| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 7, July 2025, pages 239-247
Investigation and Management of a Small Outbreak of Septic Knee Arthritis Following Knee Arthroscopy by Stenotrophomonas maltophilia
Li Yina, Shuang Yanga, Dong Fa Liaoa, Wei Jie Yanga, Jin Biao Liua, Bing Denga, b
aDepartment of Orthopaedics, General Hospital of Western Theater Command, Chengdu, Sichuan, China
bCorresponding Author: Bing Deng, Department of Orthopaedics, General Hospital of Western Theater Command, Chengdu, Sichuan 610083, China
Manuscript submitted May 4, 2025, accepted June 17, 2025, published online July 8, 2025
Short title: Serial Cases of Rare Knee Septic Arthritis
doi: https://doi.org/10.14740/jmc5138
| Abstract | ▴Top |
Knee septic arthritis caused by Stenotrophomonas maltophilia (S. maltophilia) was very rare in immunocompetent group but was observed in a series of post-arthroscopy patients in our hospital. This study aimed to report the clinical course and treatments of the infections and the investigation of the incidents. One patient who underwent knee arthroscopy exhibited serious knee septic arthritis 17 days postoperatively. Later, three more similar patients were also suspected of knee infection. Investigation was initiated by interviews with personnel and reviews of medical records. All instruments associated with arthroscopy were subsequently sampled and tested. While no abnormalities were revealed in medical personnel and records, positive culture of S. maltophilia was found on one arthroscope, used in all four infected patients. No violations were found in sterilization processes. The contaminated arthroscope was proven loss of airtightness subsequently. For infection treatment, double or triple therapy of levofloxacin, sulfamethoxazole-trimethoprim, and minocycline was administered, with additional debridement performed in one patient. By retrospective survey, another three patients were suspected of infection out of the total 19 patients who underwent knee arthroscopy in last 4 weeks. After intervention, all involved patients recovered. Although S. maltophilia is a rare cause of knee septic arthritis, it can still occur and even lead to nosocomial outbreaks through instrument-related transmission. Sulfamethoxazole-trimethoprim, levofloxacin, and minocycline remain the treatment of choice, despite the rising global resistance rates. Although hydrogen peroxide gas plasma sterilization serves as a fast and effective method for instrument sterilization in arthroscopy, maintaining good arthroscope condition and airtightness ensures success, which warrants periodic checks.
Keywords: Stenotrophomonas maltophilia; Knee septic arthritis; Surgical site infection; Nosocomial infection; Arthroscopy; Sterilization
| Introduction | ▴Top |
Stenotrophomonas maltophilia (S. maltophilia) is an opportunistic aerobic gram-negative bacillus widely distributed in water, soil, and plants. In hospital settings, it is frequently isolated from various sources such as medical equipment, tap water, and ventilators, posing risk on nosocomial infections in compromised patients. Over the past decades, the incidence of S. maltophilia infections has been on the rise, making it an emerging multidrug-resistant opportunistic pathogen globally [1, 2].
S. maltophilia is commonly associated with respiratory system in form of tracheobronchitis or pneumonia [3]. Other forms of infection may involve urinary tract, biliary system, and gastrointestinal system [1]. Bone and soft tissue infections are less prevalent, with a few cases reported in individuals with a history of trauma and skin lesions [4-6]. Notably, instances of knee septic arthritis attributed to S. maltophilia are very rare. Only a minimal number of cases have been reported [7].
In a recent discovery, a series of immunocompetent patients were found to be infected with S. maltophilia at the surgical site following knee arthroscopy. This study aimed to report the clinical presentation, disease course, and treatment of S. maltophilia-related knee septic arthritis, as well as to investigate how an infection outbreak occurred within a routine clinical setting.
| Case Reports | ▴Top |
Investigations
Onset of incidents
1) Case 1
A 23-year-old male patient revisited the outpatient department, and this date was designated as day 0 for subsequent reference. Seventeen days earlier, he had undergone arthroscopic partial lateral meniscectomy and medial meniscus repair in the left knee. During examination, he presented with a swollen, hot, and painful knee, accompanied by a fever of approximately 38.5 °C. These symptoms had emerged 5 days postoperatively and had worsened until the revisit. Arthroscopic incisions had healed satisfactorily, and the surrounding skin was intact.
Initial blood tests showed a normal white blood cell count and a significantly elevated C-reaction protein of 87.25 mg/L. A knee arthrocentesis was performed, yielding 80 mL of pale red, cloudy joint fluid (Fig. 1a). The sample was immediately tested for gram stain and bacterial culture, but cell count was not performed.
