Figures
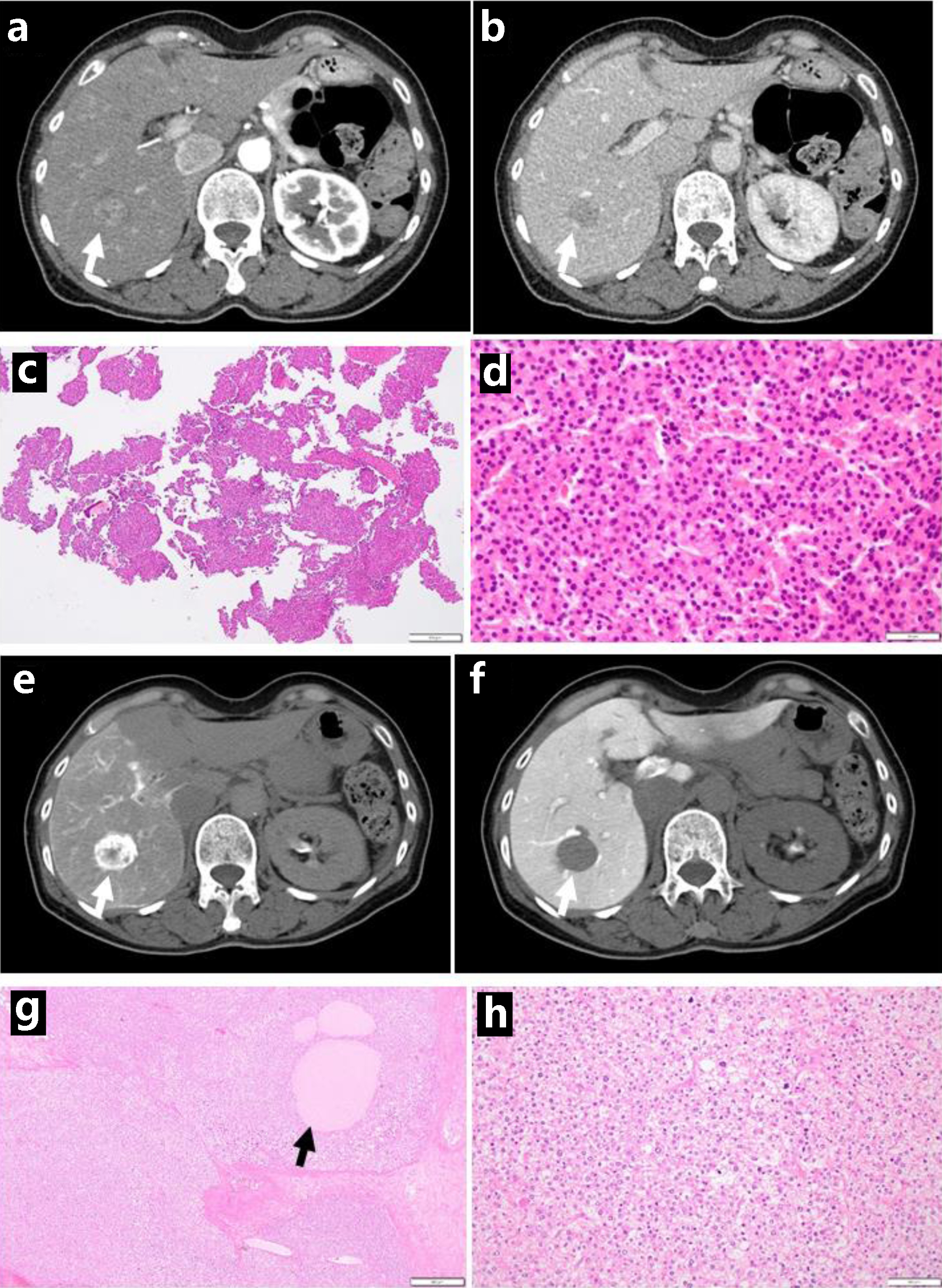
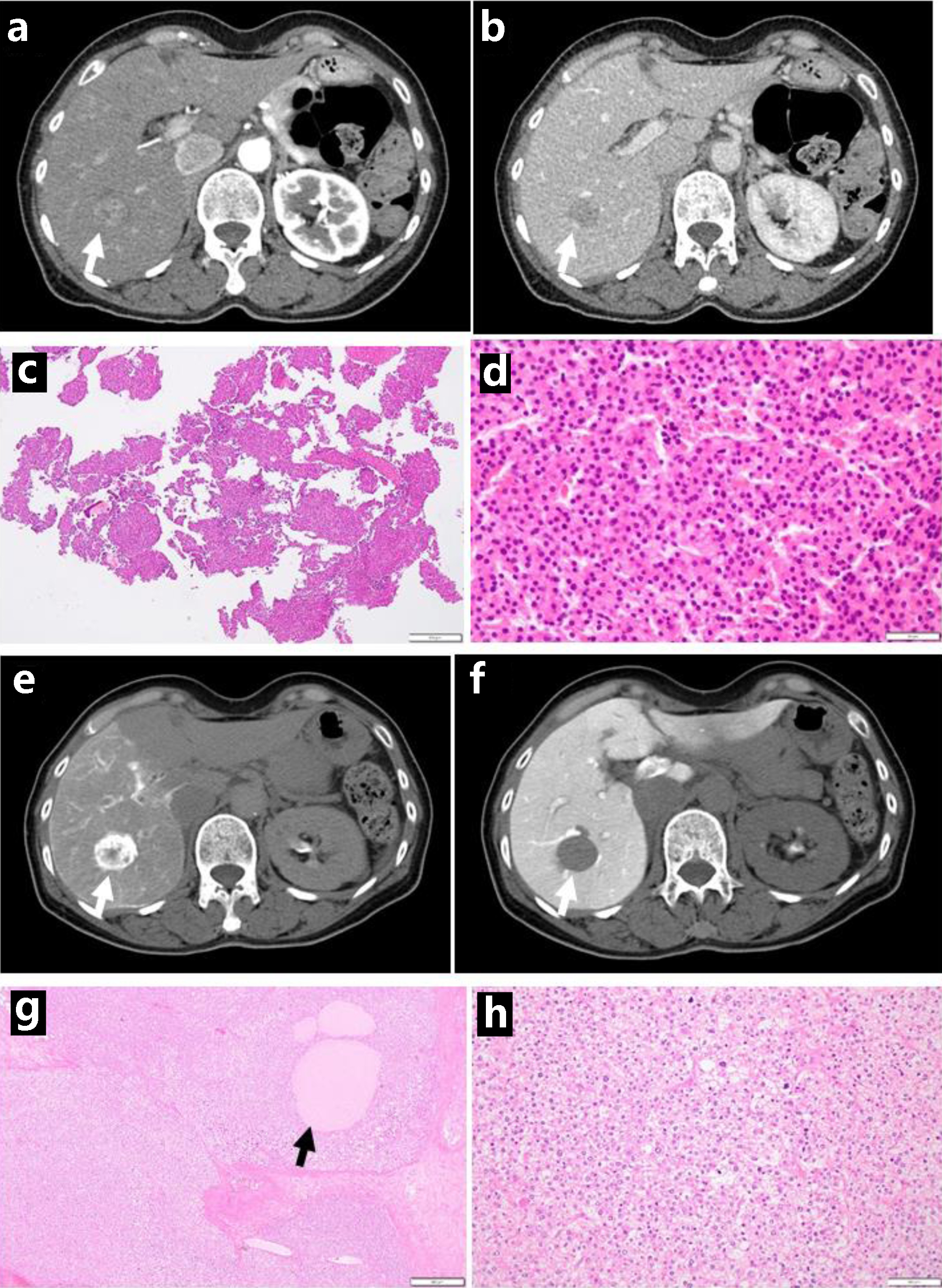
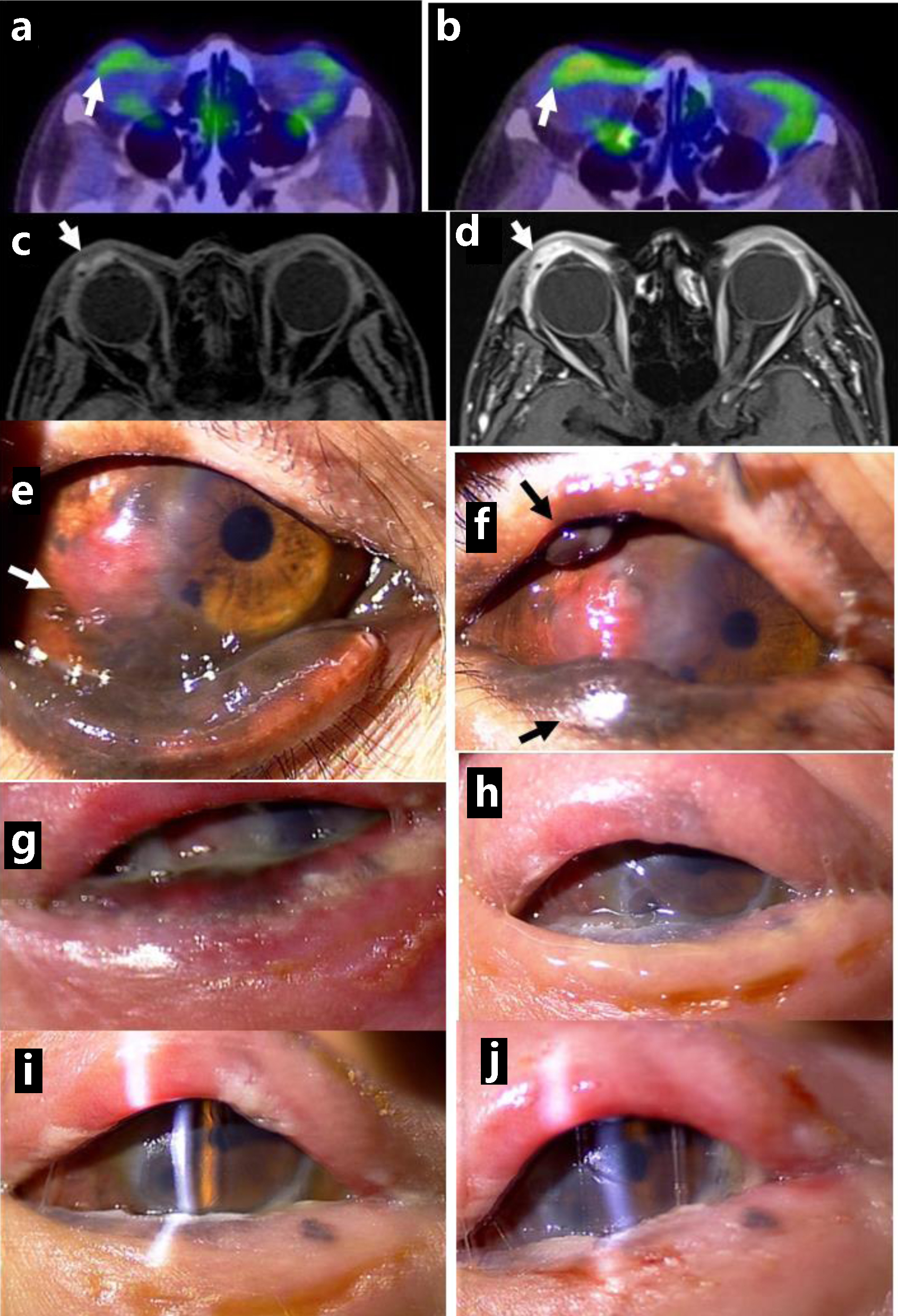
Figure 1. Dynamic-enhanced computed tomography scans with enhancement at the initial visit, showing early-phase enhancement (arrow, a) and late-phase washout (arrow, b). Needle liver biopsy, showing hepatocellular carcinoma (c in low magnification, d in high magnification). Computed tomography during hepatic arteriography with marked staining (arrow, e), in contrast with computed tomography during arterial portography with no staining (arrow, f), consistent with hepatocellular carcinoma. Note foamy cells with degeneration (h) and necrotic cell debris spaces (arrow, g) after transcatheter arterial chemoembolization, compared with viable tumor cells (d). Scale bar = 500 µm in c and g, 50 µm in d and h.
