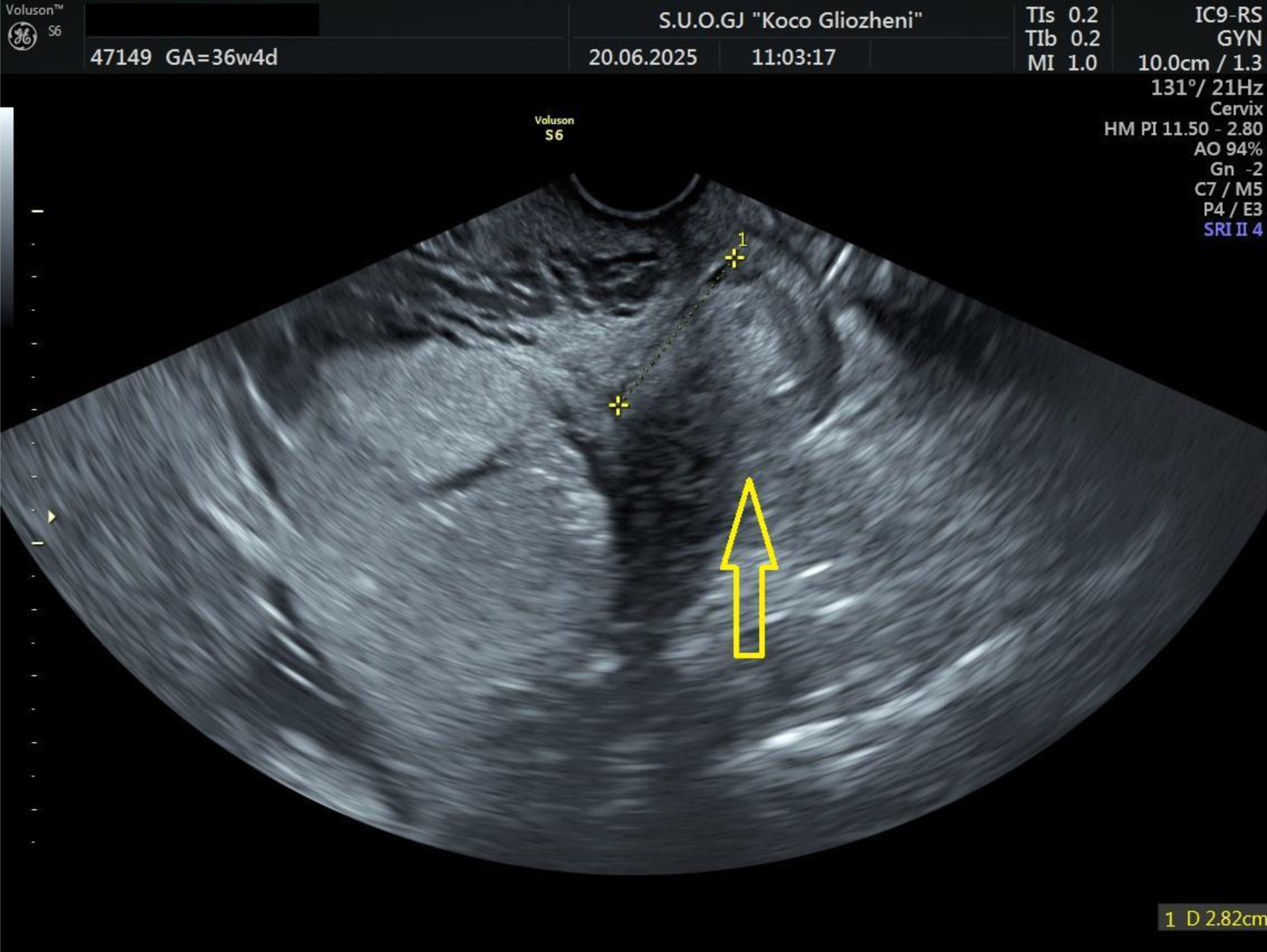
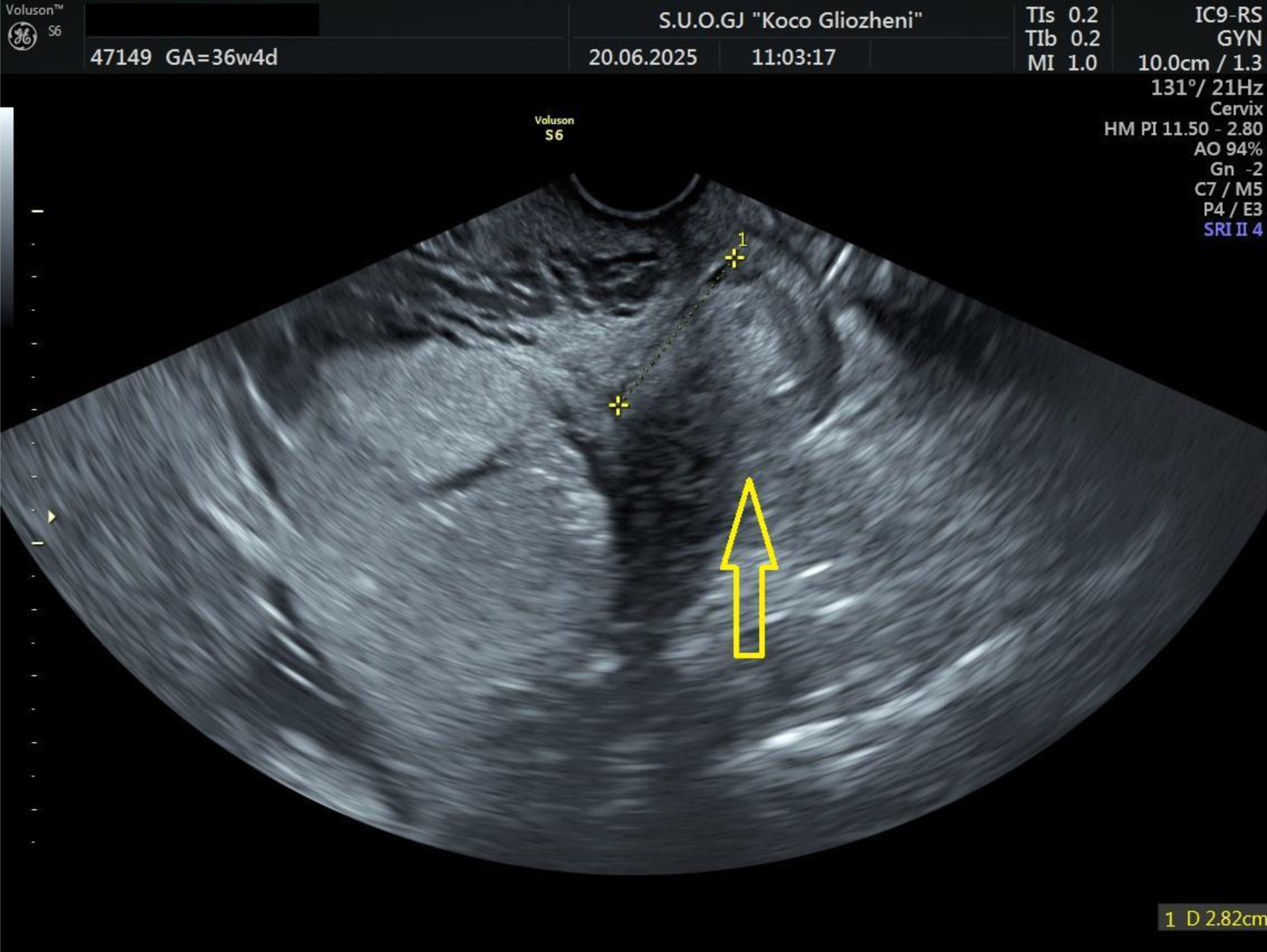
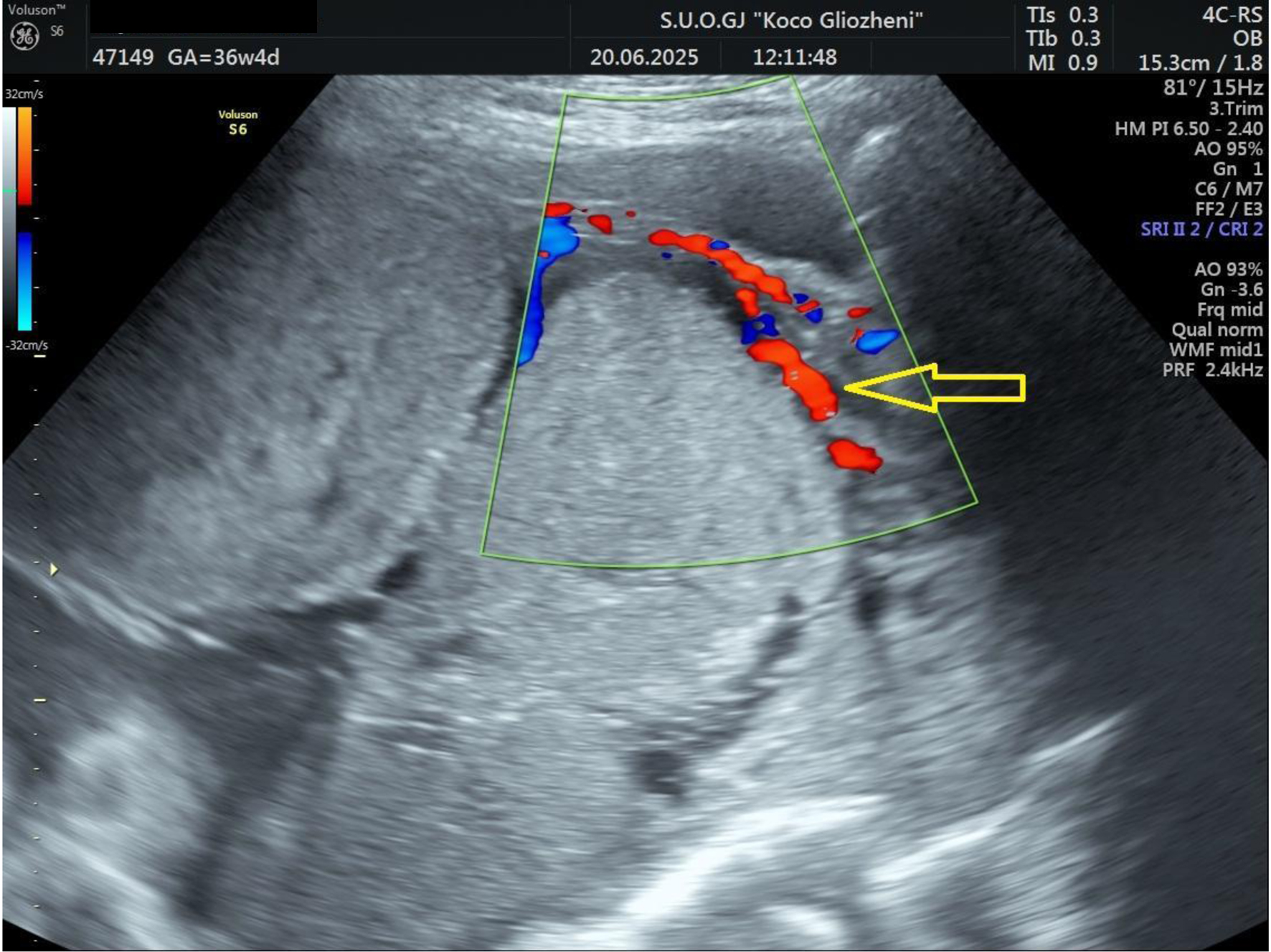
Figure 1. Ultrasound examination showing placental tissue invading the lower myometrium (arrow).
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 17, Number 1, January 2026, pages 21-27
Anesthetic and Transfusion Management in Placenta Accreta Spectrum: Lessons From a Resource-Limited Setting and Mini-Review
Figures

Tables
| Category | Complications |
|---|---|
| DIC: disseminated intravascular coagulation; DVT: deep venous thrombosis; ICU: intensive care unit; NICU: neonatal intensive care unit; PAS: placenta accreta spectrum; PE: pulmonary embolism. | |
| Hemorrhagic | Massive obstetric hemorrhage; transfusion requirement; DIC; hypovolemic shock |
| Surgical | Urologic injury (bladder, ureter); gastrointestinal injury; vascular injury; nerve injury |
| Postoperative | Infection (wound, pelvic abscess, sepsis); venous thromboembolism (DVT/PE); wound dehiscence |
| Reproductive/long-term | Loss of fertility (hysterectomy); intra-abdominal adhesions; chronic pelvic pain |