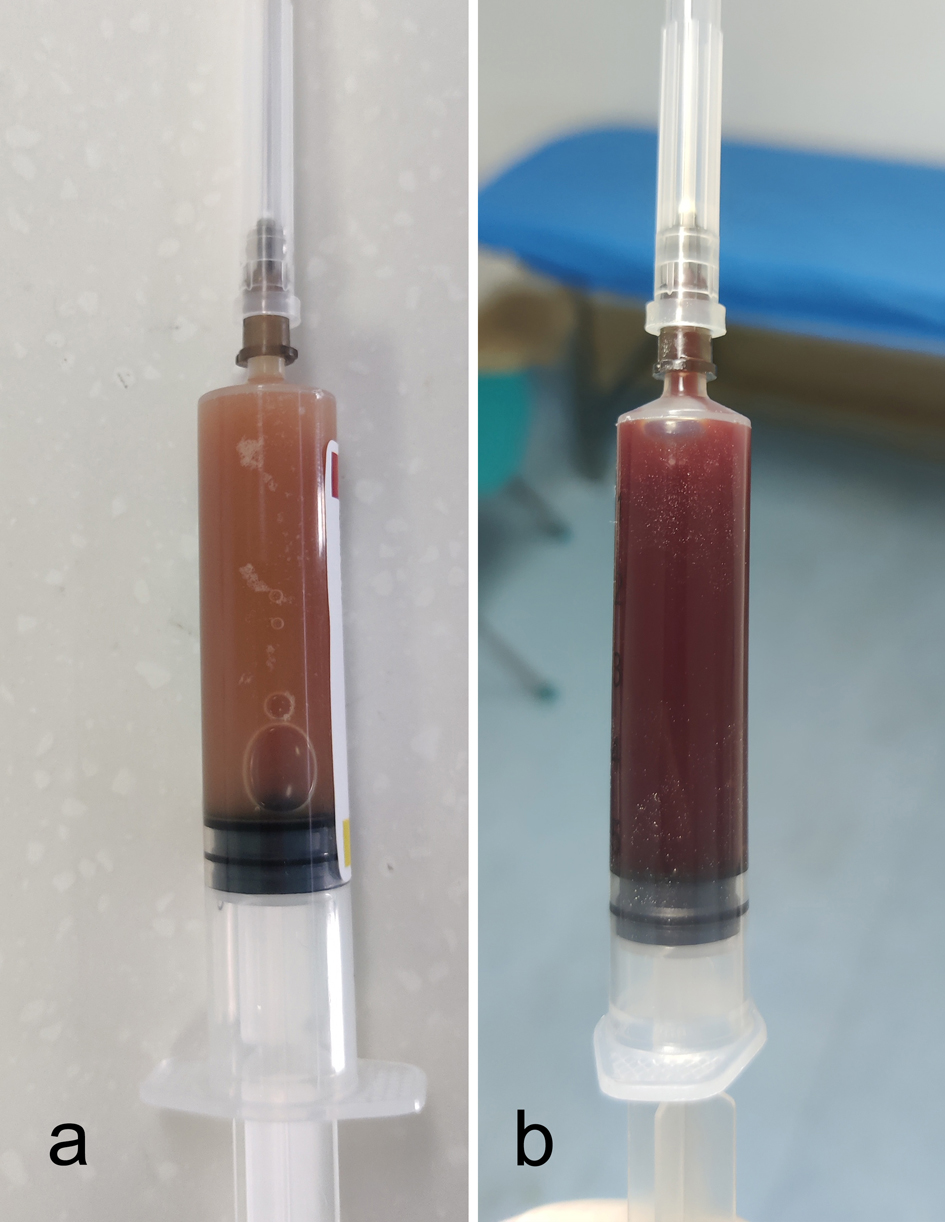 Click for large image | Figure 1. The joint fluid of two infected patients through knee arthrocentesis. (a) Case 1. (b): Case 2. |
Knee septic arthritis was highly suspected for case 1. An arthroscopic debridement was performed on day 1, revealing extensive red, edematous synovium. A large amount of necrotic tissue and purulent secretion were also observed. Despite widespread inflammation throughout the joint cavity, the articular cartilage appeared intact (Fig. 2). Samples were collected for biopsy, followed by a thorough joint debridement. Continuous irrigation and drainage were implemented for 1 week. Cefepime-sulbactam (3.0 g/8 h) was administered empirically. Although the patient experienced relief from fever and knee pain over the following days, the symptoms worsened again on day 5. Microbiological analysis reported a positive culture of S. maltophilia on the same day. On day 7, the antibiotic protocol was modified to levofloxacin (0.5 g/day) and sulfamethoxazole-trimethoprim (SMZ-TMP) (0.96 g/8 h). Subsequent bacterial culture from the drainage necrosis again confirmed the presence of S. maltophilia.
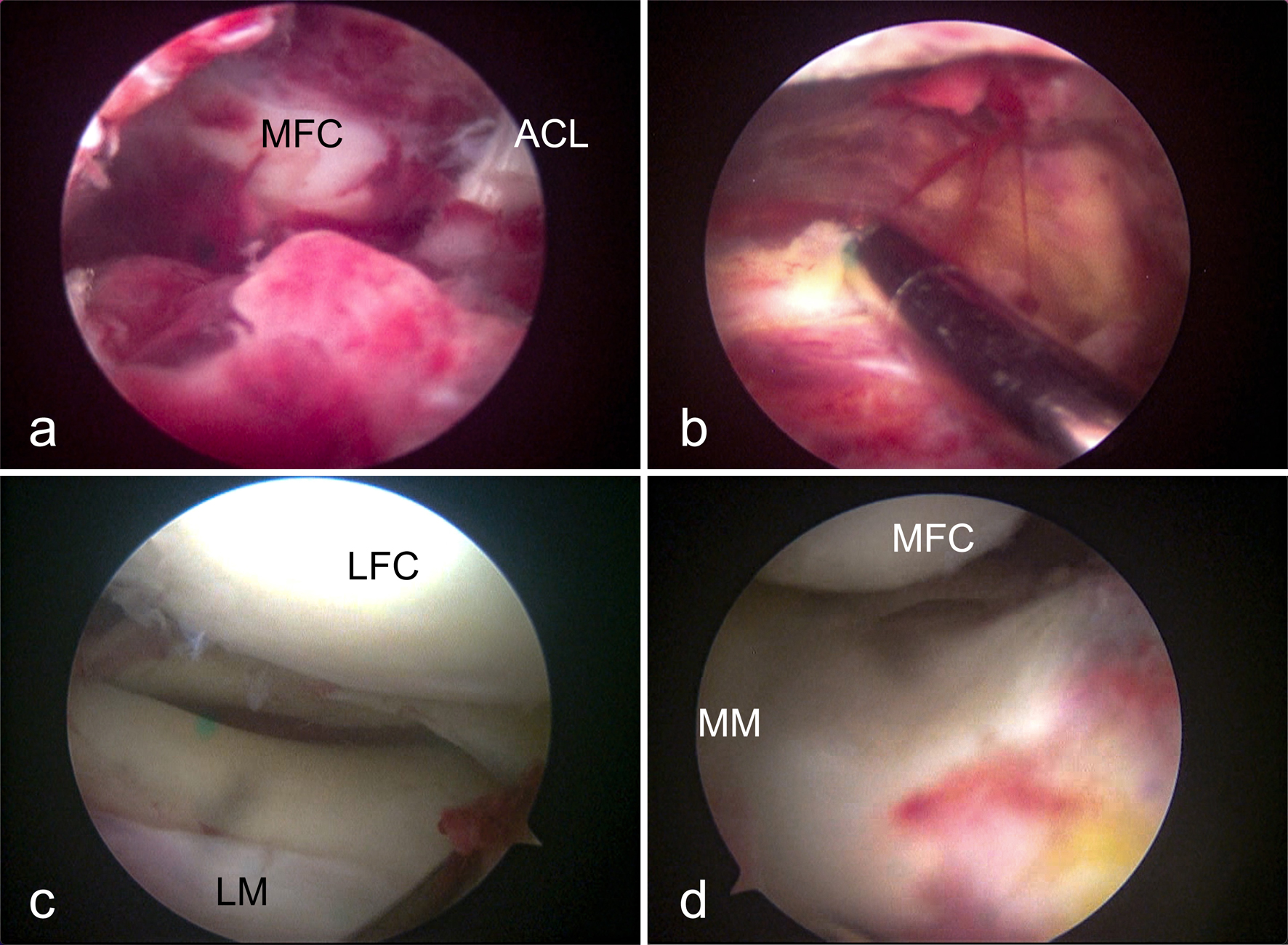 Click for large image | Figure 2. Arthroscopic presentation of knee septic arthritis of Stenotrophomonas maltophilia. (a) Infrapatellar fat pad and medial part of intercondylar notch. (b) Suprapatellar bursa. (c) Lateral compartment. (d) Medial compartment. ACL: anterior cruciate ligament; LFC: lateral femoral condyle; LM: lateral meniscus; MFC: medial femoral condyle; MM: medial meniscus. |
2) Case 2
A 41-year-old female patient underwent arthroscopic partial lateral meniscectomy on day 4. For the following 3 days, she experienced improved mobility, with relieved knee pain and locking. However, on day 8, the affected knee became increasingly swollen. On day 9, she reported worsening knee pain, increased swelling, and fatigue, accompanied by a body temperature rise to 37.1 °C. Knee arthrocentesis yielded 50 mL of bloody yet slightly turbid fluid (Fig. 1b). A regimen of ceftriaxone (2 g/24 h) and SMZ-TMP (0.96 g/12 h) was applied. However, on day 10, the knee swelling recurred, and the body temperature rose to 37.5 °C. The surgical incisions remained clean and dry.
3) Case 3
