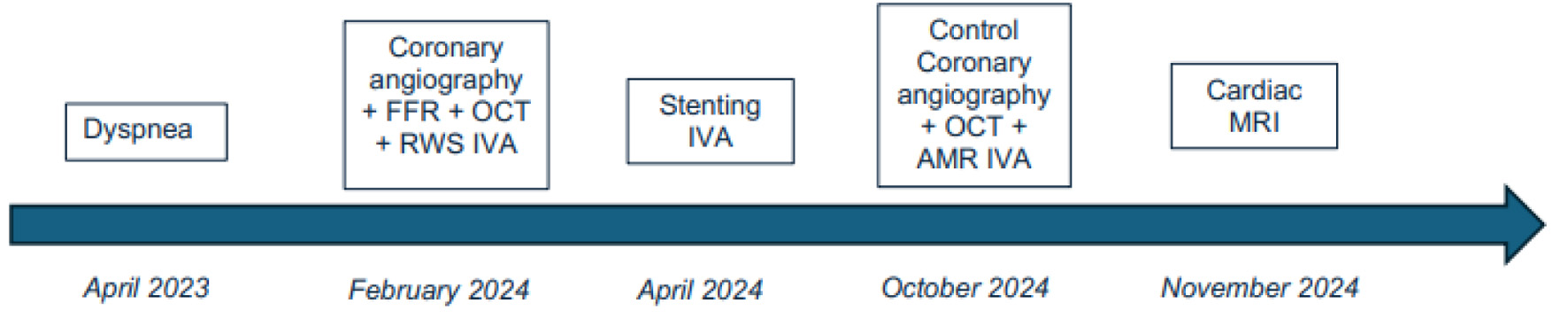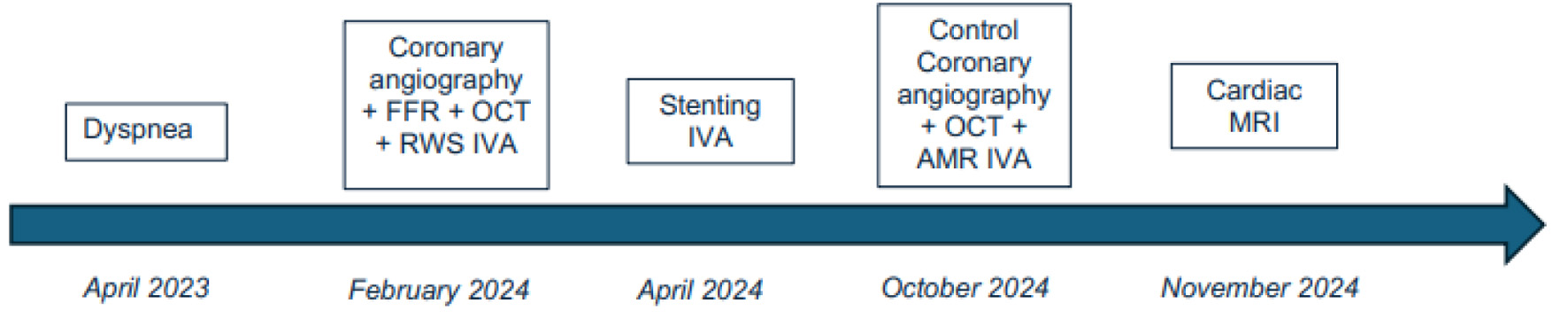
Figure 1. Timeline figure summarizing symptoms, diagnostics, interventions, and follow-up.
