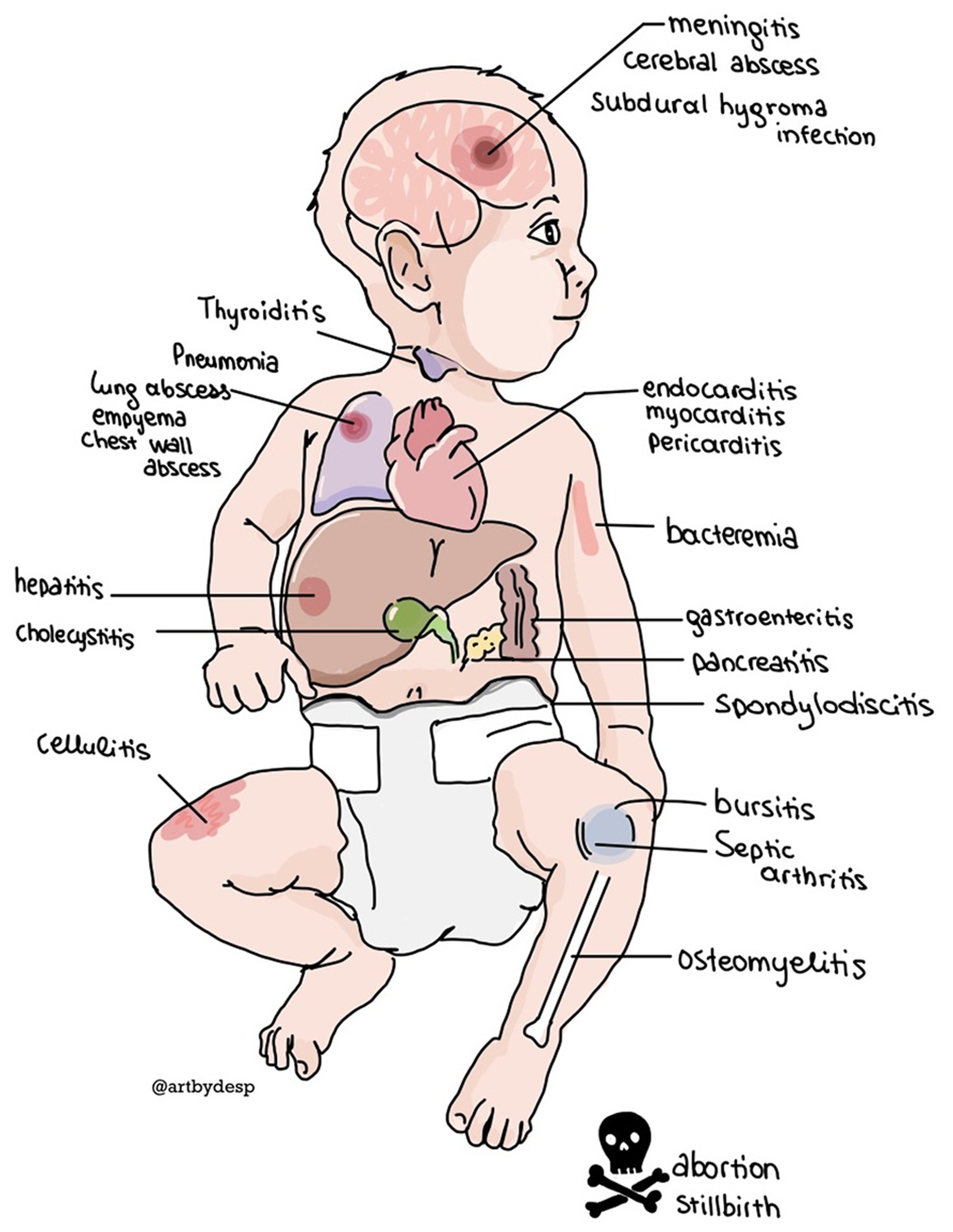
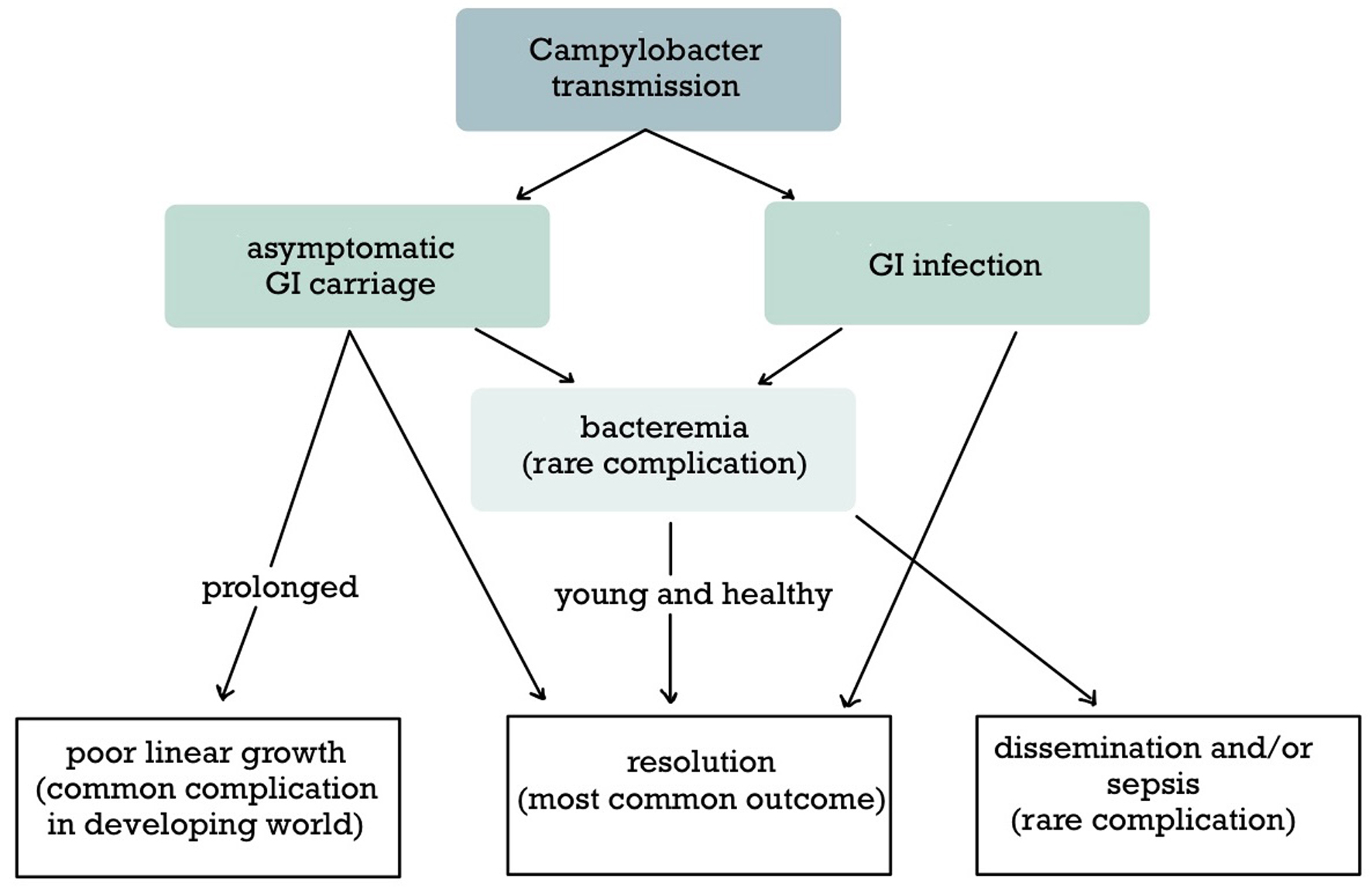
Figure 1. The extraintestinal locations of disseminated Campylobacter infection.
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 6, June 2025, pages 201-211
An Unusual Cause of Neonatal Infection: A Case Report of Campylobacter coli Meningitis and Sepsis
Figures
Tables
| PID: pelvic inflammatory disease. |
| Bacteremia |
| Nervous system: meningitis, subdural hygroma infection, cerebral abscess, neuritis |
| Cardiovascular: endovascular infections (septic thrombophlebitis, mycotic aneurysm, stent infection), endocarditis, myocarditis, pericarditis |
| Thyroiditis |
| Respiratory: pneumonia, lung abscess, empyema, chest wall abscess |
| Abdomen: hepatitis, cholecystitis, pancreatitis, peritonitis (spontaneous or secondary) |
| Skin/musculoskeletal: cellulitis, bursitis, septic arthritis, osteomyelitis, spondylodiscitis |
| Obstetrics/gynecology: cervicitis, PID, abortion, stillbirth, and prematurity |
| HIV: human immunodeficiency virus. |
| Age extremes: infants and elderly |
| Pregnancy |
| Bowel surgery |
| Immunosuppression, especially tuberculosis, asplenia, corticosteroid treatment, transplantation, HIV infection, and agammaglobulinemia |
| Cancer |
| Diabetes mellitus |
| Liver disease |
| Kidney disease |
| Alcohol consumption |
| Chronic obstructive pulmonary disease |
| Cardiovascular disease |
| Type of Campylobacter infection (listed in decreasing frequency) | Treatment of Campylobacter infection |
|---|---|
| All extraintestinal infections are considered complicated, but they are mentioned separately due to their rarity and severity. Symptomatic management is indicated in all patients. Although antibiotic treatment is indicated in complicated intestinal and systemic infections, the first-line treatment and the duration differ. HIV: human immunodeficiency virus. | |
