data Availability
The data supporting the findings of this case report are not publicly available due to patient privacy and ethical considerations. Data may be made available from the corresponding author upon reasonable request and with appropriate institutional and ethical approval.
| References | ▴Top |
- Sindou M, Mercier P. Microvascular decompression for hemifacial spasm: Outcome on spasm and complications. A review. Neurochirurgie. 2018;64(2):106-116.
doi pubmed - Satoh T, Onoda K, Date I. Fusion imaging of three-dimensional magnetic resonance cisternograms and angiograms for the assessment of microvascular decompression in patients with hemifacial spasms. J Neurosurg. 2007;106(1):82-89.
doi pubmed - Maroon JC, Lunsford LD, Deeb ZL. Hemifacial spasm due to aneurysmal compression of the facial nerve. Arch Neurol. 1978;35(8):545-546.
doi pubmed - Nagata S, Matsushima T, Fujii K, Fukui M, Kuromatsu C. Hemifacial spasm due to tumor, aneurysm, or arteriovenous malformation. Surg Neurol. 1992;38(3):204-209.
doi pubmed - Kugai M, Suyama T, Inui T, Yamazato K, Kitano M, Hasegawa H, et al. A case of vertebral artery aneurysm causing hemifacial spasm rapidly improved after parent artery occlusion. Noushinkei Kekkannai Tiryou. 2019;13:288-292.
doi - Ko HC, Lee SH, Shin HS, Koh JS. Treatment for hemifacial spasm associated with a dissecting vertebral artery aneurysm requiring microvascular decompression in addition to endovascular trapping: a case report with literature review. J Neurol Surg A Cent Eur Neurosurg. 2022;83(4):377-382.
doi pubmed - Tarnaris A, Renowden S, Coakham HB. A comparison of magnetic resonance angiography and constructive interference in steady state-three-dimensional Fourier transformation magnetic resonance imaging in patients with hemifacial spasm. Br J Neurosurg. 2007;21(4):375-381.
doi pubmed - Arisawa K, Ochi T, Goto Y, Nanbu S, Shojima M, Maeda K. Coil embolization of VA-PICA aneurysm presenting with hemifacial spasm with assistance of abnormal muscle response monitoring. J Neuroendovasc Ther. 2020;14(4):146-150.
doi pubmed - Iida Y, Mori K, Kawahara Y, Fukui I, Abe K, Takeda M, Nakano T, et al. Hemifacial spasm caused by vertebral artery aneurysm treated by endovascular coil embolization. Surg Neurol Int. 2020;11:431.
doi pubmed - Matsumoto K, Saijo T, Kuyama H, Asari S, Nishimoto A. Hemifacial spasm caused by a spontaneous dissecting aneurysm of the vertebral artery. Case report. J Neurosurg. 1991;74(4):650-652.
doi pubmed - Uchino M, Nomoto J, Ohtsuka T, Kuramitsu T. Fusiform aneurysm of the vertebral artery presenting with hemifacial spasm treated by microvascular decompression. Acta Neurochir (Wien). 2005;147(8):901-903.
doi pubmed - Nagashima H, Orz Y, Okudera H, Kobayashi S, Ichinose Y. Remission of hemifacial spasm after proximal occlusion of vertebrobasilar dissecting aneurysm with coils: case report. J Clin Neurosci. 2001;8(1):43-45.
doi pubmed - Sato K, Ezura M, Takahashi A, Yoshimoto T. Fusiform aneurysm of the vertebral artery presenting hemifacial spasm treated by intravascular embolization: case report. Surg Neurol. 2001;56(1):52-55.
doi pubmed - Murakami H, Kawaguchi T, Fukuda M, Ito Y, Hasegawa H, Tanaka R. Monitoring of the lateral spread response in the endovascular treatment of a hemifacial spasm caused by an unruptured vertebral artery aneurysm. Case report. J Neurosurg. 2004;101(5):861-863.
doi pubmed - Matsumoto K, Kimura S, Kakita K. Endovascular treatment of vertebral artery aneurysm manifesting as progressive hemifacial spasm. Neurol Med Chir (Tokyo). 2005;45(7):360-362.
