| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 2, February 2025, pages 82-86
Long-Term Outcomes and Management of Atypical Carotid Web in Nonagenarian
Daniel L. Burkea, Aldin Malkoca, b, c, Iden Andacheha
aDivision of Vascular Surgery, Department of Surgery, Kaiser Permanente Fontana Medical Center, Fontana, CA 92335, USA
bDivision of Vascular Surgery, Department of Surgery, Arrowhead Regional Medical Center, Colton, CA 92324, USA
cCorresponding Author: Aldin Malkoc, Arrowhead Regional Medical Center, Colton, CA 92324, USA
Manuscript submitted September 30, 2024, accepted December 4, 2024, published online February 2, 2025
Short title: Management of Carotid Webs
doi: https://doi.org/10.14740/jmc4339
| Abstract | ▴Top |
Internal carotid artery webs (ICAWs) have been described as noninflammatory, nonatherosclerotic shelf-like projections of intimal fibrous tissue which may be the culprit for embolic stroke of unknown origin. Carotid webs are an atypical form of intimal fibromuscular dysplasia (FMD) and internal carotid webs create areas of stagnation and recirculation distal to the web that favor thrombus formation and embolism. Symptomatic carotid webs are conventionally associated with young women presenting with few vascular risk factors and < 50% stenosis in the affected ICA. ICAWs are being described more and more in the vascular literature, but the management of this pathology remains unclear. We describe a rare case of a 90-year-old male who presented with a significantly sclerosed symptomatic right ICAW without evidence of comorbid atherosclerotic disease. The clinical management, intraoperative findings, and postoperative course are described herein. At the age of 90, this patient is the oldest case of symptomatic carotid web recorded in the literature. Successful management with a carotid endarterectomy is an appropriate strategy for treatment even in a nonagenarian. We would favor carotid endarterectomy over carotid artery stenting given the circumferential, fibrotic nature of these lesions.
Keywords: Carotid; Carotid web; Fibromuscular dysplasia; Endarterectomy
| Introduction | ▴Top |
Ischemic stroke (IS) is a significant source of morbidity and mortality, with embolic stroke of unknown origin (ESUS) representing approximately 16% of all cases [1, 2]. ESUS is a controversial designation reserved for non-lacunar infarcts in the absence of cardioembolic risk factors, hemodynamically significant atherosclerotic stenosis in the vessels supplying the infarcted region, or another definitive mechanism of ischemia [2, 3]. Within recent years, webs of the internal carotid artery (ICA), presenting as noninflammatory, nonatherosclerotic shelf-like projections of intimal fibrous tissue, have been proposed as a possible mechanism for ESUS [4, 5]. Carotid webs are an atypical form of intimal fibromuscular dysplasia (FMD), a systemic vascular disorder that can manifest as several pathologies, including hypertension, renal insufficiency, large vessel aneurysm, and dissection. Internal carotid webs create areas of stagnation and recirculation distal to the web that favor thrombus formation and embolism [6, 7]. Symptomatic carotid webs are conventionally associated with young women presenting with few vascular risk factors and < 50% stenosis in the affected ICA. We describe lesion progression in a 90-year-old man with an extensive past medical history (PMH) and chronic antithrombotic monotherapy who presented with a significantly stenosed symptomatic right proximal ICA web (ICAW) without evidence of comorbid atherosclerotic disease.
| Case Report | ▴Top |
A 90-year-old male with a PMH of bilateral moderate ICA stenosis (50-79%) presented to the emergency department (ED) from his primary care physician for an emergent vascular consult following a suspected transient ischemic attack. Patient was previously noted to have moderate carotid stenoses and had been followed by vascular surgery. Due to the asymptomatic nature and the patient’s age, we elected to watch the lesion. However, the lesion became symptomatic. One week prior, he experienced an episode of right transient monocular blindness with lingering vision changes. He denied any dizziness, headache, focal weakness, speech deficits, hemiparesis, or loss of consciousness. His PMH was significant for hypertension, type 2 diabetes mellitus, hyperlipidemia, deep vein thrombosis, diastolic heart failure, and atrial fibrillation. He had a 12.50 pack-year smoking history, and reports that he quit smoking 45 years prior. Carotid duplex ultrasound performed the day prior to his ED visit demonstrated 50-79% stenosis in the bilateral ICAs with broad-based filling defects and hyperechoic intraluminal components in the internal bulbs (Fig. 1). Head and neck computed tomography angiography (CTA) revealed 80% stenosis in the proximal right ICA and 65% stenosis in the left ICA, with no evidence of acute infarct or intracranial lesions (Fig. 2). On physical exam, he did not demonstrate acute neurological deficits suggestive of a stroke, and his cardiopulmonary exam was benign and consistent with his PMH.
