| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 6, June 2025, pages 222-225
Splenic Vein Thrombosis, Non-Cirrhotic Portal Hypertension, and Gastric Varices in a Patient With Ovarian Carcinoma
Taylor Bowlera, Lyubov Tiegsa, Bryant Megnaa, b, Nabeel Azeemb, c
aDepartment of Internal Medicine, University of Minnesota Medical Center, Minneapolis, MN, USA
bDivision of Gastroenterology, Hepatology, and Nutrition, University of Minnesota Medical Center, Minneapolis, MN, USA
cCorresponding Author: Nabeel Azeem, Division of Gastroenterology, Hepatology, and Nutrition, University of Minnesota Medical Center, Minneapolis, MN 55455, USA
Manuscript submitted March 14, 2025, accepted June 6, 2025, published online June 16, 2025
Short title: SVT and NCPH
doi: https://doi.org/10.14740/jmc5127
| Abstract | ▴Top |
The development of non-cirrhotic portal hypertension and esophagogastric varices is an uncommon, yet life-threatening complication of splenic vein thrombosis. Recognizing this association between splenic vein thrombosis and non-cirrhotic portal hypertension is critical in reducing morbidity and mortality in patients with hypercoagulable disease secondary to malignancy. Herein, we present a 45-year-old female with stage IV high-grade serous ovarian carcinoma and chronic splenic vein thrombosis found to have life-threatening esophagogastric varices secondary to non-cirrhotic portal hypertension.
Keywords: Splenic vein thrombosis; Portal hypertension; Gastric varix
| Introduction | ▴Top |
Ovarian carcinoma has one of the highest rates of venous thromboembolism compared to other solid tumors due to the hypercoagulable nature of the disease and its treatment options [1]. While several studies have explored deep venous thrombosis and pulmonary emboli in this patient population, data are limited regarding splenic vein thrombosis in patients with ovarian carcinoma specifically.
Splenic vein thrombosis is usually an asymptomatic phenomenon without sequelae. However, the development of non-cirrhotic portal hypertension is a rare, yet life-threatening complication, more often seen in patients with severe pancreatitis given the proximity of the splenic vasculature. Portal hypertension poses a high mortality risk due to the formation of collateral pathways that shunt blood towards the submucosal veins of the gastric fundus, thus increasing the potential for variceal rupture and hemorrhage [2]. In circumstances where splenic vein thrombosis precipitates portal hypertension, it is imperative to identify the underlying cause of thrombus formation, treat the thrombosis itself, and manage its potential complications including varices. Overall, recognizing this association between splenic vein thrombosis and non-cirrhotic portal hypertension is critical in reducing morbidity and mortality in patients with hypercoagulable disease such as malignancy.
In this report, we highlight a patient with stage IV ovarian carcinoma who presented with abdominal pain and was subsequently found to have a life-threatening gastric variceal bleed in the setting of non-cirrhotic portal hypertension precipitated by a chronic splenic vein thrombosis.
| Case Report | ▴Top |
A 45-year-old female with past medical history notable for stage IV high-grade serous ovarian carcinoma, chronic splenic vein thrombosis on apixaban, history of small bowel obstruction, ruptured appendix, and gastroesophageal reflux disease presented with cramping abdominal pain and constipation for 3 days. Symptoms were consistent with prior episodes of small bowel obstructions per patient report. Hemoglobin on admission was notable for 9.4 g/dL (normal range 11.7 to 15.7 g/dL). Computed tomography (CT) of abdomen/pelvis was notable for dilated small bowel with large stool burden in the right and transverse colon, mild steatosis without cirrhotic changes in the liver, chronic thrombosis in the mid to distal splenic vein and splenomegaly (14.2 cm) (Fig. 1a). Treatment was initiated for a presumed small bowel obstruction. Approximately 24 h after hospital admission, the patient developed vomiting with 150 mL of hematemesis with a precipitous hemoglobin drop to 7.4 g/dL. The hemoglobin was 5.9 g/dL 6 h later. Gastroenterology was then consulted for further evaluation.