doi pubmed - Nakagawa I, Takayama K, Kurokawa S, Wada T, Nakagawa H, Kichikawa K, Nakase H. Hemifacial spasm due to contralateral aneurysmal compression of the facial nerve successfully treated with endovascular coil embolization: case report. Neurosurgery. 2011;69(3):E768-771; discussion E771-762.
doi pubmed - Santiago-Dieppa DR, McDonald MA, Brandel MG, Rennert RC, Khalessi AA, Olson SE. Endovascular flow diversion for hemifacial spasm induced by a vertebral artery aneurysm: first experience. Oper Neurosurg. 2019;17(3):E115-E118.
doi pubmed - Satoh T, Sato Y, Sugiu K, Hishikawa T, Hiramatsu M, Haruma J, Date I. Hemifacial spasm due to vertebral artery dissecting aneurysm treated with stent-in-stent placement; Pre- and post-treatment evaluation by 3D multifusion imaging using silent MR angiography. Surg Neurol Int. 2022;13:232.
doi pubmed - Moriuchi S, Nakagawa H, Yamada M, Kadota T. Hemifacial spasm due to compression of the facial nerve by vertebral artery-posterior inferior cerebellar artery aneurysm and elongated vertebral artery—case report. Neurol Med Chir (Tokyo). 1996;36(12):884-887.
doi pubmed - Tsuchiya D, Kayama T, Saito S, Sato S. [Hemifacial spasm due to a compression of the facial nerve by a fusiform aneurysm of the vertebral artery: case report]. No To Shinkei. 2000;52(6):517-521.
pubmed - Choi SK, Rhee BA, Park BJ, Lim YJ. Hemifacial spasm caused by fusiform aneurysm at vertebral artery-posterior inferior cerebellar artery junction. J Korean Neurosurg Soc. 2008;44(6):399-400.
doi pubmed - Furtado SV, Thakar S, Saikiran NA, Hegde AS. Hemifacial spasm and jugular foramen syndrome caused by diametrically opposite aneurysms on the vertebral artery. Neurol Sci. 2013;34(10):1809-1810.
doi pubmed - Lee SH, Choi SK, Kim J. Real-time monitoring of the lateral spread response resulting from serial decompression for hemifacial spasm caused by a fusiform aneurysm. J Neurol Surg A Cent Eur Neurosurg. 2015;76(4):332-336.
doi pubmed - Chang B, Tang Y, Li Y, Zhu J, Zheng X, Li S. A successful treatment of hemifacial spasm due to anterior inferior cerebellar artery aneurysm in adolescent: a case report and literature review. Childs Nerv Syst. 2021;37(1):339-343.
doi pubmed - Arai S, Shimizu K, Matsumoto M, Mizutani T. Surgical treatment of hemifacial spasm caused by fusiform vertebral artery aneurysm: case report and literature review. Br J Neurosurg. 2024;38(6):1426-1428.
doi pubmed - Inoue G, Endo H, Kanoke A, Kawaguchi T, Tominaga T. Hemifacial spasm associated with posterior inferior cerebellar artery aneurysm: illustrative case. J Neurosurg Case Lessons. 2023;5(15):CASE23102.
doi pubmed - Feldman EL, Nave KA, Jensen TS, Bennett DLH. New horizons in diabetic neuropathy: mechanisms, bioenergetics, and pain. Neuron. 2017;93(6):1296-1313.
doi pubmed - Ghosh R, Roy D, Chatterjee S, Dubey S, Swaika BC, Mandal A, Benito-Leon J. Hemifacial spasm as the presenting manifestation of type 3c diabetes mellitus. Tremor Other Hyperkinet Mov (N Y). 2021;11:14.
doi pubmed - Trivelato FP, Abud DG, Ulhoa AC, Waihrich ES, Abud TG, Castro Afonso LH, Nakiri GS, et al. Derivo embolization device for the treatment of intracranial aneurysms. Stroke. 2019;50(9):2351-2358.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.