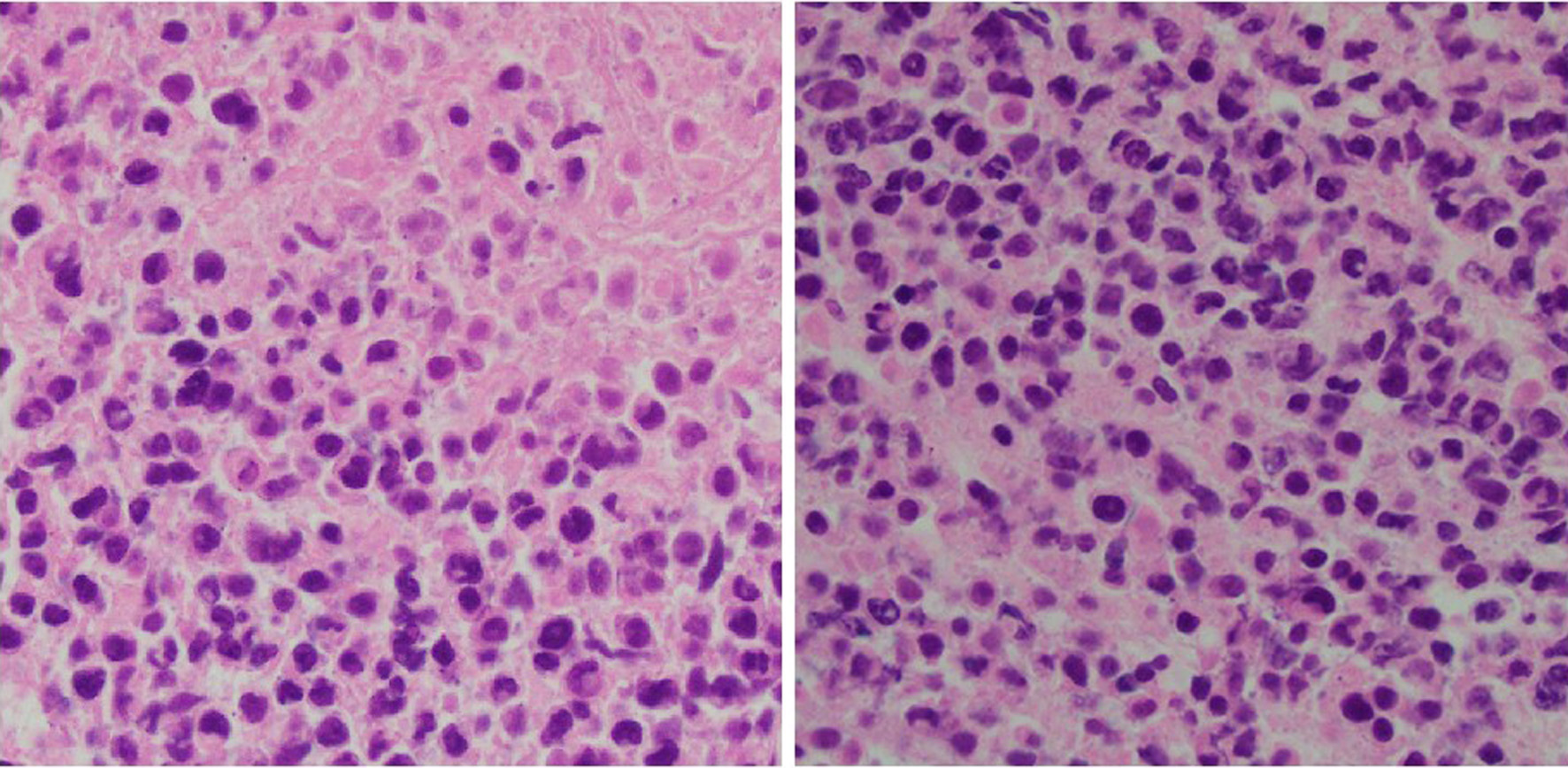
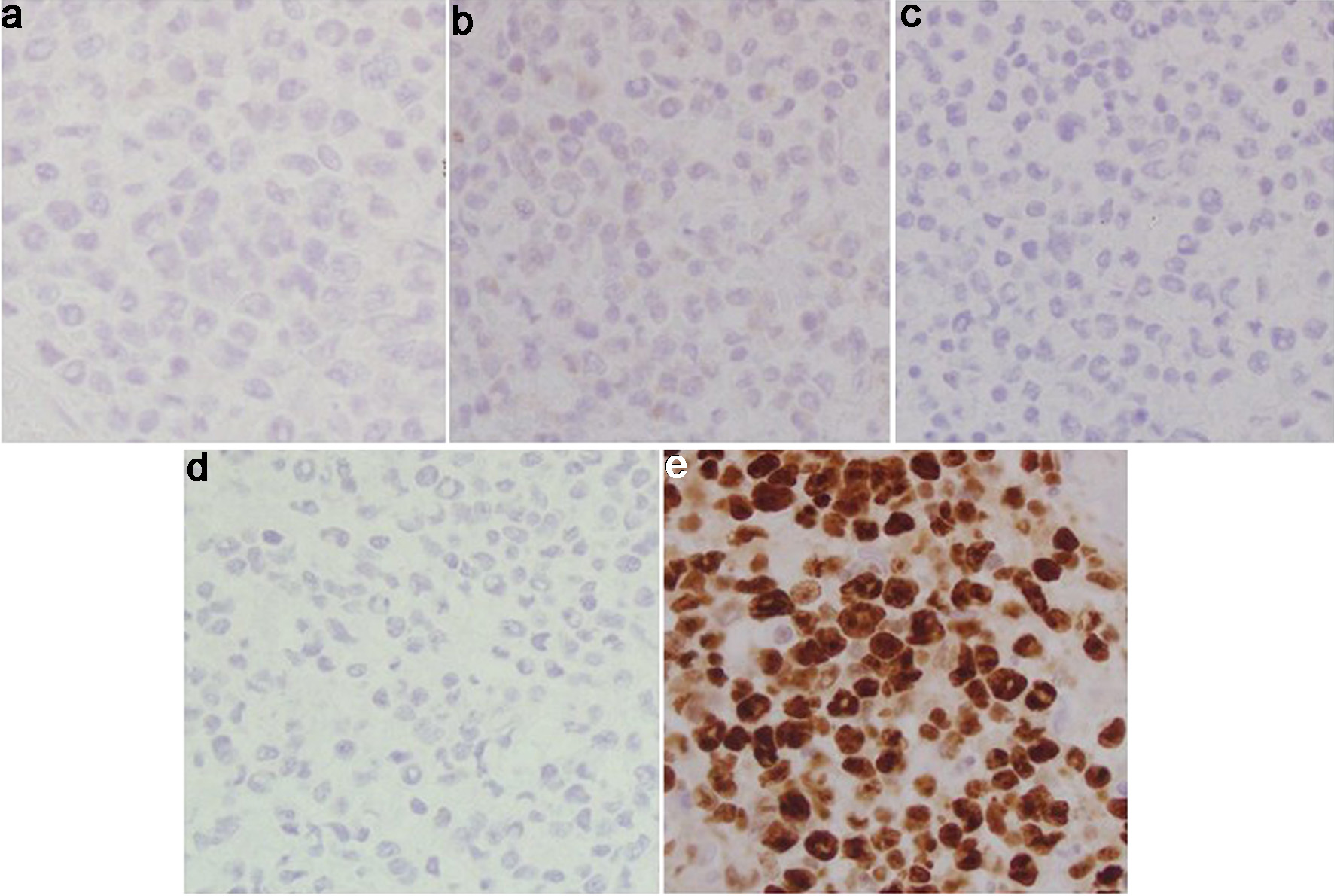
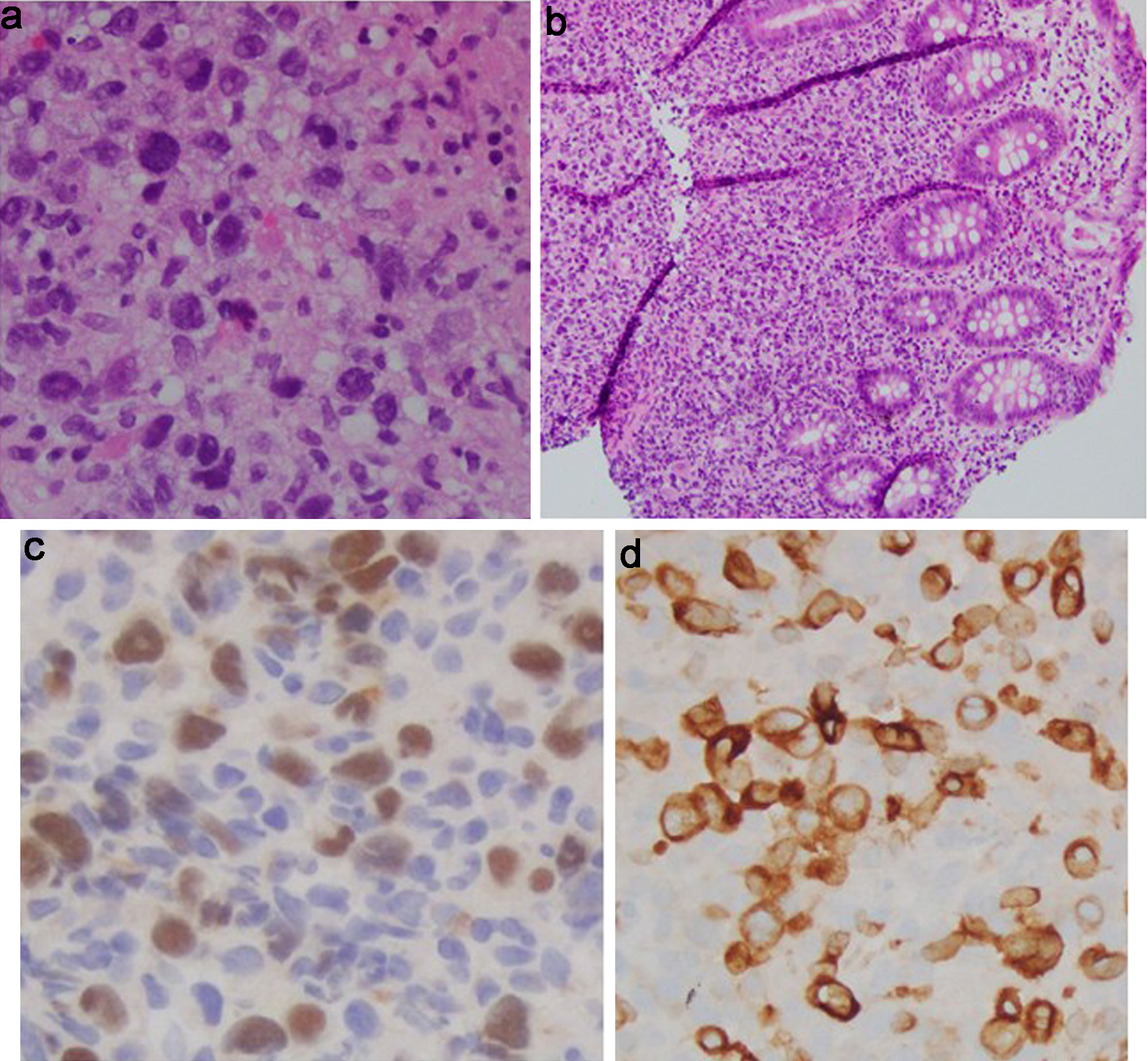
Figure 1. Tonsil mass biopsy histology: high-grade lymphoid neoplasm with necrosis (H&E, × 40). H&E: hematoxylin and eosin.
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 12, December 2025, pages 475-486
Cecal Involvement of Diffuse Large B-Cell Lymphoma: A Rare Extra-Nodal Presentation