A 24-year-old male patient underwent anterior cruciate ligament reconstruction (ACLR) and medial meniscus repair on day 2. On day 4, he experienced a low-grade fever of 37.3 °C. The temperature increased to 37.8 °C and knee swelling persisted for the next 2 days. On day 6, knee arthrocentesis was performed, extracting 20 mL of bloody joint fluid. Empirically, ceftriaxone (2.0 g/24 h) was administered. The patient continued to have a low-grade fever of 37.5 °C until day 8. On day 9, microbiological analysis reported a positive culture of S. maltophilia from the arthrocentesis fluid. The surgical incisions remained clean and dry.
4) Case 4
A 44-year-old female patient underwent arthroscopic partial medial meniscectomy on day 5. Until day 8, she exhibited no discomfort, and her body temperature remained normal. However, on day 9, significant swelling and warmth were observed in the knee, along with a slight increase in knee pain. The surgical incisions remained clean and dry. The patient declined knee arthrocentesis and antibiotic treatment.
Respond and investigation
Since four post-arthroscopy patients displayed signs of knee infection within a short timeframe, and two of them tested positive for S. maltophilia, a potential outbreak of nosocomial, arthroscopy-related surgical site infection was suspected. All planned arthroscopic surgeries were halted consequently.
Investigation was initiated by interviews with associated medical personnel, including surgeons, surgical assistants, anesthetists, and nurses. Records of patients, surgeries, and nursing care were reviewed. On day 10, comprehensive sampling of instruments was conducted on those undergoing low-temperature sterilization (e.g., arthroscope, shaver handpiece, light cable) and those subjected to steam autoclave sterilization (e.g., metal instruments and devices). In cases of luminal or complex-shaped devices, multiple samples were taken from various sites to ensure thorough evaluation.
Investigation results
Interviews with personnel and reviews of record revealed no abnormalities. However, on day 11, microbiology reported positive S. maltophilia culture from one of the four arthroscopes used (Smith&nephew, 4 mm 30°, REF 72202087, initiated use in 2019). No further positive cultures were discovered on the other instruments until day 16 (Table 1). A retrospective review of the contaminated arthroscope revealed its usage in all four infected patients. For case 1, the arthroscope was utilized in both the original and debridement operations.