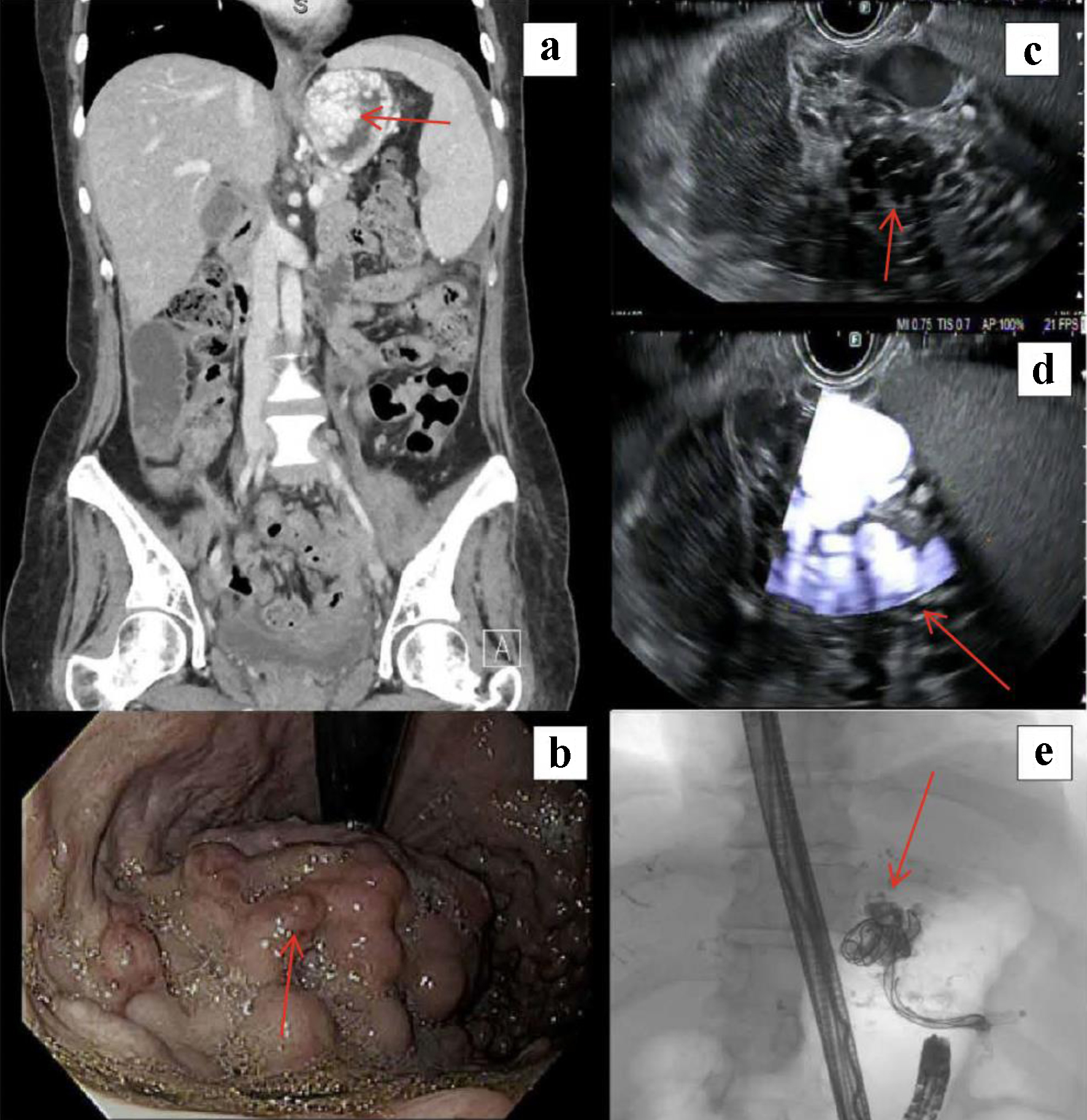 Click for large image | Figure 1. (a) Computed tomography of the abdomen/pelvis demonstrating splenomegaly and dilated collaterals in the proximal stomach (arrow). (b) Upper endoscopy with high-risk variceal stigmata (red wale signs, arrow). (c) Endoscopic ultrasound sonographic image of variceal bundle in gastric wall (arrow). (d) Doppler image of variceal bundle demonstrating significant inflow (arrow). (e) Fluoroscopic image post-embolization. Visible vascular coils and lipiodol mixture within the body of the largest variceal bundle as well as the inflow tract from the splenic hilum (arrow). |
An esophagogastroduodenoscopy (EGD) was performed and showed grade C esophagitis in the mid-esophagus, large > 5 mm esophageal varices, a small gastric erosion without stigmata of bleeding, and type 2 gastroesophageal varices (GOV-2) suspected to be the bleeding source (Fig. 1b). The patient was initiated on an octreotide drip and underwent an upper endoscopy with ultrasound (EUS). EUS demonstrated type 2 isolated gastric varices in the fundus, measuring up to 13.3 mm at the inflow tract as it crossed the gastric wall and originated from the splenic hilum (Fig. 1c, d). The largest varix projecting from the splenic hilum was targeted just prior to entry into the stomach wall fundus. The fundal varix was punctured with a 19-gauge fine-needle aspirate (FNA). Three 0.035-inch vascular coils (15 mm in diameter and 20 cm long; Azur CX, Terumo Medical Corporation, Somerset, NJ) were advanced into the varix followed by injection of 1 mL of 1:1 lipiodol/histoacryl solution with endosonographic evidence of variceal obliteration (Fig. 1e). The apex of the main gastric varix was also punctured with a 19-gauge FNA needle followed by injection of 1 mL of 1:1 solution with evidence of variceal obliteration. Interventional radiology was consulted in the post-operative period for consideration of splenic artery embolization or splenic reduction to aid in gastric variceal decompression. A multidisciplinary decision was made to defer further interventions due to known splenic metastases with increased risk of abscess formation. The patient was discharged with plans for repeat endoscopic ultrasound to achieve eradication of the remaining variceal bundle. Unfortunately, the procedure was not performed as the patient was hospitalized for a rectovaginal fistula and transitioned to hospice shortly thereafter.