| Maternal outcome | Increased morbidity: prolonged ICU stay; increased mortality risk |
| Neonatal outcome | Preterm birth; low birth weight; NICU admission; neonatal mortality |
| Step | Intervention | Description |
|---|---|---|
| GA: general anesthesia; ICU: intensive care unit; IV: intravenous; RBC: red blood cell; FFP: fresh frozen plasma. | ||
| 1 | Monitoring and access | Establish large-bore IV access (two lines), arterial line, and central venous access if needed. Continuous hemodynamic and urine output monitoring. |
| 2 | Airway and oxygenation | Early airway control with intubation if patient unstable or anticipated rapid deterioration. Provide 100% oxygen. |
| 3 | Volume resuscitation | Start with balanced crystalloids, transition quickly to blood products. Apply massive transfusion protocol (1:1:1 ratio of RBC/FFP/platelets). |
| 4 | Hemostatic agents | Administer tranexamic acid early (within 3 h), consider fibrinogen concentrate or cryoprecipitate if hypofibrinogenemia present. |
| 5 | Anesthetic technique | GA in unstable patients; regional may be used in selected stable cases (but be prepared to convert to GA). |
| 6 | Adjunctive measures | Maintain normothermia, correct acidosis, optimize calcium levels during transfusion, permissive hypotension |
| 7 | Team communication | Close coordination with obstetricians, blood bank, and ICU team. Activate massive transfusion protocol early. |
| 8 | Postoperative care | Transfer to ICU for ongoing resuscitation, monitoring, and correction of coagulopathy. |
| Intervention | Description |
|---|---|
| FFP: fresh frozen plasma. | |
| Uterotonics and uterine massage | First-line measures to stimulate uterine contraction and reduce bleeding. |
| Tranexamic acid | Early administration (within 3 h) to reduce fibrinolysis and improve survival. |
| Volume replacement | Use crystalloids and initiate massive transfusion protocols (1:1:1 ratio). |
| Surgical interventions | Balloon tamponade, compression sutures, arterial ligation, or hysterectomy if conservative methods fail. |
| Correction of coagulopathy | Administer FFP, platelets, cryoprecipitate, or fibrinogen concentrate as indicated. |
| Hemodynamic | Permissive hypotension |
| Multidisciplinary approach | Close coordination between obstetric, anesthetic, surgical, and blood bank teams. |