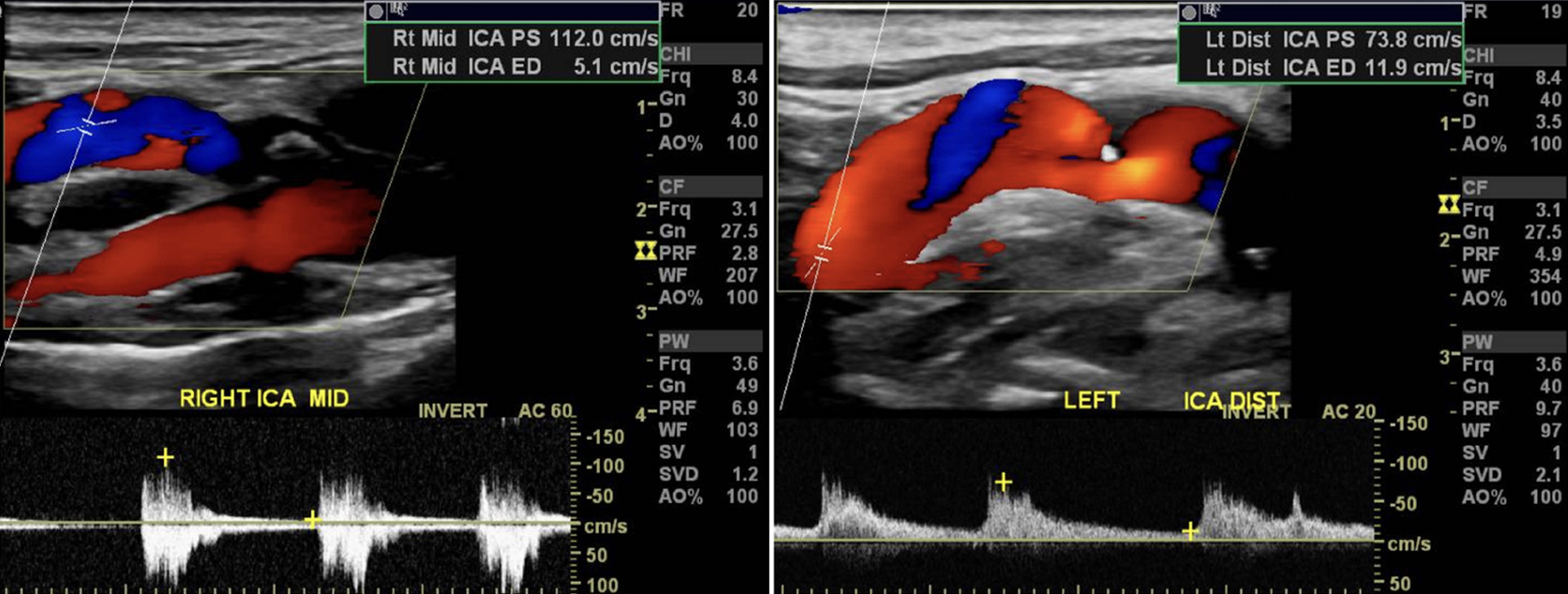 Click for large image | Figure 1. Carotid duplex ultrasound of left and right ICA showing filling defects and stenosis. ICA: internal carotid artery. |
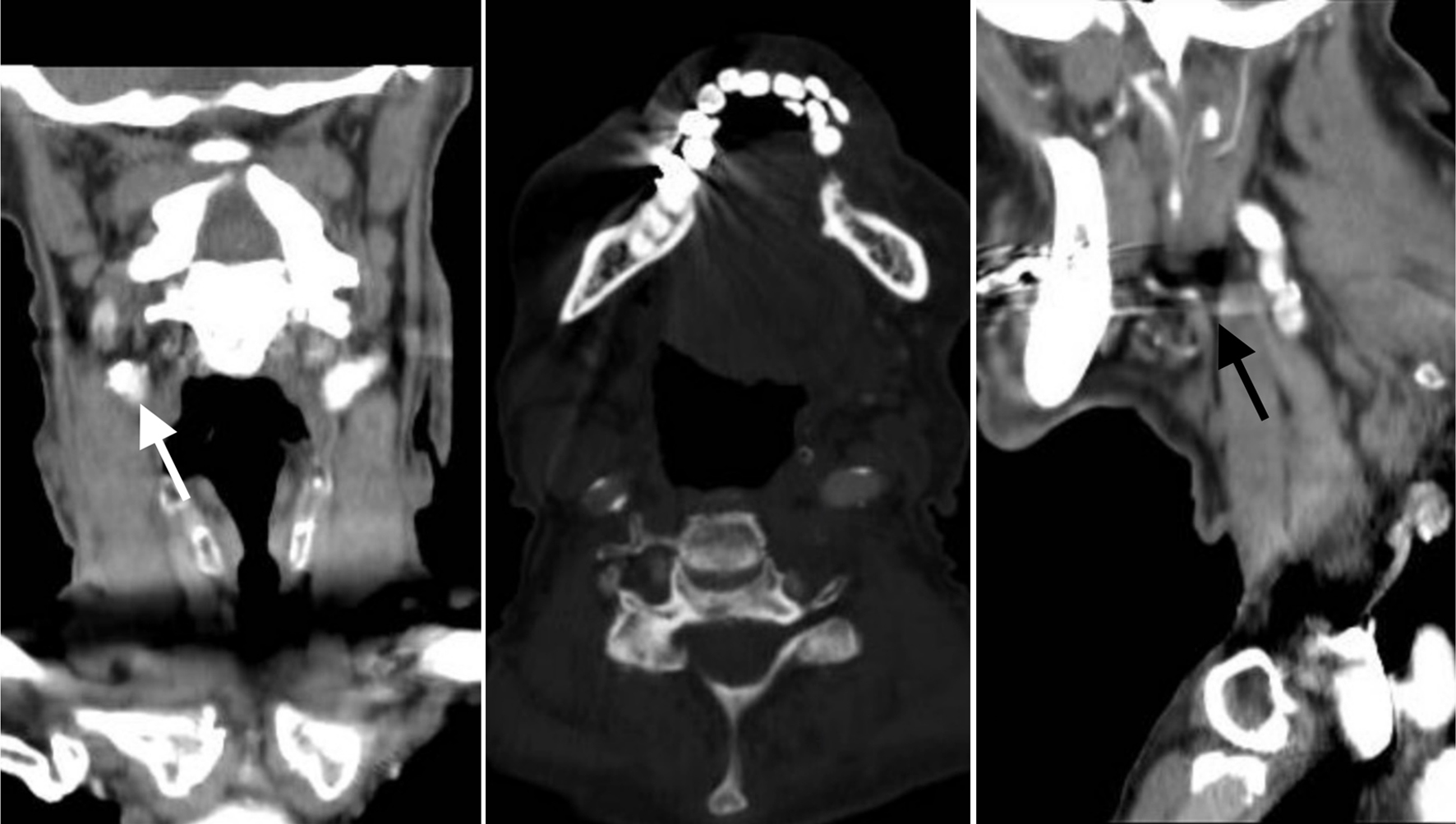 Click for large image | Figure 2. Coronal, sagittal, and axial views highlighting the right common and external carotid artery segments appear normal. There is approximately 80% stenosis of the proximal right internal carotid artery (white arrow). There is hypo-enhancement of the distal right internal carotid artery (black arrow). |
The patient was discharged home with 81 mg aspirin daily and scheduled for an elective right carotid endarterectomy (CEA). Intraoperatively, a web was identified in the proximal right ICA with some mild evidence of atherosclerotic plaque; lesion was circumferential, fibrotic, and near occlusive with a pine-hole like opening (Figs. 3 and 4). Following endarterectomy, the vessel was patched with bovine pericardium and 6-0 Prolene suture. The patient tolerated the procedure well, and his immediate postoperative neurological exam demonstrated no deficits. His postoperative hospitalization was uneventful, and he was discharged on post-operative day 2 on apixaban 5 mg and 81 mg aspirin daily for anticoagulation given his PMH of chronic atrial fibrillation. At 1-month and 13-month follow-ups, the patient denied any episodes of vision loss, slurred speech, loss of consciousness, or new paresthesia since his CEA. A carotid duplex ultrasound performed at 13 months post-operation demonstrated minimal disease (1-15%) in the right ICA with no evidence of filling defects.