Figures
Table
| Timeline/date | Clinical event/presentation | Diagnostic tests and findings | Treatment/intervention | Outcome/notes |
|---|---|---|---|---|
| CT: computed tomography; DLBCL: diffuse large B-cell lymphoma; EBER-ISH: Epstein-Barr virus-encoded small RNA in situ hybridization; EBV-LMP1: Epstein-Barr virus latent membrane protein 1; FDG: F-fluorodeoxyglucose; GCB: germinal center B-cell; PET: positron emission tomography; R-CHOP: rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone; R-ICE: rituximab, ifosfamide, carboplatin, and etoposide; SUV: standardized uptake value. | ||||
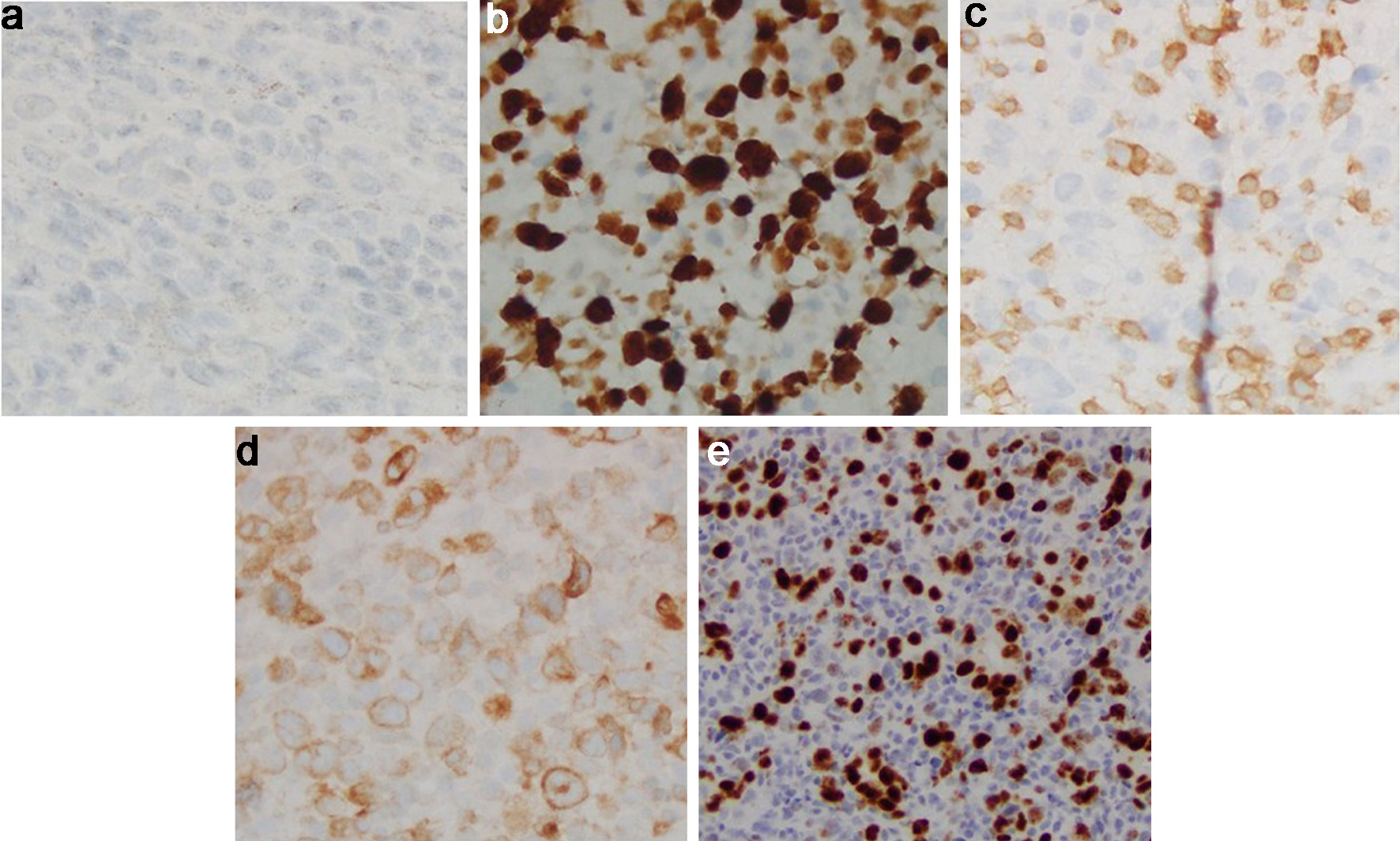
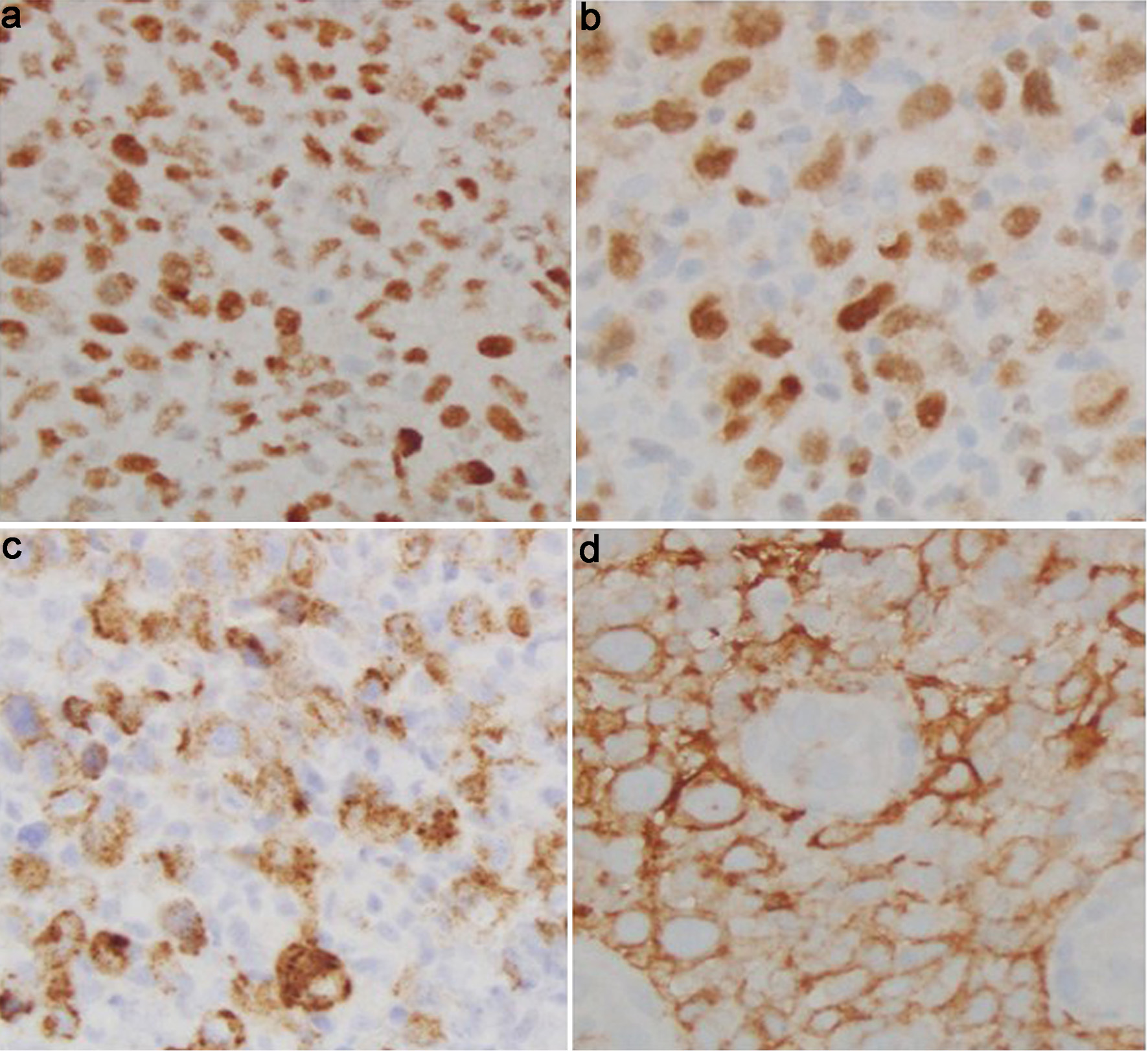
