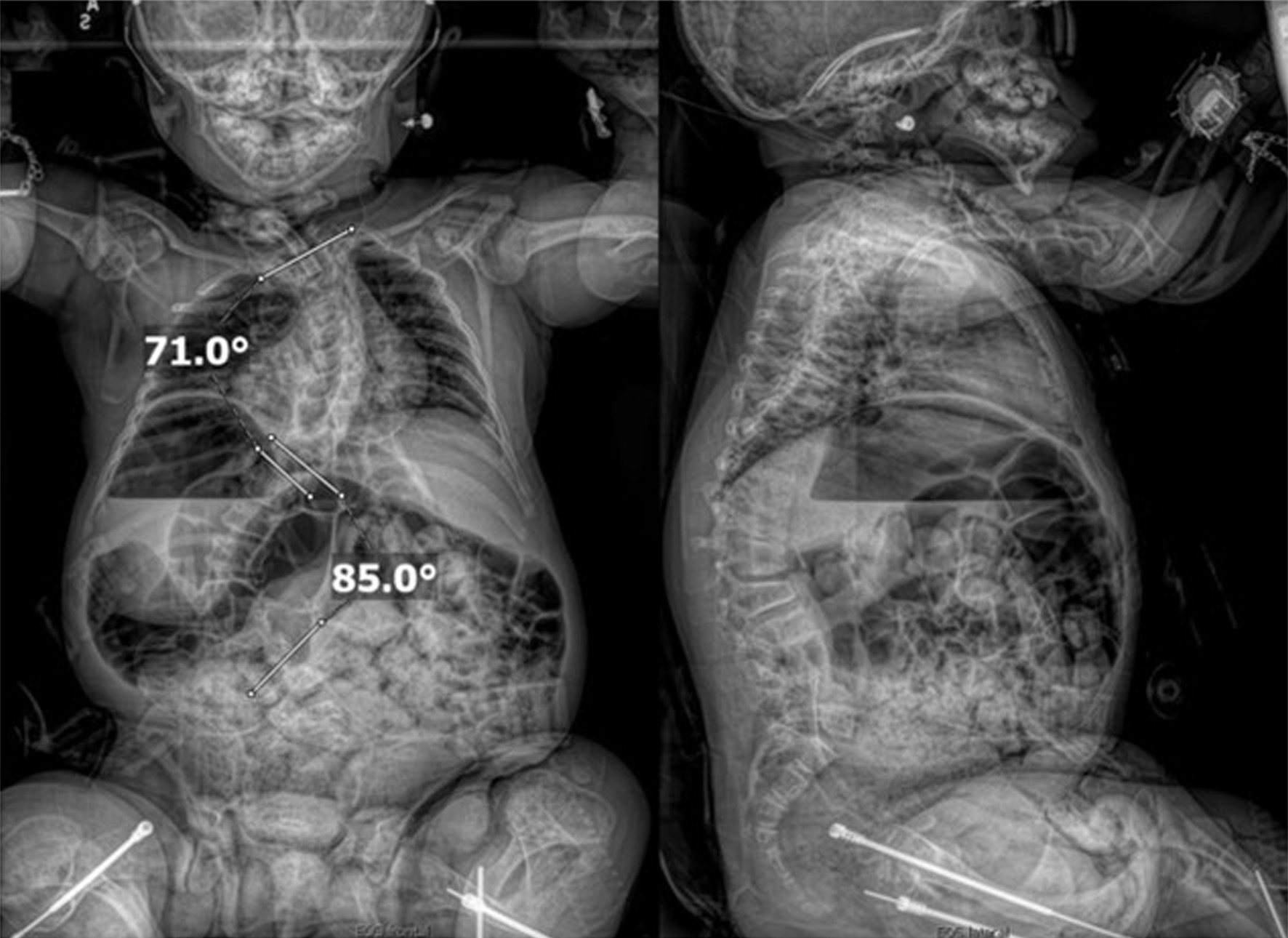
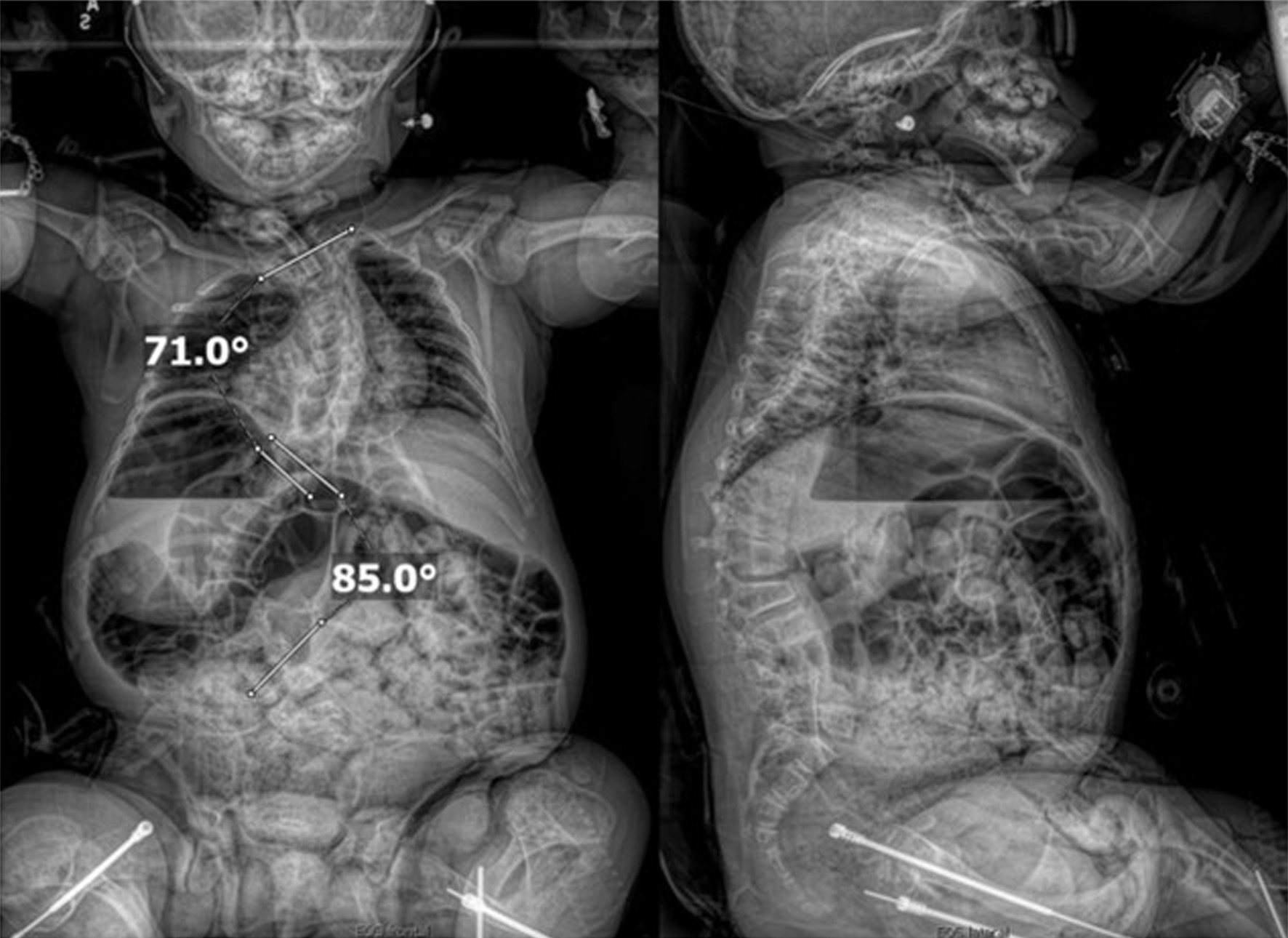
Figure 1. Preoperative seated radiographs demonstrating severe scoliosis with 71° right thoracic curve (T1-T9), 85° left lumbar curve (T9-L3, major), and thoracolumbar kyphosis.
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 17, Number 3, March 2026, pages 107-114
Perioperative Care of an Eleven-Year-Old Child With Osteogenesis Imperfecta Type II During Posterior Spinal Fusion
Figures


Tables
| Author and reference | Patient demographic | Anesthetic technique | Comments and outcome |
|---|---|---|---|
| BP: blood pressure; OI: osteogenesis imperfecta; PSF: posterior spinal fusion. | |||
| Patino and Soliman [26] | A 4-year-old, 11 kg girl with OI and severe scoliosis (Cobb angle 90°) for PSF (T2–L3). Prior history of multiple atraumatic fractures and restrictive lung disease. | Induction and maintenance: Intravenous induction with propofol, oxygen/nitrous oxide, isoflurane, and remifentanil (0.1–0.3 µg/kg/min). Airway approach: Gentle mask ventilation and direct laryngoscopy with neutral head positioning. | Attention to prone positioning with pressure points padded. Invasive BP monitoring and avoidance of noninvasive blood pressure monitoring due to fracture risk. Cell saver to limit need for allogeneic blood. Patient’s trachea was extubated uneventfully, transferred to the PICU with no new fractures or complications. Uncomplicated postoperative course. |
| Chin and Stuart [27] | An 11-year-old, 21.6 kg boy with autosomal recessive OI type VIII (LEPRE1 mutation) for posterior spinal fusion (T3–L5) for progressive scoliosis (Cobb angle 54.5°). Prior history of extreme bone fragility, barrel chest, visual/hearing impairment, and restricted growth. | Induction and maintenance: Total intravenous anesthesia (TIVA) using target-controlled propofol and remifentanil. Airway approach: Endotracheal intubation by direct laryngoscopy with minimal neck movement and head in neutral position. | Invasive BP monitoring. Blood conservation strategies included intraoperative cell salvage and tranexamic acid. Temperature management included forced air warming and in-line fluid warmer. The patient’s trachea was extubated on postoperative day 1 but later sustained humeral and rib fractures (conservative management). |
| IV: intravenous; NOBP: non-invasive blood pressure; OI: osteogenesis imperfecta. |
1. Airway concerns
|
2. Progressive kyphoscoliosis and thoracic wall deformities
|
3. Cardiac involvement
|
4. Bleeding tending
|
5. Bone fragility
|
6. Difficult venous and arterial access
|
7. Positioning concerns
|
8. Potential for intraoperative hyperthermia
|
9. Central nervous system involvement
|