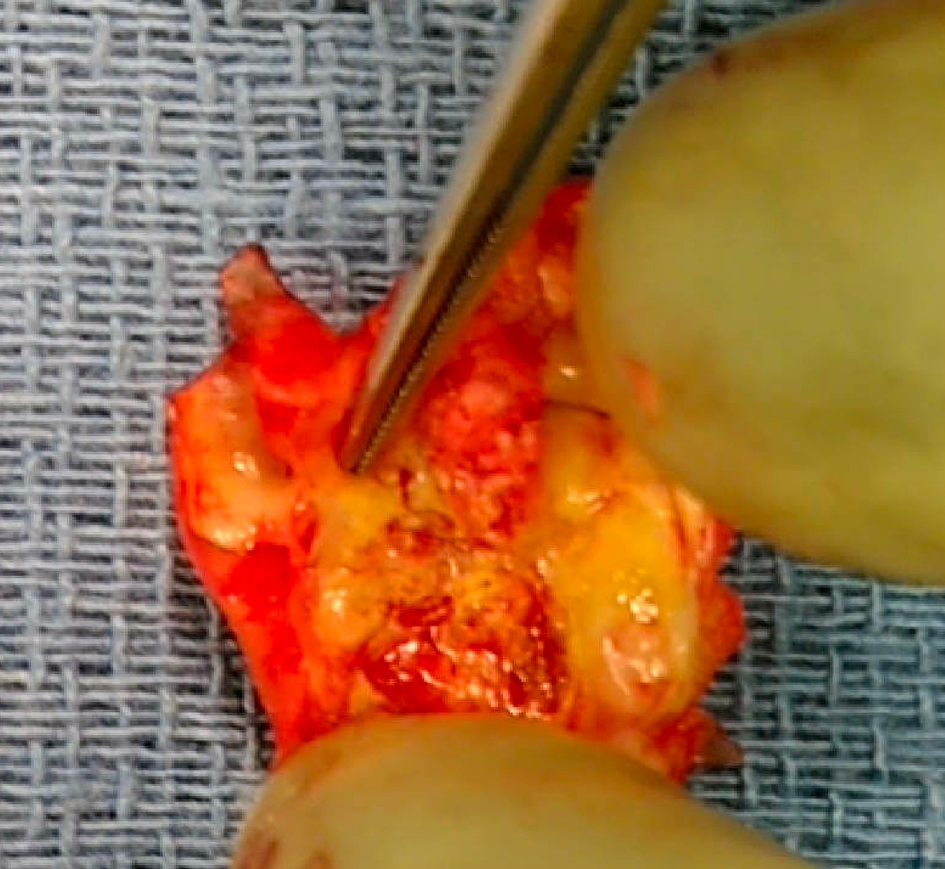 Click for large image | Figure 3. Intraoperative photo of excised section of right proximal internal carotid artery with the presence of a fibrous band protruding from the posterior lumen. Note the absence of an atheroma characteristic of atherosclerosis. |
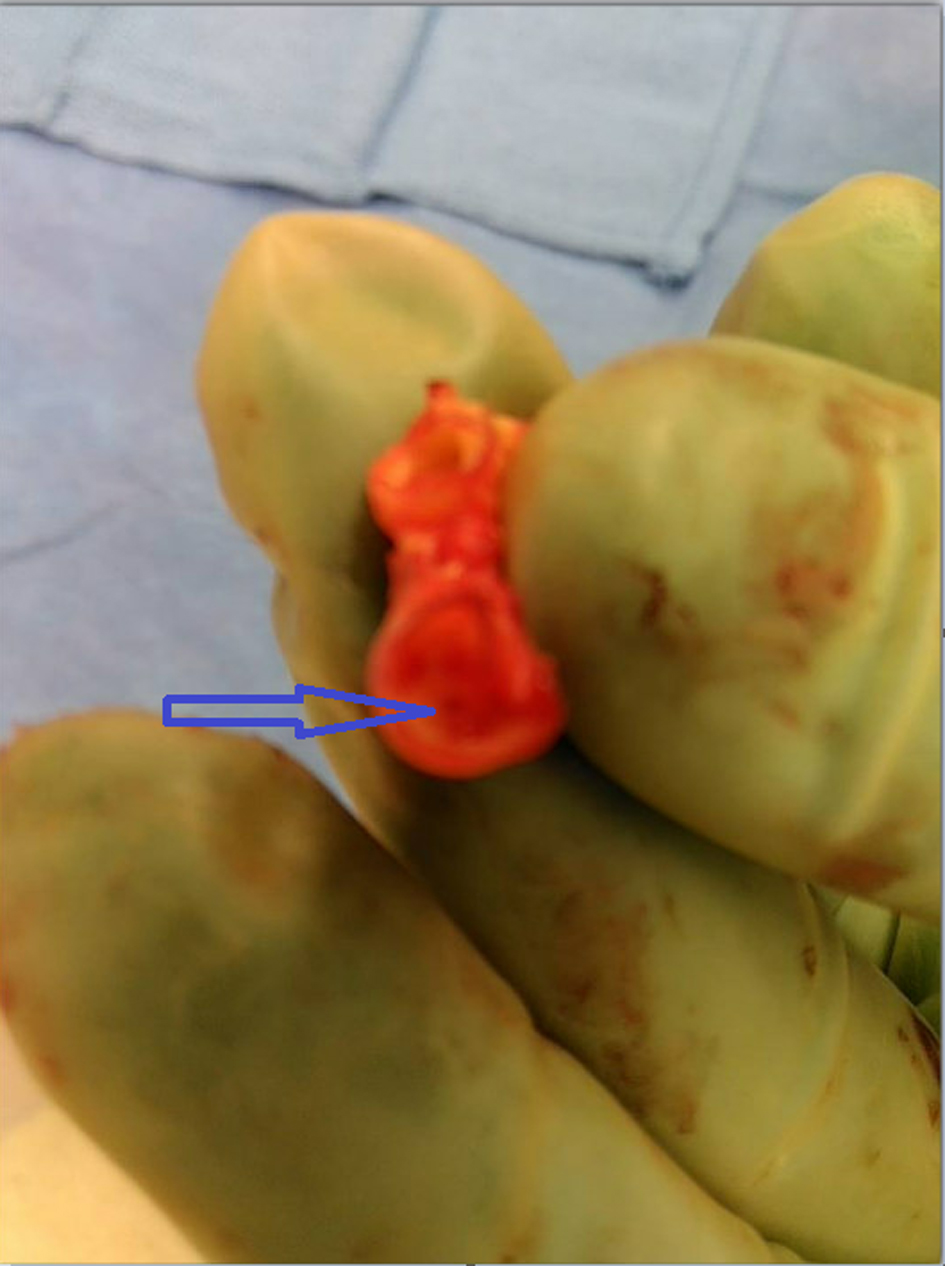 Click for large image | Figure 4. Intraoperative photo highlighting the pin-hole opening rolled up and recreating natural intraluminal morphology (arrow). |
| Discussion | ▴Top |
The carotid web is an intimal variant of FMD, a systemic non-atherosclerotic vascular disorder that most commonly affects the renal and extracranial carotid arteries [4]. Radiographically, carotid webs present as translucent, shelf-like posteroanterior projections in the proximal ICA on oblique sagittal CTA and a septal defect just beyond the carotid bifurcation on axial CTA [5]. Carotid webs have been proposed as a possible mechanism for ESUS, in which an infarct occurs in the absence of hemodynamically significant atherosclerotic stenosis or cardioembolic risk factors, due to the altered hemodynamics of the ICA. Internal carotid webs disrupt normal laminar flow through the vessel, creating zones of recirculation distal to the web that favor platelet aggregation and thrombus formation [7]. The altered hemodynamics associated with carotid webs can be directly visualized by digital subtraction angiography [8], although this was not performed for this patient.