| Initial presentation | 56-year-old male with 6-week history of sore throat, enlarging neck mass, odynophagia, dysphagia, 10-lb weight loss, night sweats | CT neck: enlarged thyroid with bilateral lesions (5.5 × 4.9 cm R, 3 × 1.8 cm L), cervical lymphadenopathy, mediastinal nodes | Biopsy of left tonsillar mass | Histopathology: atypical lymphoid infiltrate; CD20+, high Ki-67 (80-90%), EBER-ISH positive; diagnosed aggressive DLBCL |
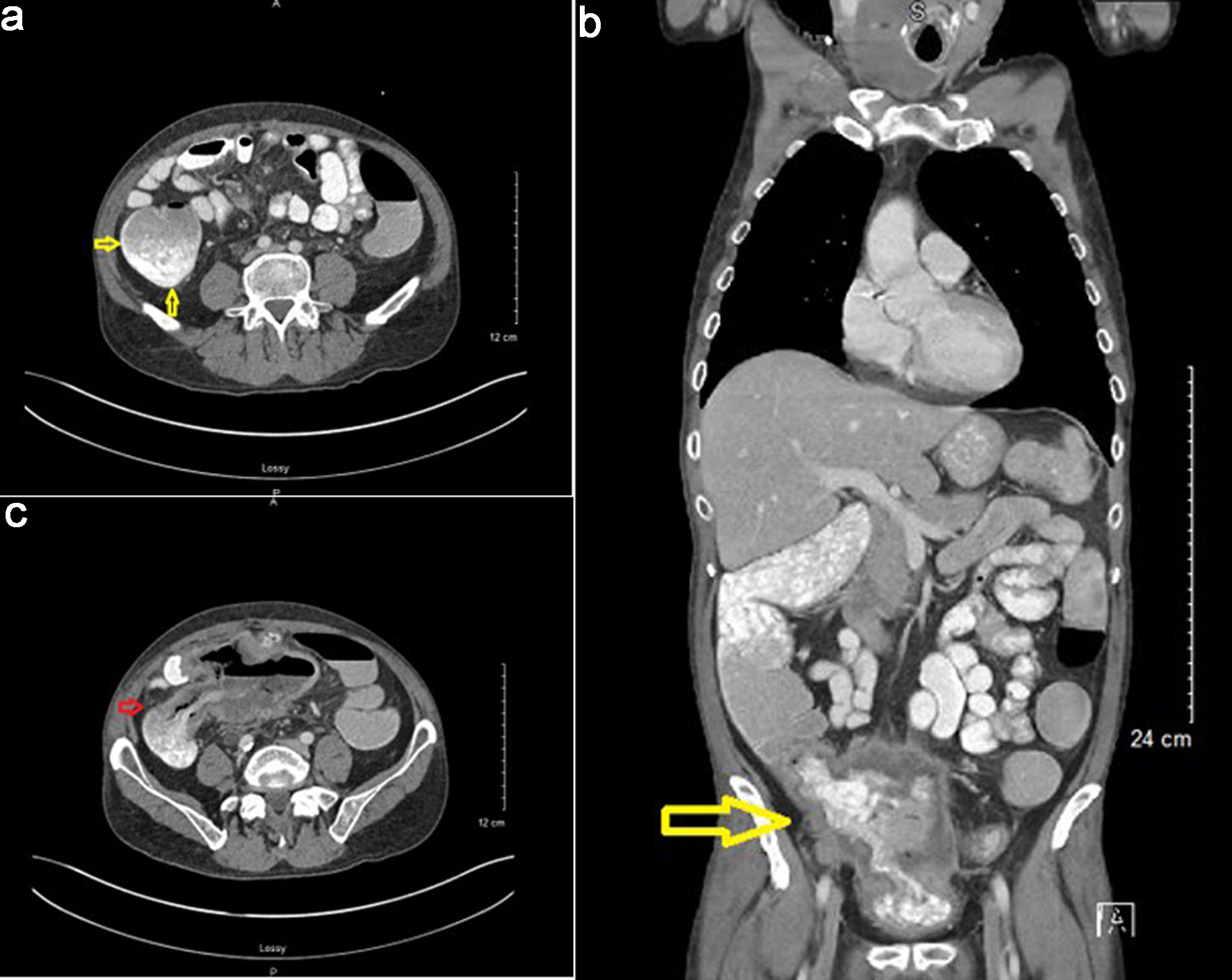
| Initial staging | PET-CT whole body | FDG-avid cervical nodes, hypermetabolic cecal wall thickening | Bone marrow biopsy | No marrow involvement |
| Initial treatment | R-CHOP chemotherapy (six cycles over 3 months) | - | R-CHOP regimen | - |
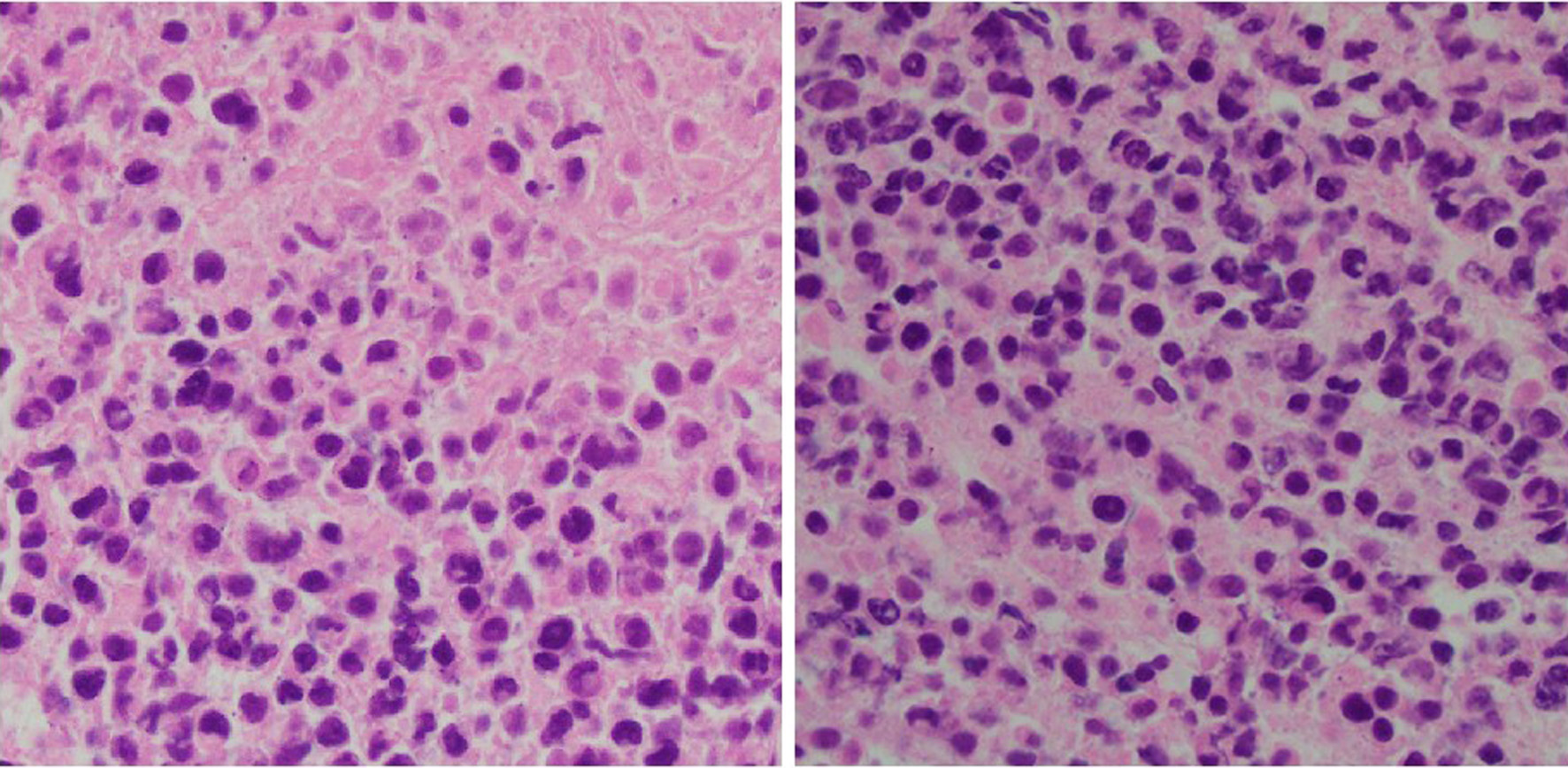
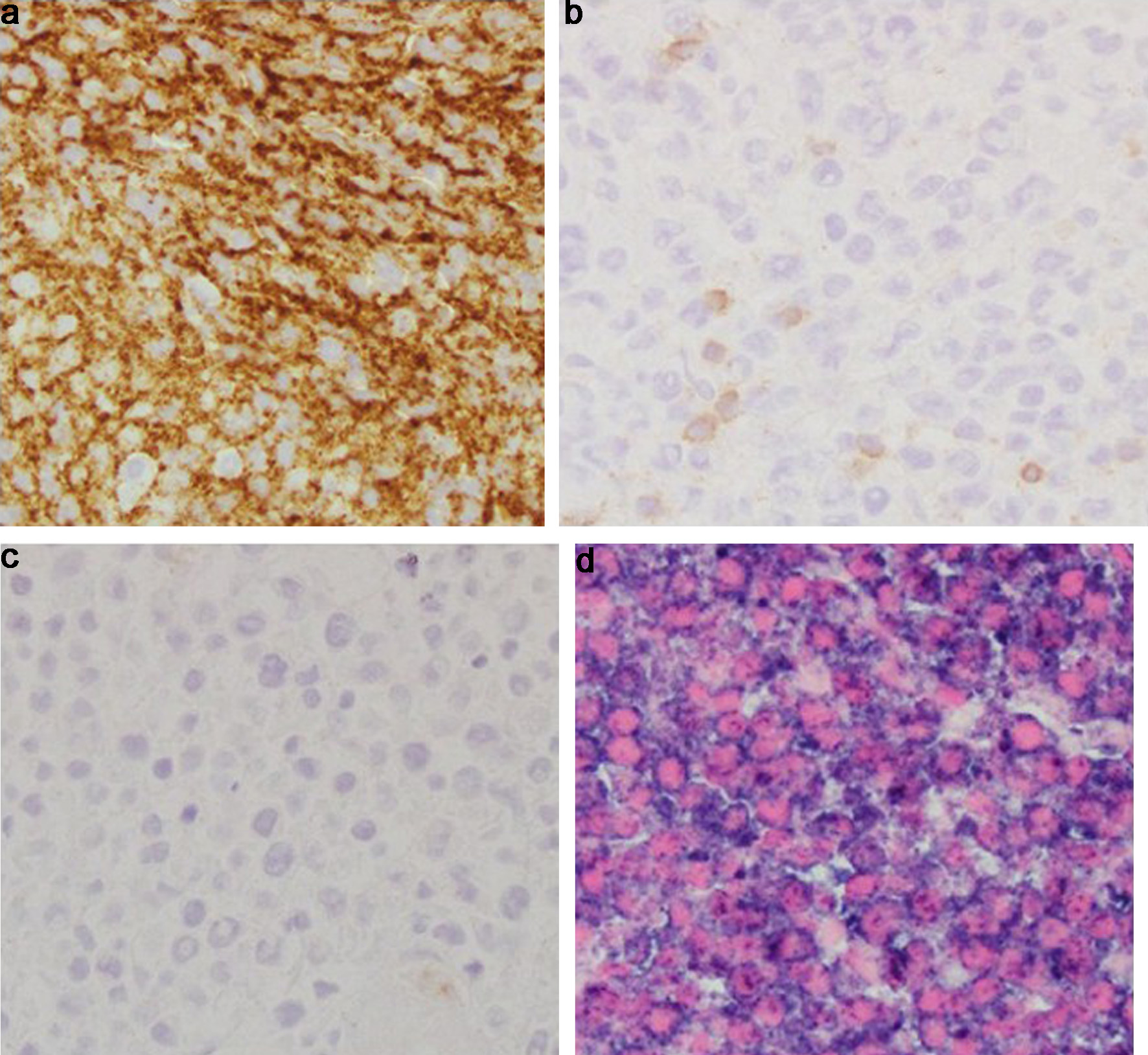