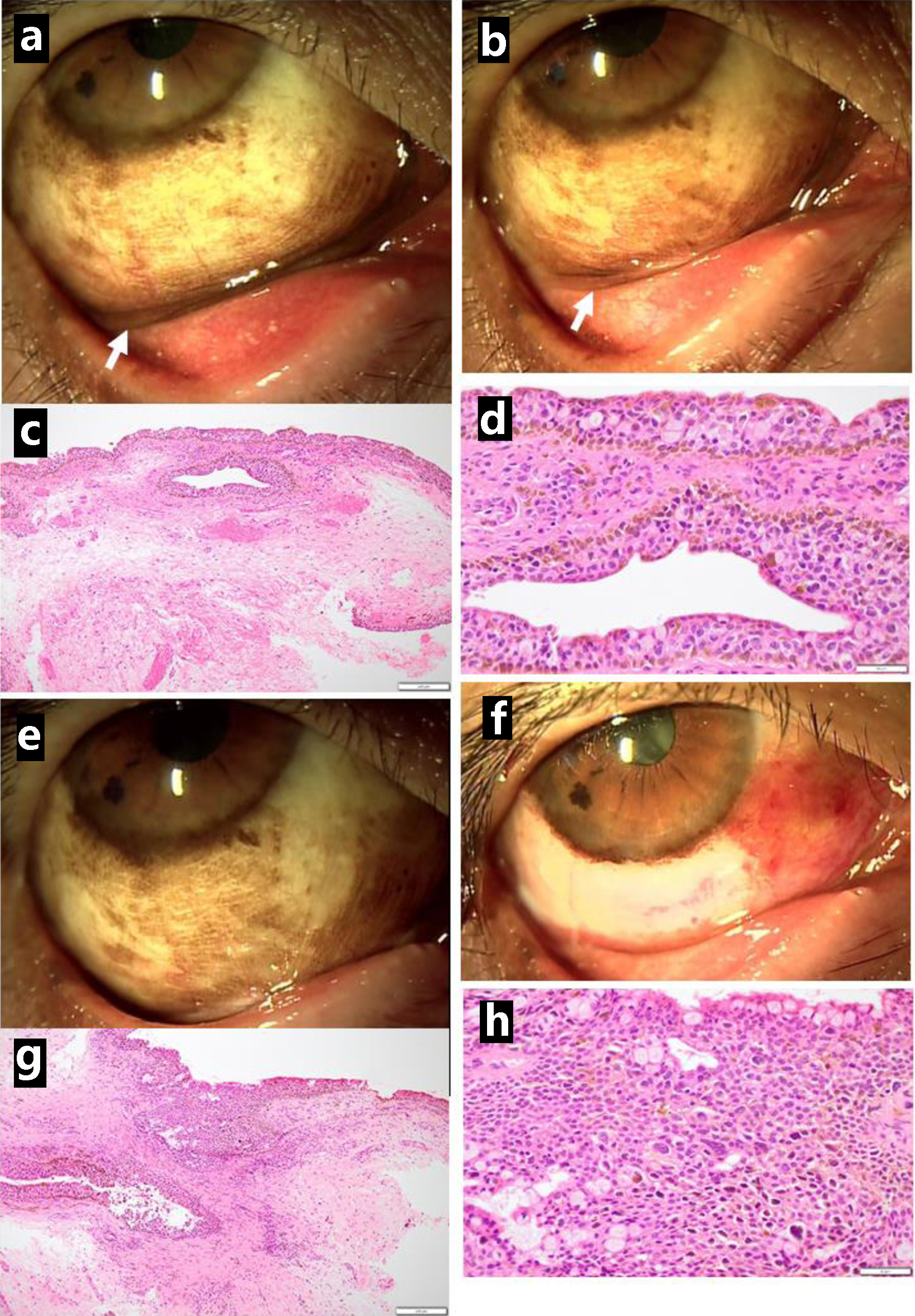
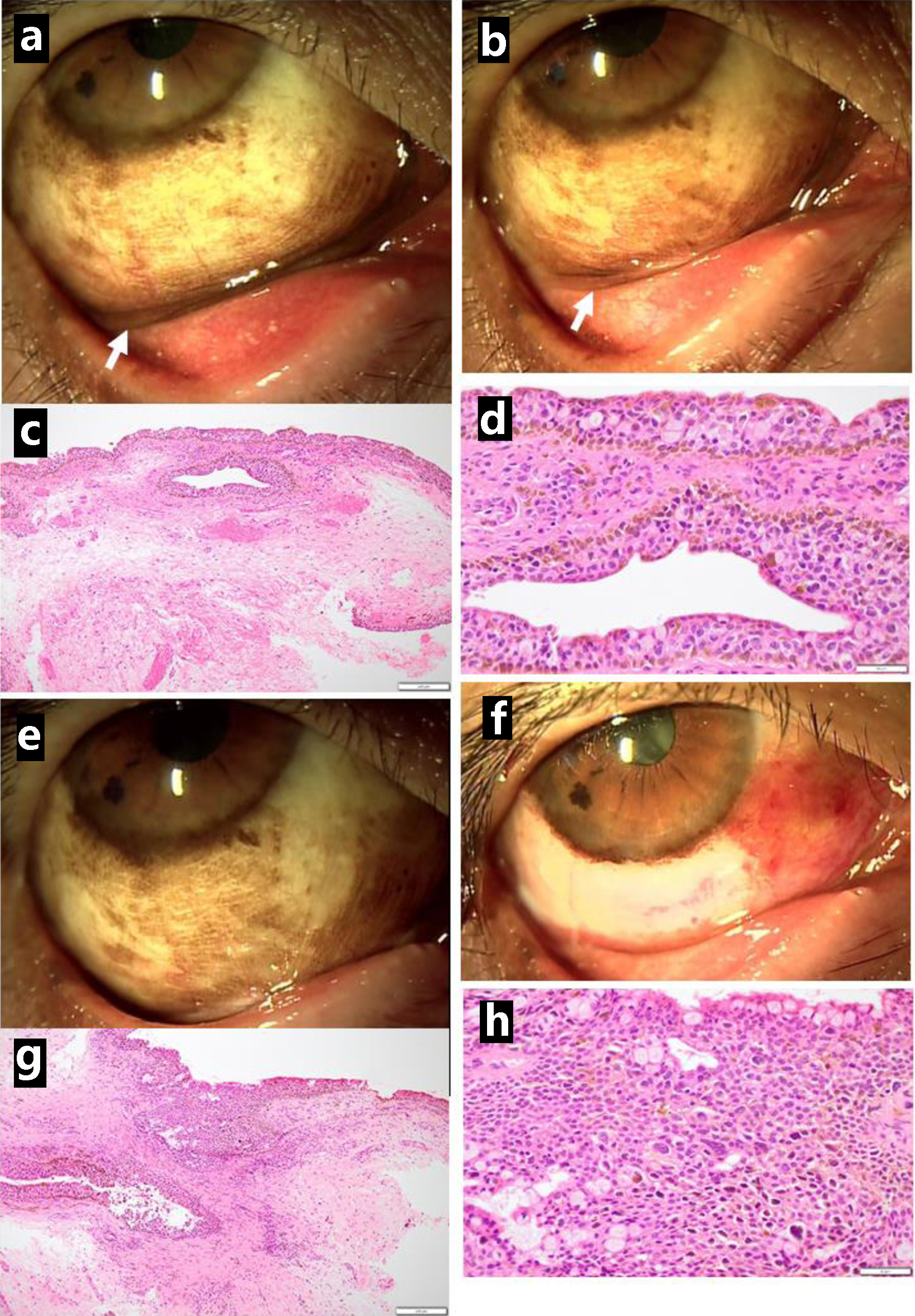
Figure 2. Pigmented lesions mainly along the lower conjunctival fornix (arrow, a) in the right eye just before excisional biopsy at the initial visit and reduced pigmented lesions in the fornix (arrow, b) one month later. Excisional biopsy showing conjunctival malignant melanoma in situ (c in low magnification, d in high magnification). Three months after the initial visit, the lower bulbar conjunctiva excised as wide as possible (presurgical photo in e, postsurgical photo in f). The excised tissue diagnosed as conjunctival malignant melanoma in situ (g in low magnification, h in high magnification). Scale bar = 200 µm in c and g, 50 µm in d and h.