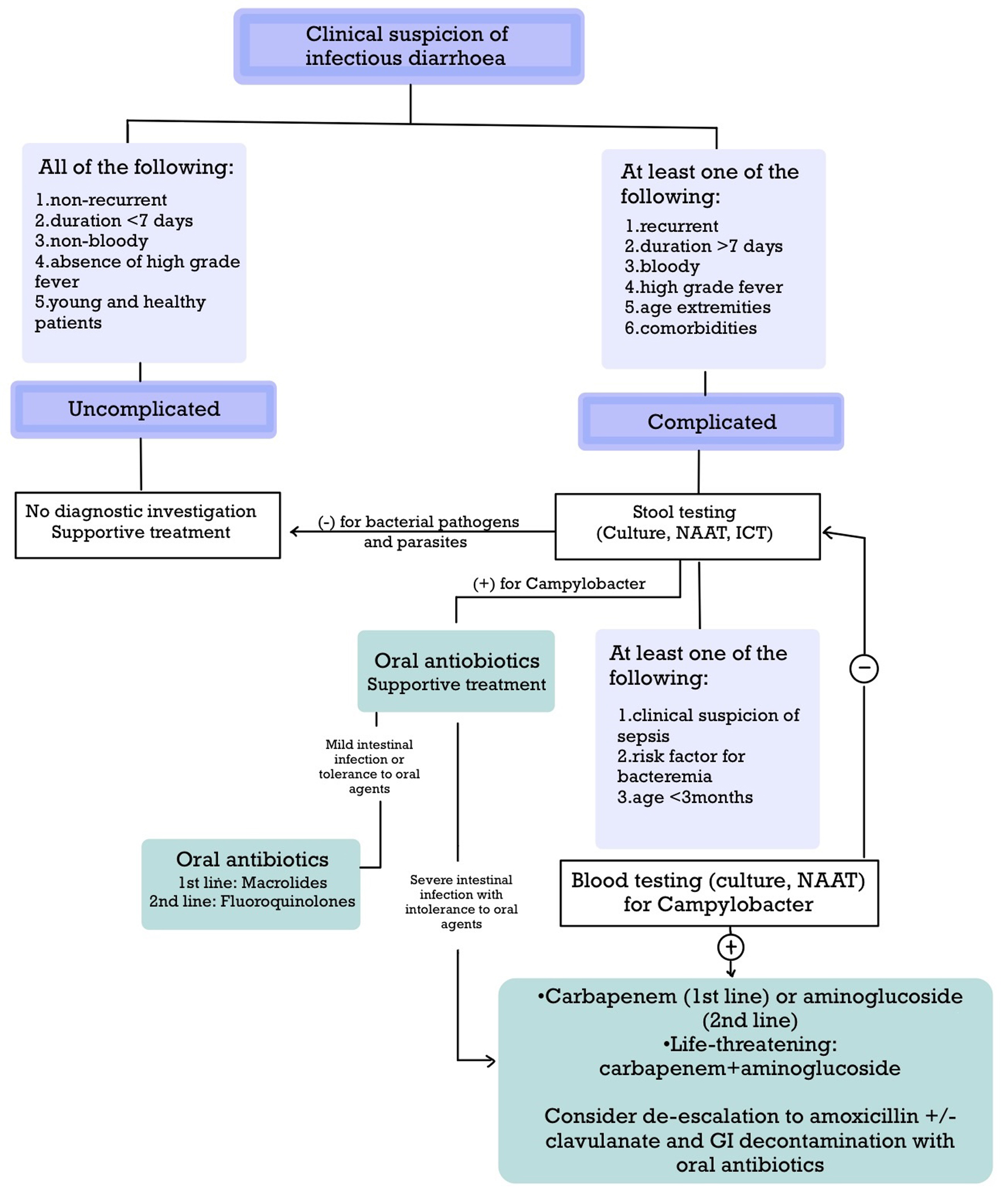
| 1. Uncomplicated intestinal infection: It is defined as non-recurrent gastroenteritis lasting less than 7 days without blood, high-grade fever, and extraintestinal complications in young and otherwise healthy patients. | 1. Uncomplicated intestinal infection: 1) Symptomatic management: repletion of fluids and electrolytes, antiemetics, and analgesics. 2) Probiotics may be helpful. 3) Consider zinc supplementation in children 6 months to 5 years with malnutrition or from areas with high prevalence of zinc deficiency. 4) No antibiotic treatment. |
| 2. Complicated intestinal infection: It is defined in the presence of any of the following criteria: 1) Bloody diarrhea; 2) High-grade fever; 3) Recurrence; 4) Duration greater than 7 days; 5) High-risk features: age extremities, pregnancy, immunosuppression (including HIV infection, agammaglobulinemia, transplantation, tuberculosis, asplenia, corticosteroid use), cancer, diabetes mellitus, liver disease, kidney disease, alcohol abuse, chronic obstructive pulmonary disease, and cardiovascular disease; 6) Extraintestinal complications. | 2. Complicated intestinal infection: 1) Symptomatic management: repletion of fluids and electrolytes, antiemetics, and analgesics. 2) Probiotics may be helpful; avoid them in patients with critical illness, e.g. hospitalized patients, or impaired immunity due to the risk of bacteremia. 3) Consider zinc supplementation in children 6 months to 5 years with malnutrition or from areas with high prevalence of zinc deficiency. 4) Antibiotic treatment should be administered; macrolides are the first-line choice, while fluoroquinolones are a second-line choice. Other alternatives include tetracyclines, trimethoprim-sulfamethoxazole (TMP-SMX), amoxicillin/clavulanate, and third-generation cephalosporins. 