 Click to view | Table 1. Infection Control Investigation of Instruments Associated With Arthroscopy |
Response and treatment
Systematic management
A meticulous examination of sterilization equipment, supplies, and processes was subsequently undertaken. Logs and surveillance footage of instrument reprocessing were scrutinized, and reprocessing workers and supervisors were interviewed. In our facility, hydrogen peroxide gas plasma (HPGP) sterilizers were utilized for all rigid endoscopes, including arthroscopes. The investigation into sterilization processes found no violations against requirements. For further tests, the contaminated arthroscope was subjected to steam autoclave sterilization and subsequently resampled twice alongside other instruments. No positive cultures were found in the subsequent tests. However, a closer examination of the contaminated arthroscope revealed damage, particularly a blurring and foggy field of view, likely caused by steam leak-in during autoclave. Records indicated that the arthroscope had undergone glass replacement months ago. Visual inspection uncovered intact object glasses with a few light scratches and slight deformation with potentially enlarged gap at the metallic junction site of the scope body and object glasses (Fig. 3). This contaminated arthroscope was subsequently suspended from use permanently. Arthroscopic operations resumed on day 25 after two rounds of instrument sampling and tests. HPGP sterilization continued for the remaining arthroscopes, and no further adverse events have occurred since.
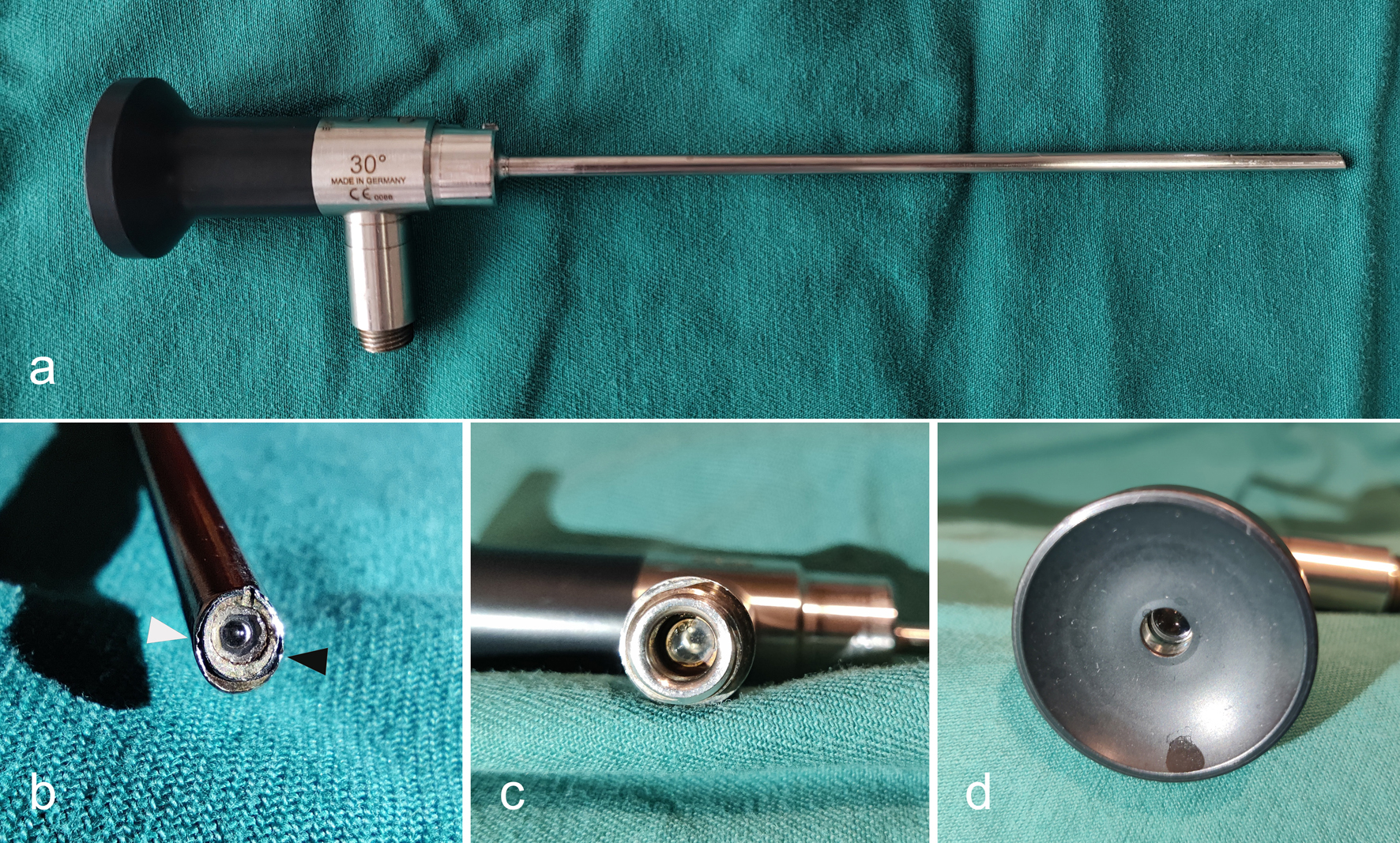 Click for large image | Figure 3. The appearance of the contaminated arthroscope. (a) Gross look. (b) Object glasses: white arrowhead indicates slight deformation at the junction of glasses and scope body; black arrowhead indicates slight deformation and an enlarged gap at the junction. (c) Port for light cable. (d) Camera glasses. |
Retrospective telephone interviews were conducted with all arthroscopic patients from 6 weeks before day 0. Remarkably, no patients before day -17 (the day case 1 underwent meniscectomy and meniscus repair) exhibited infectious phenomena, including those on whom the contaminated arthroscope was used. Consequently, case 1 appeared to be “patient zero.” Since that date, a total of 19 patients were treated with the contaminated arthroscope, including partial meniscectomy, meniscus repair, ACLR, synovectomy, elbow release, and iliotibial band release. In addition to cases 1-4, two more patients with partial meniscectomy were suspected of S. maltophilia infection due to clinical manifestations. However, no pathogens were cultured through arthrocentesis. Both patients were treated with the double or triple antibiotic protocols of levofloxacin, SMZ-TMP, and minocycline, and fully recovered as confirmed during outpatient follow-up visits at 12 and 14 weeks postoperatively, respectively. One patient who underwent synovectomy was also suspected of knee infection. Regrettably, this patient sought treatment in a nonlocal facility, and follow-up was lost. In summary, out of the 19 patients treated with the contaminated arthroscope, seven were suspected of joint infection, with or without the isolation of S. maltophilia (Table 2).