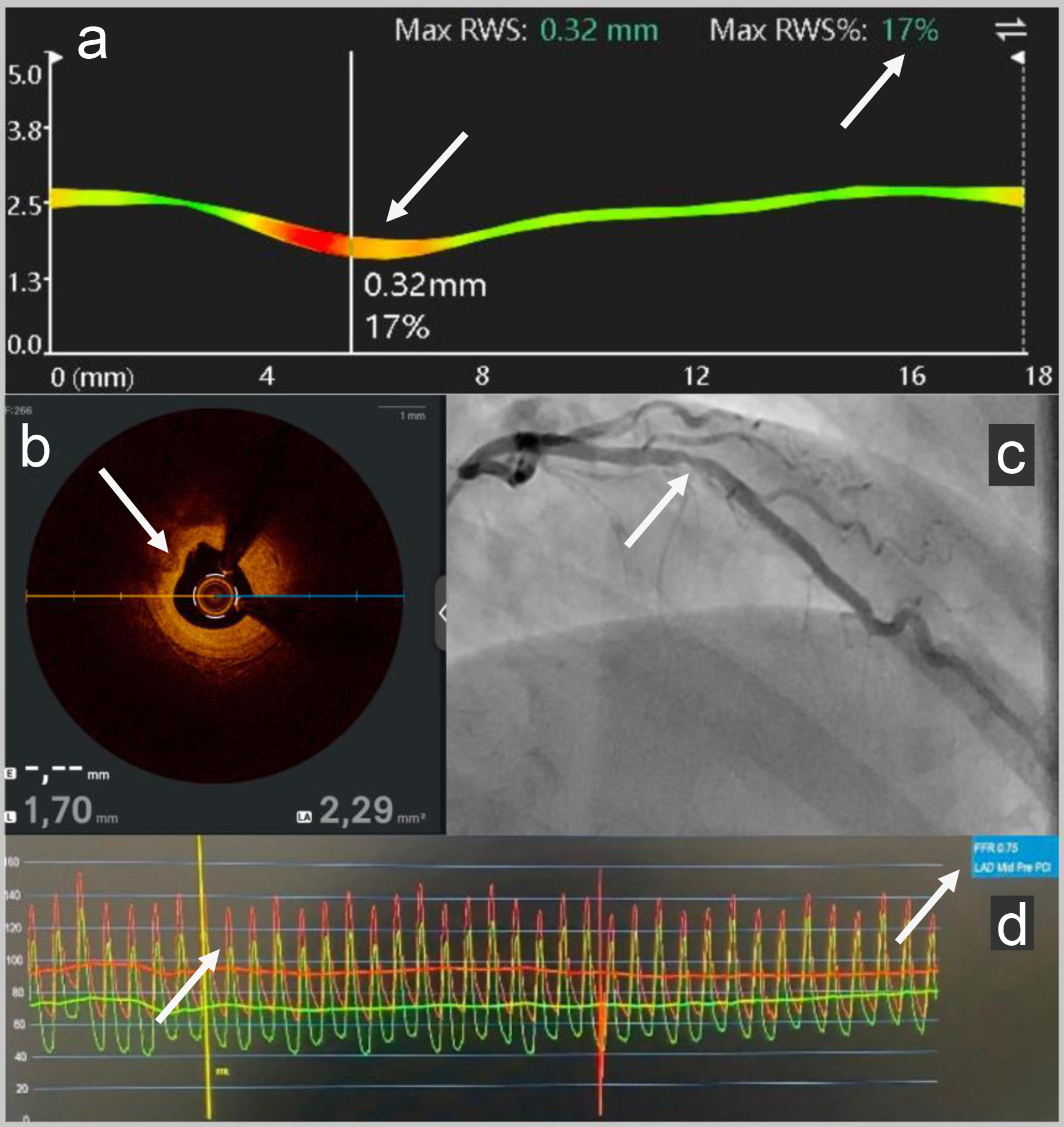
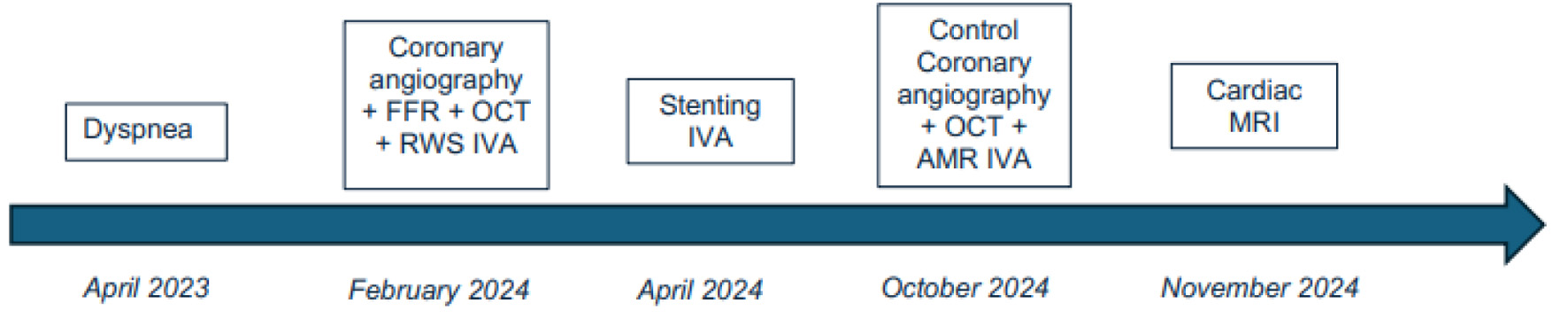
Figure 2. (a) RWS pre-PCI: Subsequent analysis using RWS (Pulse Medical) software determined the vulnerability of the mid-LAD stenosis with a high risk of myocardial infarction with pathological max RWS = 17%. (b) OCT pre-PCI: Intravascular coronary imaging: OCT (Abbott) showed a fibro-lipid plaque (the intimal layer primarily appears bright and relatively homogeneous; it causes hardly any shadowing because of the fibrous tissue) in the mid-LAD with MLA to 2.3 mm2 (standard > 4 mm2). (c) Angiography pre-PCI: Coronary angiography revealed a mid-LAD coronary artery stenosis. (d) FFR pre-PCI: The LAD FFR (Boston Scientific) was positive to 0.75 (standard > 0.80). RWS: radial wall strain; PCI: percutaneous coronary intervention; LAD: left anterior descending; OCT: optical coherence tomography; MLA: minimum lumen area; FFR: fractional flow reserve.