5) The course of antibiotic treatment usually lasts 3 days or until symptom resolution. Consider longer courses of 7 - 14 days in the presence of complications or impaired immunity. 6) Consider the combination of antimotility agents, e.g. loperamide, with antibiotics. 7) Consider the use of a carbapenem with or without an aminoglycoside in those with severe disease and intolerance to oral antibiotics. |
| 3. Campylobacter bacteremia/meningitis | 3. Campylobacter bacteremia/meningitis: 1) Symptomatic management: repletion of fluids and electrolytes, antiemetics, analgesics. 2) Antibiotic treatment for at least 3 - 4 weeks; carbapenems with or without an aminoglycoside are the first-line choice. 3) Consider de-escalation treatment with amoxicillin with or without clavulanic acid. 4) Consider gastrointestinal decontamination with oral antibiotics, such as macrolides or tetracyclines. 5) Consider surgical management in the presence of complications. |
| Diagnostic tests | Indications |
|---|---|
| The indications for stool testing are shown in the first line according to the recommendations of IDSA, ACG, AAP, and AMSUS; these patients are more likely to develop unfavorable outcomes, such as dehydration and sepsis. The indications for blood testing are shown in the second line according to the recommendations of IDSA and AAP; these patients are more likely to develop bacteremia and extraintestinal infections. AAP: American Academy of Pediatrics; ACG: American College of Gastroenterology; AMSUS: Association of the Military Surgeons in the United States; ICT: immunochromatography; IDSA: Infectious Diseases Society of America; NAAT: nucleic acid amplification test. | |