 Click to view | Table 2. Retrospective Survey of Usage of the Contaminated Arthroscope Since “Patient Zero” |
Subsequent treatments of infected patients
1) Case 1
On day 12, due to a blockage in the drainage pipe, a second arthroscopic debridement was conducted, with irrigation and drainage implemented. The intraoperative findings mirrored those of the initial debridement 11 days earlier. The antibiotic protocol was adjusted to levofloxacin (0.75 g/day), SMZ-TMP (1.44 g/8 h), and minocycline (100 mg/12 h). The symptoms exhibited gradual improvement over the following days. Joint irrigation was discontinued on day 19. The patient’s condition stabilized, with normal body temperature and reduced knee pain and effusion. Case 1 was discharged on day 40, and the triple antibiotic regimen continued for additional 4 weeks. The last outpatient follow-up occurred on day 95, revealing a return to light sports since 2 weeks before and an absence of symptoms related to the involved knee.
2) Case 2
On day 10, another arthrocentesis was performed, extracting 55 mL of the same bloody, slightly turbid fluid. The body temperature remained elevated. Levofloxacin (0.75 g/day) and SMZ-TMP (1.44 g/8 h) were initiated on day 11, due to the suspicion of S. maltophilia infection due to the use of the contaminated arthroscope. Bacterial culture results from the day 10 arthrocentesis later confirmed S. maltophilia infection. In subsequent days, the body temperature stabilized below 37 °C, and the knee effusion decreased. The patient was discharged on day 17, with instructions to continue SMZ-TMP and minocycline for an additional 4 weeks. At outpatient follow-up on day 46, the patient exhibited a normal gait and knee appearance, without any signs of knee pain, swelling, fever or other symptoms. No subsequent revisits were recorded.
3) Case 3
Upon confirmation of the positive S. maltophilia culture, the antibiotic protocol was promptly adjusted to levofloxacin (0.75 g/day) and SMZ-TMP (1.44 g/8 h). The following day, the body temperature decreased to a peak of 37.3 °C. Subsequently, the patient’s overall condition stabilized. Slight knee effusion persisted, but no additional discomfort was reported. Case 3 was discharged on day 22 with instructions to continue SMZ-TMP and minocycline for an additional 4 weeks. Regrettably, the patient did not return for a follow-up. However, a telephone survey later confirmed that he exhibited no signs of knee infection a month after discharge.
4) Case 4
On day 12, 40 mL of bloody joint fluid was extracted through arthrocentesis, and levofloxacin (0.75 g/day) and SMZ-TMP (1.44 g/8 h) were initiated. On day 16, microbiology reported a positive culture of S. maltophilia. Over the subsequent 10 days, the knee swelling gradually subsided. Case 4 was discharged on day 22 with a prescription for SMZ-TMP and minocycline to be continued for an additional 4 weeks. A soon clinic follow-up on day 25 revealed an absence of local symptoms. She did not return for subsequent revisits, but a telephone survey later confirmed her well-being a month after discharge.
The antibiotic protocols for the four patients are summarized in Table 3.
 Click to view | Table 3. Summary of the Antibiotic Protocols for Cases 1-4 |
| Discussion | ▴Top |
S. maltophilia has garnered increasing attention as a “rising concern” due to its escalating multidrug resistance and frequent clinical isolation [8]. Primarily as an opportunistic pathogen, it thrives in nosocomial environments, particularly among patients with immune deficiency, prolonged hospitalization, or a history of broad-spectrum antibiotic treatment [9]. Notably, there has been a surge in community-acquired infections as well [10-12]. The spectrum of S. maltophilia infections spans various systems within the human body, with a predominant association with the respiratory system [3, 13]. Infections affecting the bones, joints, and soft tissues are comparatively rare. Recent case reports have linked these infections to factors such as immunodeficiency syndrome [14], chemotherapy [15], post-trauma [5, 6], and community-acquired conditions [10, 12, 16].
To our knowledge, septic knee arthritis caused by S. maltophilia following arthroscopy has been sparsely documented, with only one instance reported by Pinol et al [7]. In that report, a 51-year-old man presented with knee pain, warmth, and swelling, without fever at 4 weeks post-meniscectomy, later diagnosed with septic knee arthritis. Despite the initial empirical use of ceftazidime and vancomycin, the condition remained uncontrolled. S. maltophilia isolation during arthroscopic debridement prompted a shift to SMZ-TMP. However, the situation only improved following two arthroscopic washouts and the addition of levofloxacin to the regimen. Strikingly, the characteristics and progression of this case closely paralleled that of case 1 in the current cases. Moreover, we conducted epidemiological investigation and comprehensive tests on all arthroscopic instruments. This diligent approach allowed us to trace the origin of S. maltophilia to a contaminated arthroscope. This discovery was significant, as it averted a potentially devastating outbreak of S. maltophilia infection. Furthermore, it played a crucial role in streamlining the treatment of all suspected patients, enabling the implementation of a proper antibiotic regimen ahead of or even with negative microbiology reports.