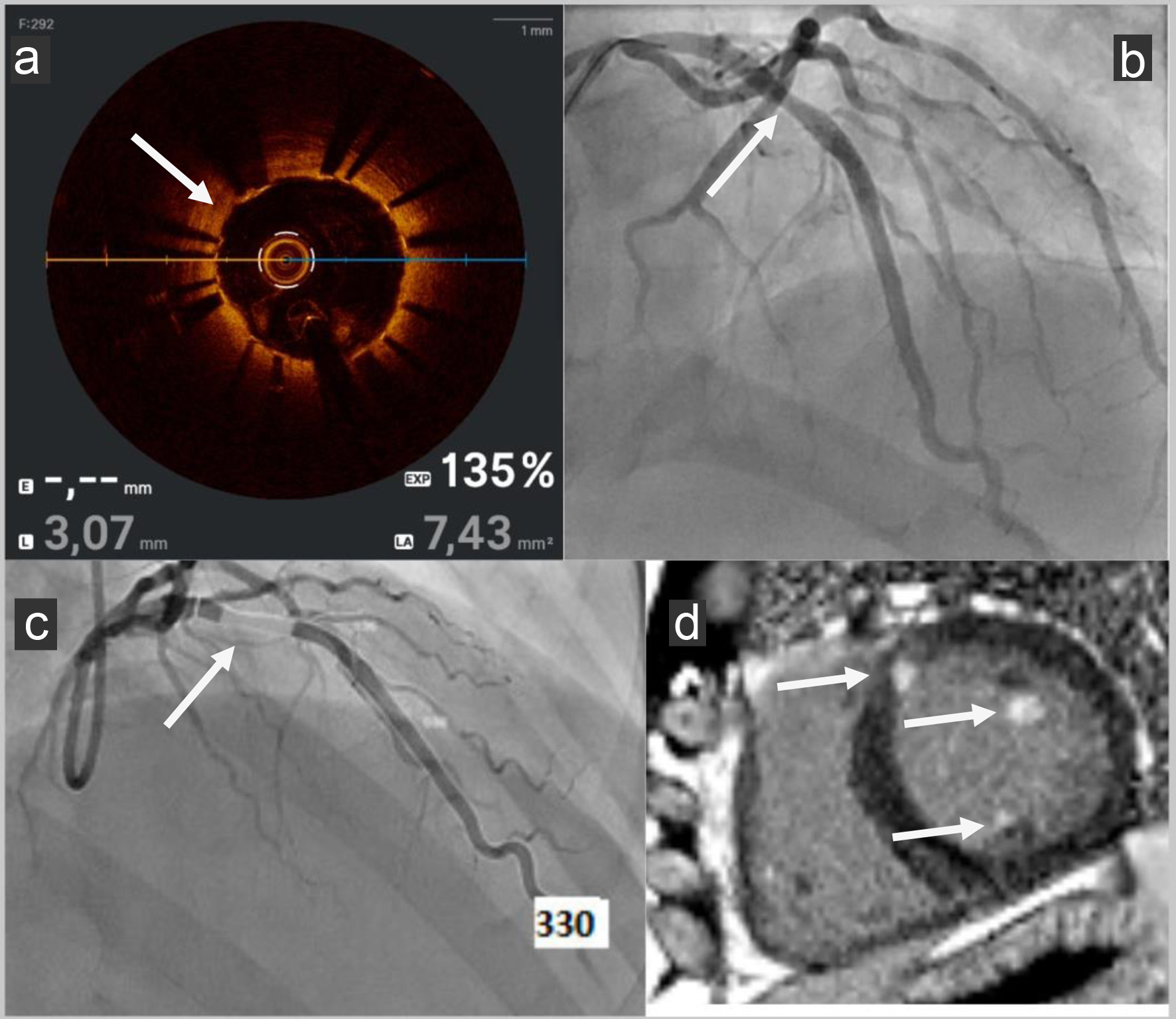
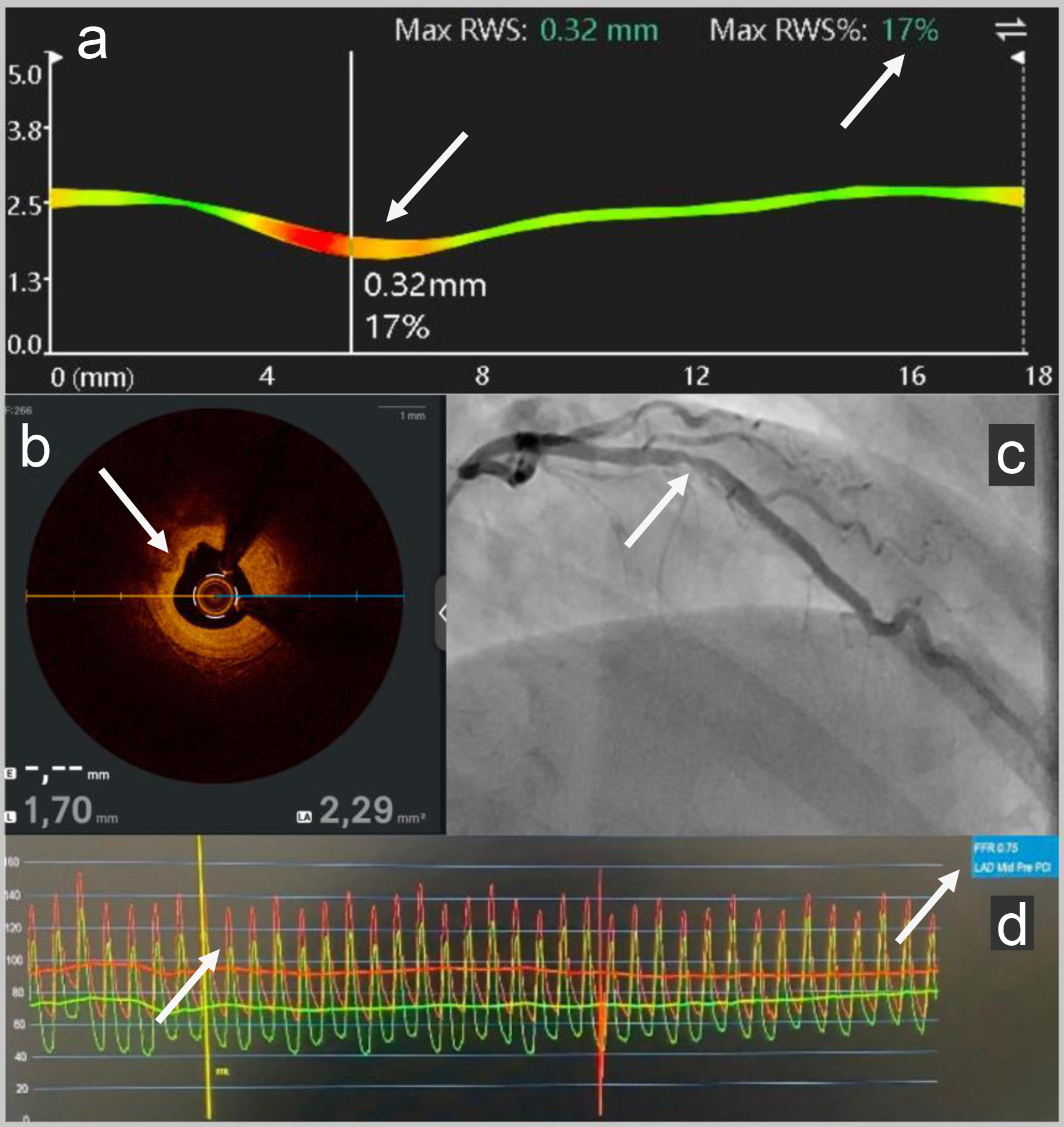
Figure 3. (a) OCT post-PCI: OCT (Abbott) showed good stent apposition (no space greater: malapposition than 0.4 mm2 between the stent struts and the intimal wall of the artery) with no ISR with MLA to 7.4 mm2 (standard > 4 mm2). (b) Angiography post-PCI: LAD PCI was performed with a bioresorbable drug-eluting stent Freesolve (Biotronik). (c) AMR post-PCI: AMR (Pulse Medical) was calculated from one coronary angiography view, yielding a pathological value of 330 mm Hg s/m (standard < 250 mm Hg s/m). (d) Cardiac MRI post-PCI: Late enhancement sequences in cardiac MRI were pathological with presence of basal and antero-septal focal intra- and sub-endocardial enhancement, involvement of two mitral pillars and a right intra ventricular mitral cord. OCT: optical coherence tomography; PCI: percutaneous coronary intervention; ISR: in-stent restenosis; MLA: minimum lumen area; LAD: left anterior descending; AMR: angiography-derived microcirculatory resistance; MRI: magnetic resonance imaging.