As carotid webs promote thrombus formation through turbulent blood flow and stasis, patients who present with symptomatic carotid webs are typically younger with fewer vascular risk factors than those associated with symptomatic atherosclerotic carotid stenosis. In a 2018 systematic literature review, the median age of presentation for 134 cases of symptomatic carotid webs was 46 years old. Additionally, among 94 patients with recorded stroke risk factors, only 43% had one or more risk factors of developing carotid web disease. For patients with recorded vascular risk factors, the prevalence of smoking, hypertension, and hyperlipidemia are significantly lower in patients with symptomatic carotid web than those observed in atherosclerotic carotid stenosis. These findings are consistent with a 2019 matched case-control study, in which nine symptomatic carotid webs (17.6%) were present in young patients presenting with hemispheric ESUS, compared to 0 out of 51 matched trauma patients [9]. In a 2018 post-hoc analysis of 500 patients from the Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands (MR CLEAN) [10], 11 patients (2.5%) with carotid webs presented with ipsilateral IS compared to two patients (0.5%) with carotid webs contralateral to the occluded vessel, yielding an odds ratio (OR) of 10 (95% confidence interval (CI): 1.28 - 78.12; P = 0.28). For those with symptomatic ipsilateral carotid webs, these patients tended to be younger, female, have no smoking history, and have less cardiovascular risk factors than IS patients without carotid webs [11].
The optimal management of symptomatic carotid webs is controversial. Recurrent ischemic events are a significant source of morbidity in this population: a 2021 ad hoc analysis of the MR CLEAN trial observed that patients with symptomatic carotid webs had a 17% rate of recurrent ipsilateral IS, compared to 3% for patients without carotid webs [12]. For patients presenting after an ischemic event, management is tailored towards medical therapy or definitive treatment via endovascular stenting or CEA. Single and dual antiplatelet therapy has been observed to be less effective in secondary stroke prevention when a carotid web is present. Joux et al observed that six of 20 (30%) patients receiving antiplatelet monotherapy for secondary stroke prevention experienced another ipsilateral ischemic event [13]. A similar phenomenon was shown by Haussen et al, in which, out of seven patients with carotid webs who experienced recurrent ischemic events, two were on dual antiplatelets, three on antiplatelet monotherapy, and one had received thrombolysis within 24 h of recurrence [8]. Anticoagulation may be a preferable medical option, as it may prevent thrombus forming in the static pocket of the carotid web. However, evidence is limited in the literature, and the presence of the fibrous web without remodeling potential may require definitive treatment in most patients.
In our case, the patient deviated from the conventional presentation of carotid webs in several distinct ways. As with FMD, the presentation of symptomatic carotid webs is most common in younger female patients without vascular risk factors [6, 14]. At the age of 90, this patient is the oldest case of symptomatic carotid web recorded in the literature. Additionally, the degree of stenosis, according to North American Symptomatic Carotid Endarterectomy Trial criteria, observed on duplex ultrasound and CTA for this patient greatly exceeds what is typically observed in carotid webs without comorbid atherosclerosis or calcifications [15]. Haussen et al observed no symptomatic carotid webs with > 50% stenosis [8]. In a study by Guglielmi et al, 0 of the 30 patients with carotid webs and recurrent ipsilateral ischemic events had > 50% stenosis [12]. This trend is complicated by the exclusion of moderately or severely stenosed vessels from some studies, as atherosclerotic disease may be a more plausible etiology for embolic ischemic events in this population [11, 16]. Additionally, this could also represent a circumferential fibrous plaque producing carotid diaphragm; however, more literature describing carotid webs would be needed to provide a better definition. Despite this patient’s advanced age, smoking history, and comorbid vascular risk factors, the excised proximal ICA demonstrated no ruptured atheroma.
Learning points
This case demonstrates the safety and efficacy of performing a carotid endartectomy for nonagenarian for a symptomatic carotid web. Our patient has progression from a previously noted asymptomatic lesion to developing symptoms. Despite this patient’s advanced age and PMH, the excised proximal ICA demonstrated no ruptured atheroma and circumferential, near-occlusive fibrotic tissue. Carotid stenting for such lesions should be avoided given risks of stent compression and occlusion.
Acknowledgments
None to declare.
Financial Disclosure
The research presented in this manuscript had no specific funding from any agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare there is no conflict of interest.
Informed Consent
Informed consent was obtained for use of de-identified information for publication per our Institutional Review Board policy.
Author Contributions
Daniel L. Burke, Aldin Mlakoc, and Iden Andacheh: conceptualization, methodology, writing - original draft, writing - review and editing. All authors read and approved the final manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available in the article.