S. maltophilia is traditionally regarded as a pathogen with low virulence, although our understanding of its complete virulent characteristics remains limited [3, 9]. Recognized virulence factors, including pili, flagella, adhesins, and lipopolysaccharide, primarily contribute to its adherence and colonization on surfaces, as well as its resilience against antibiotics and immune responses. Additionally, the production of extracellular enzymes such as lipases, proteases, fibrinolysin, and esterase may contribute to cell damage and disruption of the immune system in infected hosts [3, 17]. In comparison to S. maltophilia, Staphylococcus aureus (S. aureus), the most common causative agent of knee septic arthritis across all age groups, exhibits higher virulence due to its cell wall, surface proteins, enzymes, and abundant toxins [18]. S. aureus infections often result in articular cartilage destruction and joint damage [19]. Notably, during the arthroscopic debridement of case 1, despite severe and widespread joint inflammation and sepsis, the articular cartilage remained intact. This observation aligns with the general impression of the low virulence of S. maltophilia. However, it is crucial to acknowledge that drawing definitive conclusions from a single case with short-term infection may be premature. Further studies are warranted to delve into various aspects of septic arthritis caused by S. maltophilia, including presentations, pathology, complications, and beyond.
As a multidrug-resistant organism, S. maltophilia is inherently resistant to most β-lactam agents and the aminoglycosides. In addition, it can also develop acquired resistance by obtaining other resistance determinants [3]. Traditionally, SMZ-TMP has been recommended as the first-line agent for treating S. maltophilia and has been widely utilized for years. Clinically, levofloxacin and minocycline have also proven to be effective [20]. However, controlled trials on the selection of antimicrobics are still lacking [21]. Unfortunately, the global rise in SMZ-TMP and levofloxacin-resistant strains is a concerning trend [22-24]. Reported resistance rates for SMZ-TMP can range from 26% to 50%. For levofloxacin, rates vary worldwide, from 10% in Hungary to 40% in pediatric patients in China [3, 9]. Minocycline has demonstrated excellent susceptibility to S. maltophilia, even in strains resistant to SMZ-TMP and levofloxacin [25]. In addition, it exhibited minimal drug-drug interactions and a relatively good tolerability profile [26], suggesting minocycline to be a valuable therapeutic option for S. maltophilia infection. In our cases, double or triple combinations of these agents were applied based on the severity of infection and individual tolerance, resulting in satisfactory outcomes for all patients. A timely discovery and management of infection are crucial. For cases 2-4, in whom infections were identified soon after onset, antibiotic drugs alone were effective in controlling the condition. In comparison, rigorous debridement, washout, and continuous irrigation of the joint cavity were equally important for a delayed and more severe condition, as observed in case 1.
The contaminated arthroscope played a significant role in the nosocomial infection series. Regrettably, due to limited research conditions, further investigations such as gene sequencing and a comparison of isolated S. maltophilia strains, were not conducted. The source of contamination for the arthroscope remains unknown. Previous studies suggest that S. maltophilia can originate from various nosocomial sources, including hospital water, nebulizers, dialysis machines, catheters, blood gas analyzers, ventilator circuits, thermometers, and the hands of hospital personnel [9]. It is possible that the contamination occurred during the cleaning process, followed by an unsuccessful sterilization attempt. Despite being labeled as autoclavable, the contaminated arthroscope was proven to have a damaged airtightness by steam leak-in during an autoclave test, which may be related to a glass replace history months ago. It was speculated that S. maltophilia entered and colonized in glass cavities of the scope through the compromised seal, escaping sterilization and finally spread into joints intraoperatively. S. maltophilia features with the ability of biofilm formation, if any in the scope, made the organism more difficult to be eradicated. Conclusively, we hypothesize that a compromised seal of the arthroscope is a high-risk factor for contamination, a theory that warrants further investigation.
As mentioned earlier, HPGP sterilization was routinely used in our facility for arthroscopes, as well as other rigid endoscopes like laparoscopes and ureteroscopes, etc. Despite the autoclavable capability of arthroscopes, we observed accelerated wear when autoclaving compared to low-temperature sterilization. HPGP sterilization has been widely utilized for various types of lumen devices for over two decades [27, 28]. In fact, high-level disinfection had been deemed sufficient for reprocessing endoscopes with little risk of infection before the introduction of HPGP sterilization in the 1990s [29]. Although HPGP sterilization is known for its speed, safety, and non-toxicity, it has poor penetration power [30]. Endoscopes are recommended to undergo testing for seal and leaks before any disinfection or sterilization process [30]. However, microcracks and leaks are challenging to detect through visual examination alone, especially at junction sites. Therefore, periodic tests of arthroscope airtightness are highly recommended to ensure the reliability of low-temperature sterilization. Careful inspection and cleaning of arthroscopes after debridement surgeries are required. Using clean water for instrument cleaning is also important [31]. Future studies are still suggested to explore more effective means for arthroscope reprocessing.
One interesting phenomenon in these incidents was a higher susceptibility to S. maltophilia infection in patients who underwent meniscectomy or meniscus repair compared to those undergoing ACLR (75% and 66.7% vs. 12.5%, respectively). It is essential to acknowledge that this is an observed phenomenon rather than a conclusive finding, given the limited sample size. Theoretically, ACLR involves longer operation time, causes larger trauma, and implants a tendon graft inside the joint, all of which could contribute to a higher vulnerability to infection. However, we did not find a clear explanation during our investigation. Several presumptions were proposed: 1) Prophylactic antibiotics, such as cefazolin or cefuroxime, were routinely administered for 24 h before and after ACLR as part of our regimen, but not for sole meniscus surgeries. It is possible that these prophylactic antibiotics somehow eliminate intraoperative infections. However, given S. maltophilia’s inherent resistance to β-lactam antibiotics, the actual effectiveness of these prophylactic agents is questionable. 2) We routinely perform a thorough washout of the knee cavity using a large amount of normal saline at the end of ACLR to reduce the risk of infection, a practice not strictly employed for meniscus surgeries. This might indeed contribute to the lower infection rate. 3) ACLR typically involves more bleeding and a higher chance of hemarthrosis postoperatively. However, white blood cells entering the knee cavity with bleeding may play a role in eliminating microorganisms. Nevertheless, it should be noted that these are mere presumptions based on observations from a limited number of cases and have not been validated.