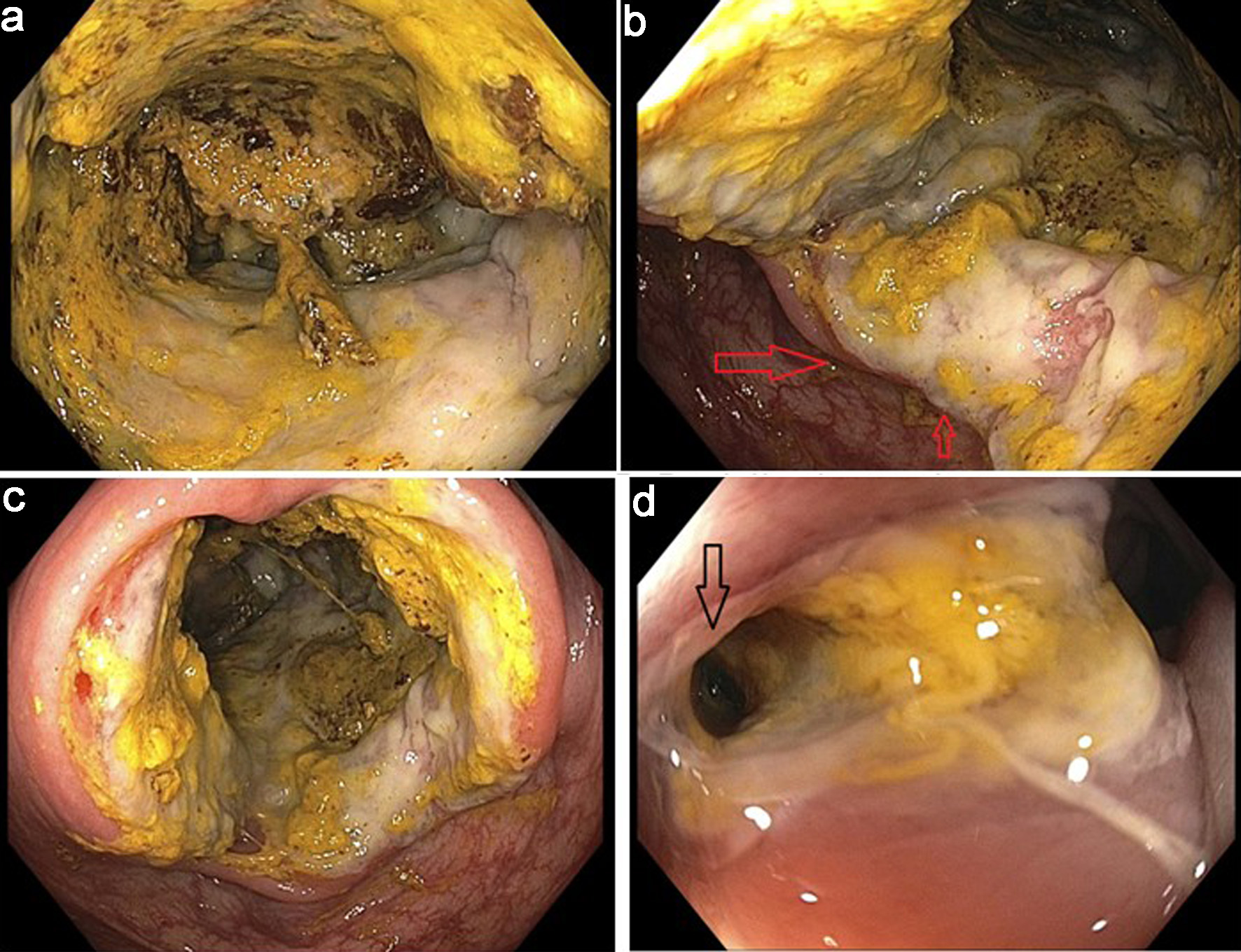
| Post-R-CHOP evaluation | PET-CT | Complete response in head/neck lymphadenopathy; persistent FDG uptake in cecum (SUV 23.2) | Gastroenterology consult; colonoscopy | 15-mm cecal ulcer biopsied; confirmed DLBCL, CD20-, PAX5+/CD79a+, Ki-67 high, EBV-LMP1+, double-expressor phenotype, GCB subtype |
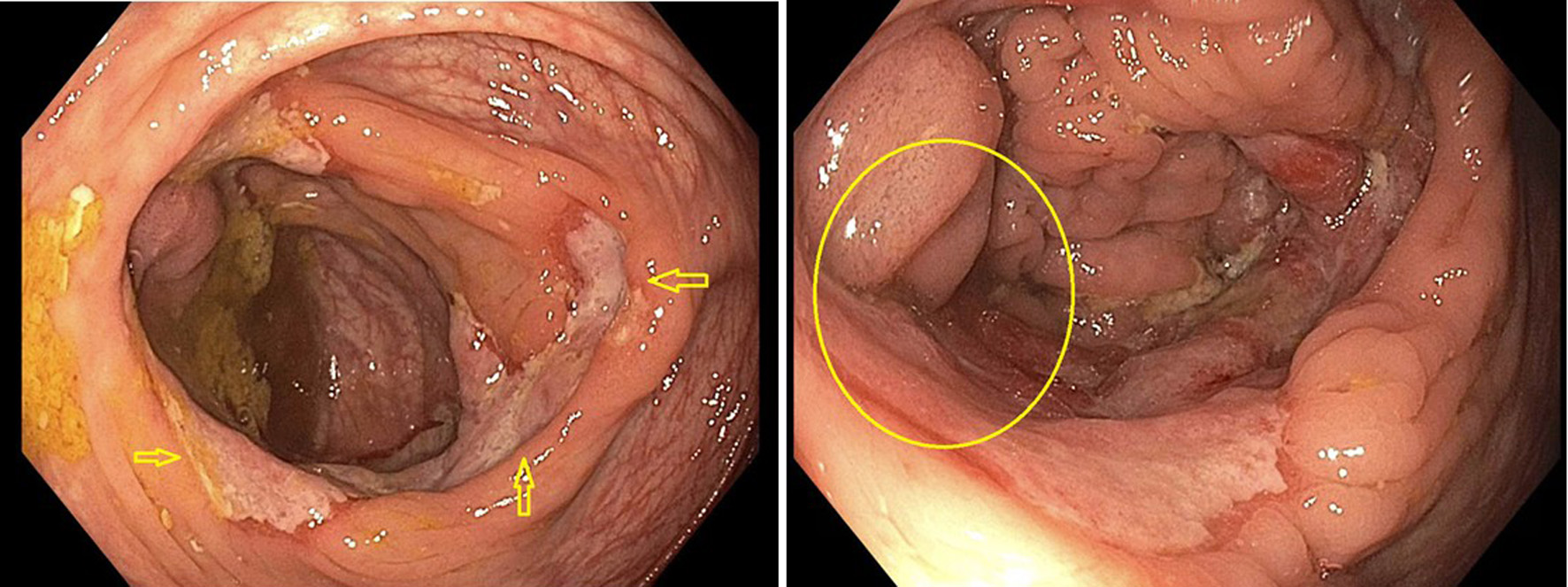
| Disease progression and development of urologic complications | Follow-up PET-CT | Metabolically active diffuse cecal wall thickening; necrotic right neck lymphadenopathy; right hydroureteronephrosis; confirmation of colovesical fistula on CT | Repeat colonoscopy | Infiltrative, ulcerated obstructing cecal mass (14 mm); rectal fistula Confirmed recurrent DLBCL; nephrostomy tube placement for obstructive uropathy |
| Salvage therapy | R-ICE chemotherapy (two cycles) | - | Rituximab, ifosfamide, carboplatin, etoposide | Did not respond; diverting loop ileostomy performed |
| Subsequent treatment | Rituximab + polatuzumab (every 21 days) | - | Chemotherapy | Disease continued to progress |
| Outcome | Final | - | Supportive care | Patient died due to lymphoma-related complications |