| Discussion | ▴Top |
While several studies have highlighted this phenomenon in patients with pancreatic adenocarcinoma and severe pancreatitis, few reports have explored splenic vein thrombosis in patients with ovarian carcinoma given that it is relatively uncommon amongst non-gastrointestinal malignancies [3]. Specifically, a retrospective study by Shang et al outlined that the prevalence of splenic vein thrombosis in patients with non-gastrointestinal malignancies is less than 0.4% [4]. This case demonstrates the importance of casting a broad differential when managing patients with hypercoagulable diseases given the potential need for intervention to prevent future decompensation in those with underlying non-cirrhotic portal hypertension secondary to splenic vein thrombosis. Reassuringly, there were minimal delays between the diagnosis of upper gastrointestinal bleed, assessment with endoscopy, and subsequent obliteration of varices in this patient’s case.
The potential sequelae of chronic splenic vein thrombosis raise concern about the effectiveness of anticoagulation as an alternative treatment to splenectomy. Splenectomy is currently considered standard therapy for symptomatic patients with splenic venous thrombosis as this intervention addresses the problem itself and its downstream complications [5, 6]. However, surgical intervention bears its own risks in patients with cancer specifically, including seeding tumor within the peritoneum and developing infection in the setting of immunosuppression [5]. On the other hand, anticoagulation only serves as a temporizing measure with no guaranteed resolution of the clot, thereby increasing the risk for life-threatening variceal hemorrhage as seen in this patient’s case. Despite these risks, anticoagulation with direct oral anticoagulants is appealing to both patient and physician due to ease of oral administration and absence of laboratory monitoring [7]. This predicament highlights the need for ongoing investigation into the preferred treatment for splenic vein thrombosis in patients who are susceptible to high clot burden and consequential non-cirrhotic portal hypertension. Future studies should consider the utility of surveillance with Doppler abdominal ultrasound or EGD in these high-risk patients to decrease morbidity and mortality [5].
This case highlights that patients with ovarian carcinoma are at risk of developing splenic vein thrombosis due to the hypercoagulable nature of their disease. It is critical to consider the potential sequelae of non-cirrhotic portal hypertension to assure early intervention and mitigate risk of a life-threatening gastric variceal hemorrhage as seen in our patient.
Learning points
Splenic vein thrombosis is usually an asymptomatic phenomenon without sequelae.
The development of non-cirrhotic portal hypertension is a rare, yet life-threatening complication of splenic vein thrombosis.
Patients with ovarian carcinoma are also at risk of developing splenic vein thrombosis due to the hypercoagulable nature of their disease.
Recognizing this association between splenic vein thrombosis and non-cirrhotic portal hypertension is critical in reducing morbidity and mortality in patients with hypercoagulable disease such as malignancy.
Acknowledgments
This abstract was presented at American College of Gastroenterology Annual Meeting in Pennsylvania in October 2024.
Financial Disclosure
None to declare.
Conflict of Interest
NA is a consultant for Boston Scientific.
Informed Consent
Informed consent was obtained for this case report.
Author Contributions
BM: study conception, image selection, and final review of manuscript. NA: final review of manuscript. TB and LT: writing, literature review, critical appraisal, and final review of manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Weeks K, Herbach E, McDonald M, Charlton M, Schweizer ML. Meta-analysis of VTE risk: ovarian cancer patients by stage, histology, cytoreduction, and ascites at diagnosis. Obstet Gynecol Int. 2020;2020:2374716.
doi - Guixe-Muntet S, Quesada-Vazquez S, Gracia-Sancho J. Pathophysiology and therapeutic options for cirrhotic portal hypertension. Lancet Gastroenterol Hepatol. 2024;9(7):646-663.
doi pubmed - Nguyen KB, Zhang DM, Sultenfuss MM, Victor DIM. Massive gastric variceal hemorrhage due to splenic vein thrombosis: a rare initial presentation of asymptomatic metastatic pancreatic adenocarcinoma. Am J Gastroenterol. 2018;113:S1357.
- Shang H, Jiang JY, Guffey D, Novoa F, Bandyo R, Ma S, Li A. Natural history of cancer-associated splanchnic vein thrombosis. J Thromb Haemost. 2024;22(5):1421-1432.
doi pubmed - Hayashi H, Shimizu A, Motoyama H, Kubota K, Notake T, Ikehara T, Yasukawa K, et al. Left-sided portal hypertension caused by idiopathic splenic vein stenosis improved by splenectomy: a case report. Surg Case Rep. 2020;6(1):148.
doi pubmed - Paramythiotis D, Papavramidis TS, Giavroglou K, Potsi S, Girtovitis F, Michalopoulos A, Papadopoulos VN, et al. Massive variceal bleeding secondary to splenic vein thrombosis successfully treated with splenic artery embolization: a case report. J Med Case Rep. 2010;4:139.
doi pubmed - Hicks AM, DeRosa A, Raj M, Do R, Yu KH, Lowery MA, Varghese A, et al. Visceral thromboses in pancreas adenocarcinoma: systematic review. Clin Colorectal Cancer. 2018;17(2):e207-e216.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.