There are several limitations in the current study. Firstly, due to practical constraints, not all patients could be examined in person during this period; many were followed up only by telephone. Secondly, in our infection control investigation, we focused solely on sampling and testing surgical instruments, omitting other materials in contact with the surgical field, such as drapes, films, gowns, gloves, and items like shaver blades and coblation wands. Additionally, environmental factors such as suction channels, air vents, the instrument reprocessing area, water sources, sinks, and equipment were not included in the testing. Although we identified the arthroscope as the source of contamination, we did not conduct a gene-level comparison between the isolated strains from infected patients and the contaminated arthroscope. This limitation highlights the less rigorous nature of our infection control investigation. Thirdly, the exact cause of arthroscope contamination is unclear. Our hypothesis stems from the arthroscope’s repair history, steam autoclave test, and speculations. A more definitive conclusion could be reached with laboratory tests and controlled experiments.
Conclusion
Although S. maltophilia is a very rare cause of knee septic arthritis in immunocompetent individuals, it can still occur and even lead to nosocomial outbreaks through instrument-related transmission. Routine close inspection and examination of postoperative patients should be conducted to detect any early signs of infection. SMZ-TMP, levofloxacin, and minocycline remain the treatment of choice for S. maltophilia, despite the rising global resistance rates to these agents. While low-temperature HPGP serves as a fast and effective method for instrument sterilization in arthroscopy, maintaining good airtightness of arthroscopes may be key to guaranteeing success and should be periodically checked.
Learning points
1) Routinely inspect arthroscopes before and after use for debridement surgery. Do not reuse a scope without prior quality check if it has been used in debridement.
2) Do not reuse a scope without rigorous quality inspection if it has been repaired.
3) Use clean water for instrument cleaning and sterilization. Autoclave is recommended for sterilizing the arthroscope after debridement, provided it is deemed safe by the manufacturer.
4) Perform routine wash after arthroscopic surgeries, even for simple meniscus procedures.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
As a retrospective and descriptive study of case series and investigation, the current study has been granted exemption from approval by the ethics committee of the authors’ institute. Written consents reviewed by the ethics committee were obtained from all patients, granting access to their clinical data and medical record for research purpose and scientific publication under privacy protection.
Author Contributions
LY: original draft, review and editing of the manuscript, and methodology; SY: review and editing of the manuscript; DFL: conduction of investigation and data curation; WJY: patient treatment and data curation; JBL: statistics and data analysis; BD: project administration and supervision.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
ACL: anterior cruciate ligament; ACLR: anterior cruciate ligament reconstruction; HPGP: hydrogen peroxide gas plasma; LFC: lateral femoral condyle; LM: lateral meniscus; MFC: medial femoral condyle; MM: medial meniscus; S. aureus: Staphylococcus aureus; S. maltophilia: Stenotrophomonas maltophilia; SMZ-TMP: sulfamethoxazole-trimethoprim
| References | ▴Top |
- Umar Z, Ilyas U, Ashfaq S, Bhangal R, Nassar M. Stenotophomonas maltophilia as not just a mere colonozer: two cases of urinary tract infection and multidrug-resistant respiratory infection. Cureus. 2022;14(3):e23541.
doi pubmed - Falagas ME, Valkimadi PE, Huang YT, Matthaiou DK, Hsueh PR. Therapeutic options for Stenotrophomonas maltophilia infections beyond co-trimoxazole: a systematic review. J Antimicrob Chemother. 2008;62(5):889-894.
doi pubmed - Mojica MF, Humphries R, Lipuma JJ, Mathers AJ, Rao GG, Shelburne SA, Fouts DE, et al. Clinical challenges treating Stenotrophomonas maltophilia infections: an update. JAC Antimicrob Resist. 2022;4(3):dlac040.
doi pubmed - Rajkumari N, Mathur P, Gupta AK, Sharma K, Misra MC. Epidemiology and outcomes of Stenotrophomonas maltophilia and Burkholderia cepacia infections among trauma patients of India: a five year experience. J Infect Prev. 2015;16(3):103-110.
doi pubmed - Osakwe N. Osteomyelitis due to Stenotrophomonas maltophilia treated with trimethoprim-sulfamethoxazole monotherapy. IDCases. 2023;32:e01798.
doi pubmed - Chesnutis EJ, 3rd, Ng A, Kruse D, Stone PA. Stenotrophomonas maltophilia: a rare case of osteomyelitis after an open distal tibial fracture. J Foot Ankle Surg. 2018;57(5):1037-1041.
doi pubmed - Pinol I, Alier A, Hinarejos P, Sorli ML, Puig L. [Septic arthritis of the knee by Stenotrophomonas maltophilia]. Rev Esp Quimioter. 2012;25(3):218-219.
pubmed - Johnson AP, Duckworth GJ. The emergence of Stenotrophomonas maltophilia. BMJ. 2008;336(7657):1322.
doi pubmed - Senol E. Stenotrophomonas maltophilia: the significance and role as a nosocomial pathogen. J Hosp Infect. 2004;57(1):1-7.
doi pubmed - Aydemir C, Aktas E, Eldes N, Kutsal E, Demirel F, Ege A. Community-acquired infection due to Stenotrophomonas maltophilia: a rare cause of septic arthritis. Turk J Pediatr. 2008;50(1):89-90.
