
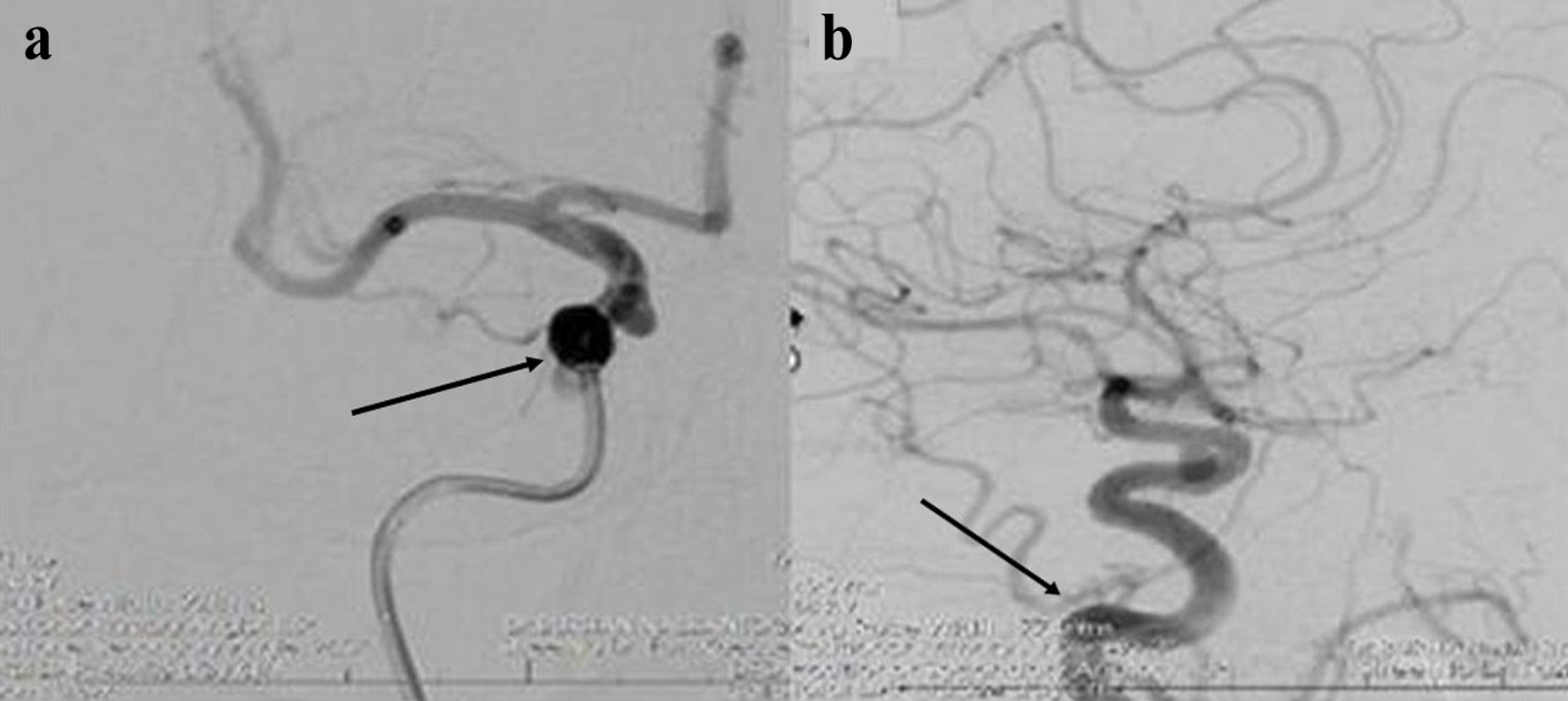
Figure 1. Appearance consistent with hemifacial spasm (HFS) prior to the patient’s treatment.
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 8, August 2025, pages 323-329
A Successful Treatment of Hemifacial Spasm After Flow Diverter Stent Placement for Ipsilateral Internal Carotid Artery Saccular Aneurysm
Figures




Table
| Case No. | Author and year | Age/sex | AN location | AN type and offending vessel | Treatment | Outcome |
|---|---|---|---|---|---|---|
| AN: aneurysm; AICA: anterior inferior cerebellar artery; BA: basilar artery; Coil: endovascular coil embolization; DED: Derivo embolization device; ICA: internal carotid artery; MVD: microvascular decompression; PAO: parent artery occlusion; PICA: posterior inferior cerebellar artery; SAC: stent-assisted coiling; VA: vertebral artery; V3/V4: vertebral artery segments. | ||||||
| 1 | Nagashima et al, 2001 [12] | 69/M | VA-BA junction | Dissection | PAO | Cure |
| 2 | Sato et al, 2001 [13] | 53/M | PICA | Fusiform AN | PAO | Cure |
| 3 | Murakami et al, 2004 [14] | 49/F | V3-V4 junction | Saccular AN | PAO | Cure |
| 4 | Matsumoto et al, 2005 [15] | 62/F | PICA | Saccular AN | PAO | Cure |
| 5 | Nakagawa et al, 2011 [16] | 55/F | VA union | Fusiform AN | PAO | Cure |
| 6 | Kugai et al, 2019 [5] | 56/M | VA union | Saccular AN | PAO | Cure |
| 7 | Santiago-Dieppa et al, 2019 [17] | 60/F | V4 segment | Saccular AN | PAO | Cure |
| 8 | Arisawa et al, 2020 [8] | 62/F | V4 segment | Saccular AN | SAC | Recurrence |
| 9 | Iida et al, 2020 [9] | 59/M | VA-PICA | Saccular AN | Coil | Cure |
| 10 | Satoh et al, 2022 [18] | 50/M | V4 segment | Dissection | Stent | Cure |
| 11 | Ko et al, 2022 [6] | 42/M | V4 segment | Dissection + PICA | PAO | Cure after MVD |
| 12 | Matsumoto et al, 1991 [10] | 58/M | V4 segment | Dissection | MVD | Cure |
| 13 | Nagata et al, 1992 [4] | 70/F | VA-PICA | Saccular AN | Clip | Cure |
| 14 | Moriuchi et al, 1996 [19] | 62/F | VA-PICA | Saccular AN | Clip + MVD | Cure |
| 15 | Tsuchiya et al, 2000 [20] | 71/F | V4 segment | Fusiform AN + AICA | Clip + MVD | Cure |
| 16 | Uchino et al, 2005 [11] | 59/F | V4 segment | Fusiform AN | MVD | Cure |
| 17 | Choi et al, 2008 [21] | 45/M | V4 segment | Fusiform AN + PICA | MVD | Cure |
| 18 | Furtado et al, 2013 [22] | 50/F | V4 segment | Saccular AN + VA | Clip + MVD | Cure |
| 19 | Lee et al, 2015 [23] | 69/M | V4 segment | Dissection | MVD | Cure |
| 20 | Chang et al, 2021 [24] | 17/M | AICA | Saccular AN | Clip + MVD | Cure |
| 21 | Arai et al, 2022 [25] | 64/M | V4 segment | Fusiform AN + AICA | MVD | Cure |
| 22 | Inoue et al, 2023 [26] | 68/M | VA-PICA | Saccular AN | Clip + MVD | Cure |
| 23 | Present case | 56/F | ICA cavernous-ophthalmic | Saccular AN | Flow diverter stent | Cure |