| Stool testing (culture, NAAT, ICT) | 1) Fever; 2) Bloody or mucus diarrhea; 3) Abdominal pain; 4) Immunocompromised status; 5) Duration greater than 7 days; 6) Suspicion of sepsis; 7) Inadequate response to antibiotics; 8) Epidemic outbreak. |
| Blood cultures or NAAT | 1) Clinical suspicion of sepsis; 2) Risk factors for Campylobacter extraintestinal infection (Table 1); 3) Age lower than 3 months old. |
| Diagnostic tests | Culture | Molecular testing (NAAT) | ICT |
|---|---|---|---|
| CIDT: culture-independent technique; CSF: cerebrospinal fluid; ICT: immunochromatography; NAAT: nucleic acid amplification test. | |||
| Advantages | 1) Antibiotic susceptibility pattern; 2) Available for stool and non-stool specimens, e.g. blood, CSF. | 1) Faster results within hours; 2) Higher sensitivity (especially for Campylobacter non-jejuni/coli); 3) Simultaneous testing for multiple pathogens; 4) Available for stool and non-stool specimens, e.g. blood, CSF. | 1) Faster results within minutes; 2) High specificity. |
| Disadvantages | 1) Prolonged incubation period (at least 48 - 72 h); 2) Special requirements: rapid preparation, medium with selective antibiotics, microaerophilic conditions, and temperature; 3) Lower sensitivity for Campylobacter non-jejuni/coli. | 1. Lower specificity due to the detection of nucleic acids instead of viable pathogens; 2. Detection of enteropathogens in a lower microbial load causing asymptomatic infection; detection of multiple pathogens is a common problem; 3. No information regarding antibiotic susceptibility; combination with culture is generally recommended. | 1) No information regarding antibiotic susceptibility; combination with culture is generally recommended; 2) Relatively new technique; fewer number of studies; 3) Available for stool specimens only. |