pubmed - Falagas ME, Kastoris AC, Vouloumanou EK, Dimopoulos G. Community-acquired Stenotrophomonas maltophilia infections: a systematic review. Eur J Clin Microbiol Infect Dis. 2009;28(7):719-730.
doi pubmed - Wang G, Xu N, Yang L, Zheng F, Sai L, Zhou J, Yang S. Community acquired Stenotrophomonas maltophilia discitis: Diagnosis aided by shotgun metagenomic sequencing. Int J Infect Dis. 2019;81:1-3.
doi pubmed - Samonis G, Karageorgopoulos DE, Maraki S, Levis P, Dimopoulou D, Spernovasilis NA, Kofteridis DP, et al. Stenotrophomonas maltophilia infections in a general hospital: patient characteristics, antimicrobial susceptibility, and treatment outcome. PLoS One. 2012;7(5):e37375.
doi pubmed - Belzunegui J, De Dios JR, Intxausti JJ, Iribarren JA. Septic arthritis caused by Stenotrophomonas maltophilia in a patient with acquired immunodeficiency syndrome. Clin Exp Rheumatol. 2000;18(2):265.
pubmed - Teo WY, Chan MY, Lam CM, Chong CY. Skin manifestation of Stenotrophomonas maltophilia infection—a case report and review article. Ann Acad Med Singap. 2006;35(12):897-900.
pubmed - Thomas J, Prabhu VN, Varaprasad IR, Agrawal S, Narsimulu G. Stenotrophomonas maltophilia: a very rare cause of tropical pyomyositis. Int J Rheum Dis. 2010;13(1):89-90.
doi pubmed - Brooke JS. Advances in the Microbiology of Stenotrophomonas maltophilia. Clin Microbiol Rev. 2021;34(3):e0003019.
doi pubmed - Jin T, Mohammad M, Pullerits R, Ali A. Bacteria and host interplay in staphylococcus aureus septic arthritis and sepsis. Pathogens. 2021;10(2):158.
doi pubmed - Alder KD, Lee I, Munger AM, Kwon HK, Morris MT, Cahill SV, Back J, et al. Intracellular Staphylococcus aureus in bone and joint infections: A mechanism of disease recurrence, inflammation, and bone and cartilage destruction. Bone. 2020;141:115568.
doi pubmed - Chung HS, Hong SG, Kim YR, Shin KS, Whang DH, Ahn JY, Park YJ, et al. Antimicrobial susceptibility of stenotrophomonas maltophilia isolates from Korea, and the activity of antimicrobial combinations against the isolates. J Korean Med Sci. 2013;28(1):62-66.
doi pubmed - Andelkovic MV, Jankovic SM, Kostic MJ, Zivkovic Zaric RS, Opancina VD, Zivic MZ, Milosavljevic MJ, et al. Antimicrobial treatment of Stenotrophomonas maltophilia invasive infections: Systematic review. J Chemother. 2019;31(6):297-306.
doi pubmed - Hu LF, Chen GS, Kong QX, Gao LP, Chen X, Ye Y, Li JB. Increase in the Prevalence of Resistance Determinants to Trimethoprim/Sulfamethoxazole in Clinical Stenotrophomonas maltophilia Isolates in China. PLoS One. 2016;11(6):e0157693.
doi pubmed - Wang CH, Yu CM, Hsu ST, Wu RX. Levofloxacin-resistant Stenotrophomonas maltophilia: risk factors and antibiotic susceptibility patterns in hospitalized patients. J Hosp Infect. 2020;104(1):46-52.
doi pubmed - Herrera-Heredia SA, Pezina-Cantu C, Garza-Gonzalez E, Bocanegra-Ibarias P, Mendoza-Olazaran S, Morfin-Otero R, Camacho-Ortiz A, et al. Risk factors and molecular mechanisms associated with trimethoprim-sulfamethoxazole resistance in Stenotrophomonas maltophilia in Mexico. J Med Microbiol. 2017;66(8):1102-1109.
doi pubmed - Patterson SB, Mende K, Li P, Lu D, Carson ML, Murray CK, Tribble DR, et al. Stenotrophomonas maltophilia infections: Clinical characteristics in a military trauma population. Diagn Microbiol Infect Dis. 2020;96(2):114953.
doi pubmed - Gibb J, Wong DW. Antimicrobial treatment strategies for stenotrophomonas maltophilia: a focus on novel therapies. Antibiotics (Basel). 2021;10(10):1226.
doi pubmed - Wang J, Zhang B, Sun H, Zhang J, Duan H, Ban H, Shen J, et al. Monitoring the effective sterilization of low-temperature hydrogen peroxide gas plasma sterilizers in 58 hospitals - 22 PLADs, China, June 2015-December 2019. China CDC Wkly. 2021;3(29):624-626.
doi pubmed - Okpara-Hofmann J, Knoll M, Durr M, Schmitt B, Borneff-Lipp M. Comparison of low-temperature hydrogen peroxide gas plasma sterilization for endoscopes using various Sterrad models. J Hosp Infect. 2005;59(4):280-285.
doi pubmed - Ayliffe GA, Babb JR, Bradley CR. 'Sterilization' of arthroscopes and laparoscopes. J Hosp Infect. 1992;22(4):265-269.
doi pubmed - Rutala WA. Guideline for disinfection and sterilization in healthcare facilities, 2008. Available from: https://www.cdc.gov/infectioncontrol/guidelines/disinfection/. Access date: April 18, 2025.
- Jain MJ, Mavani K. Lethal necrotizing fasciitis triggered by plaster: case report and review of literature. J Orthop Case Rep. 2016;6(5):73-75.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.