Abbreviations
ESUS: embolic stroke of unknown origin; FMD: fibromuscular dysplasia; ICA: internal carotid artery; IS: ischemic stroke
| References | ▴Top |
- Ornello R, Degan D, Tiseo C, Di Carmine C, Perciballi L, Pistoia F, Carolei A, et al. Distribution and temporal trends from 1993 to 2015 of ischemic stroke subtypes: a systematic review and meta-analysis. Stroke. 2018;49(4):814-819.
doi pubmed - Hart RG, Catanese L, Perera KS, Ntaios G, Connolly SJ. Embolic stroke of undetermined source: a systematic review and clinical update. Stroke. 2017;48(4):867-872.
doi pubmed - Hart RG, Diener HC, Coutts SB, Easton JD, Granger CB, O'Donnell MJ, Sacco RL, et al. Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol. 2014;13(4):429-438.
doi pubmed - Mac Grory B, Emmer BJ, Roosendaal SD, Zagzag D, Yaghi S, Nossek E. Carotid web: an occult mechanism of embolic stroke. J Neurol Neurosurg Psychiatry. 2020;91(12):1283-1289.
doi pubmed - Choi PM, Singh D, Trivedi A, Qazi E, George D, Wong J, Demchuk AM, et al. Carotid webs and recurrent ischemic strokes in the era of CT angiography. AJNR Am J Neuroradiol. 2015;36(11):2134-2139.
doi pubmed - Olin JW, Froehlich J, Gu X, Bacharach JM, Eagle K, Gray BH, Jaff MR, et al. The United States Registry for Fibromuscular Dysplasia: results in the first 447 patients. Circulation. 2012;125(25):3182-3190.
doi pubmed - Ozaki D, Endo T, Suzuki H, Sugiyama SI, Endo K, Itabashi R, Fujimura M, et al. Carotid web leads to new thrombus formation: computational fluid dynamic analysis coupled with histological evidence. Acta Neurochir (Wien). 2020;162(10):2583-2588.
doi pubmed - Haussen DC, Grossberg JA, Bouslama M, Pradilla G, Belagaje S, Bianchi N, Allen JW, et al. Carotid web (Intimal Fibromuscular Dysplasia) has high stroke recurrence risk and is amenable to stenting. Stroke. 2017;48(11):3134-3137.
doi pubmed - Kim SJ, Allen JW, Bouslama M, Nahab F, Frankel MR, Nogueira RG, Haussen DC. Carotid webs in cryptogenic ischemic strokes: a matched case-control study. J Stroke Cerebrovasc Dis. 2019;28(12):104402.
doi pubmed - Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11-20.
doi pubmed - Compagne KCJ, van Es A, Berkhemer OA, Borst J, Roos Y, van Oostenbrugge RJ, van Zwam WH, et al. Prevalence of carotid web in patients with acute intracranial stroke due to intracranial large vessel occlusion. Radiology. 2018;286(3):1000-1007.
doi pubmed - Guglielmi V, Compagne KCJ, Sarrami AH, Sluis WM, van den Berg LA, van der Sluijs PM, Mandell DM, et al. Assessment of recurrent stroke risk in patients with a carotid web. JAMA Neurol. 2021;78(7):826-833.
doi pubmed - Joux J, Chausson N, Jeannin S, Saint-Vil M, Mejdoubi M, Hennequin JL, Deschamps L, et al. Carotid-bulb atypical fibromuscular dysplasia in young Afro-Caribbean patients with stroke. Stroke. 2014;45(12):3711-3713.
doi pubmed - Sharashidze V, Nogueira RG, Al-Bayati AR, Bhatt N, Nahab FB, Yun J, Allen JW, et al. Carotid web phenotype is uncommonly associated with classic fibromuscular dysplasia: a retrospective observational study. Stroke. 2022;53(2):e33-e36.
doi pubmed - Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, Rankin RN, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1998;339(20):1415-1425.
doi pubmed - Ospel JM, Singh N, Marko M, Almekhlafi M, Dowlatshahi D, Puig J, Demchuk A, et al. Prevalence of ipsilateral nonstenotic carotid plaques on computed tomography angiography in embolic stroke of undetermined source. Stroke. 2020;51(6):1743-1749.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.