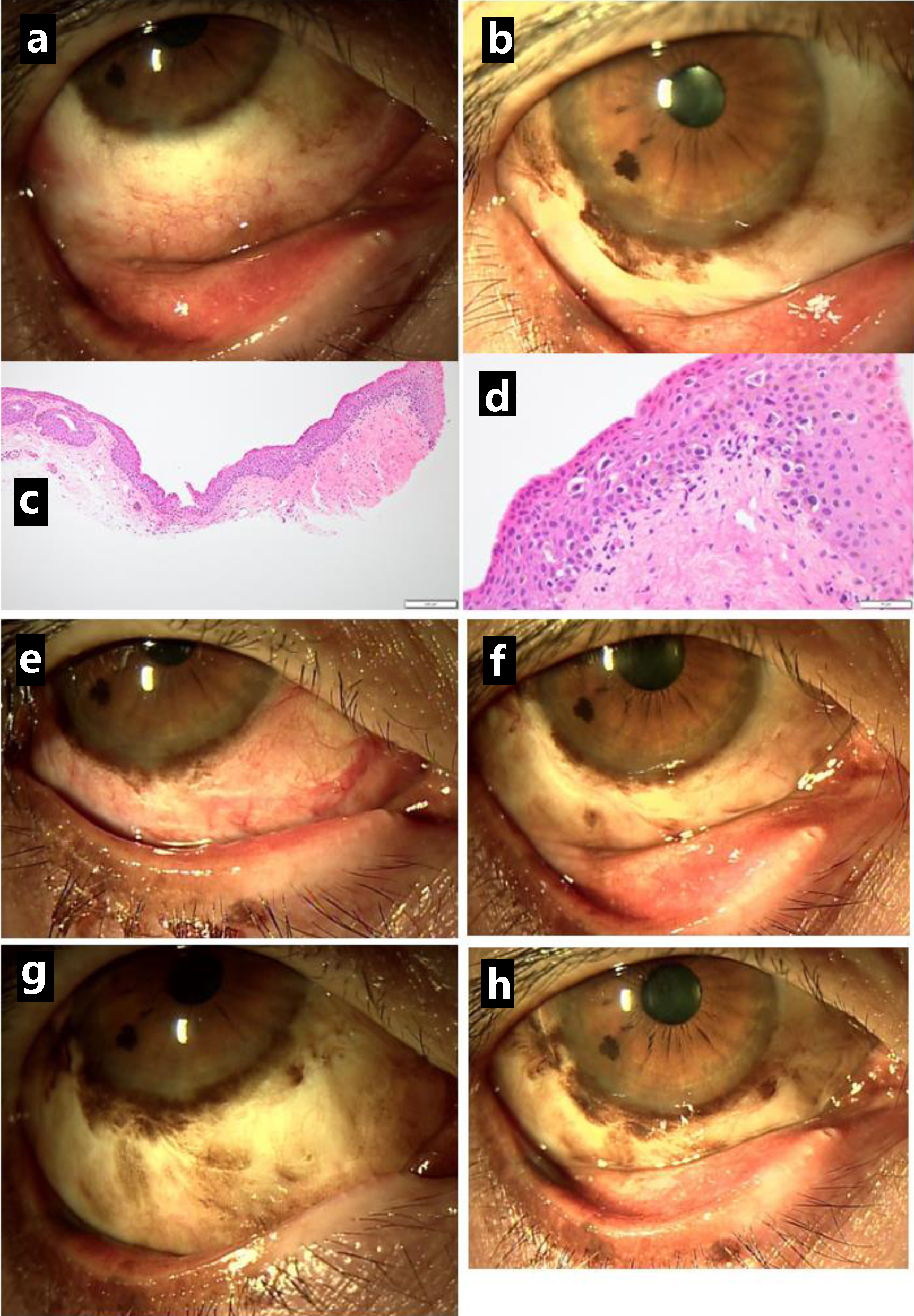
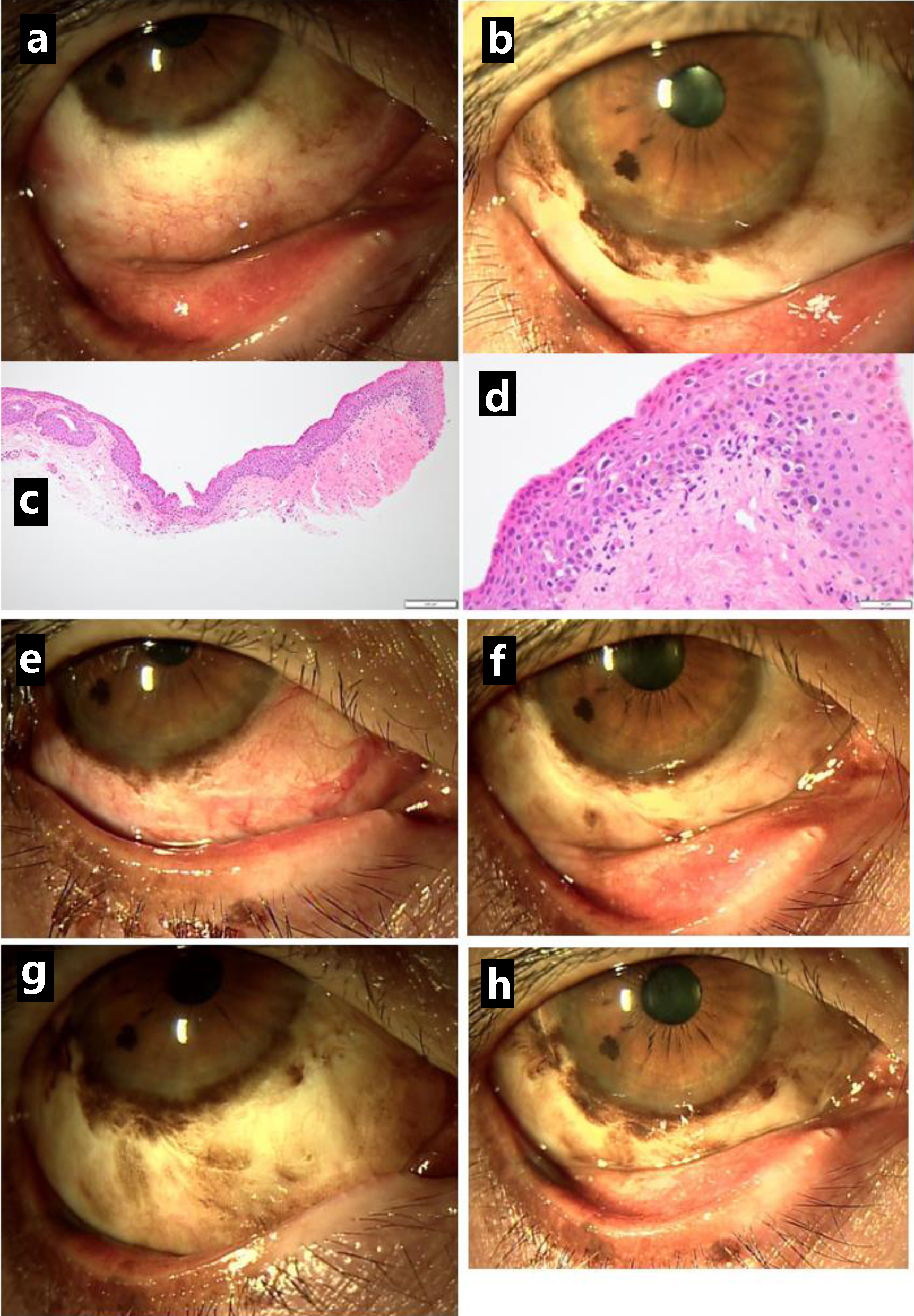
Figure 3. Clear lower bulbar conjunctiva (a) in the right eye one month after the resection but pigmented lesions along the corneal limbus (b) relapsing in half a year. The excision of relapsed lesion showing conjunctival malignant melanoma in situ (c in low magnification, d in high magnification). Relatively clear lower bulbar conjunctiva just after the excision (e) and one month later (f), 1 year from the initial visit. The pigmented lesions gradually increase half a year after the excision (g) and 1 year later (h), 2 years from the initial visit. Scale bar = 200 µm in c, 50 µm in d.
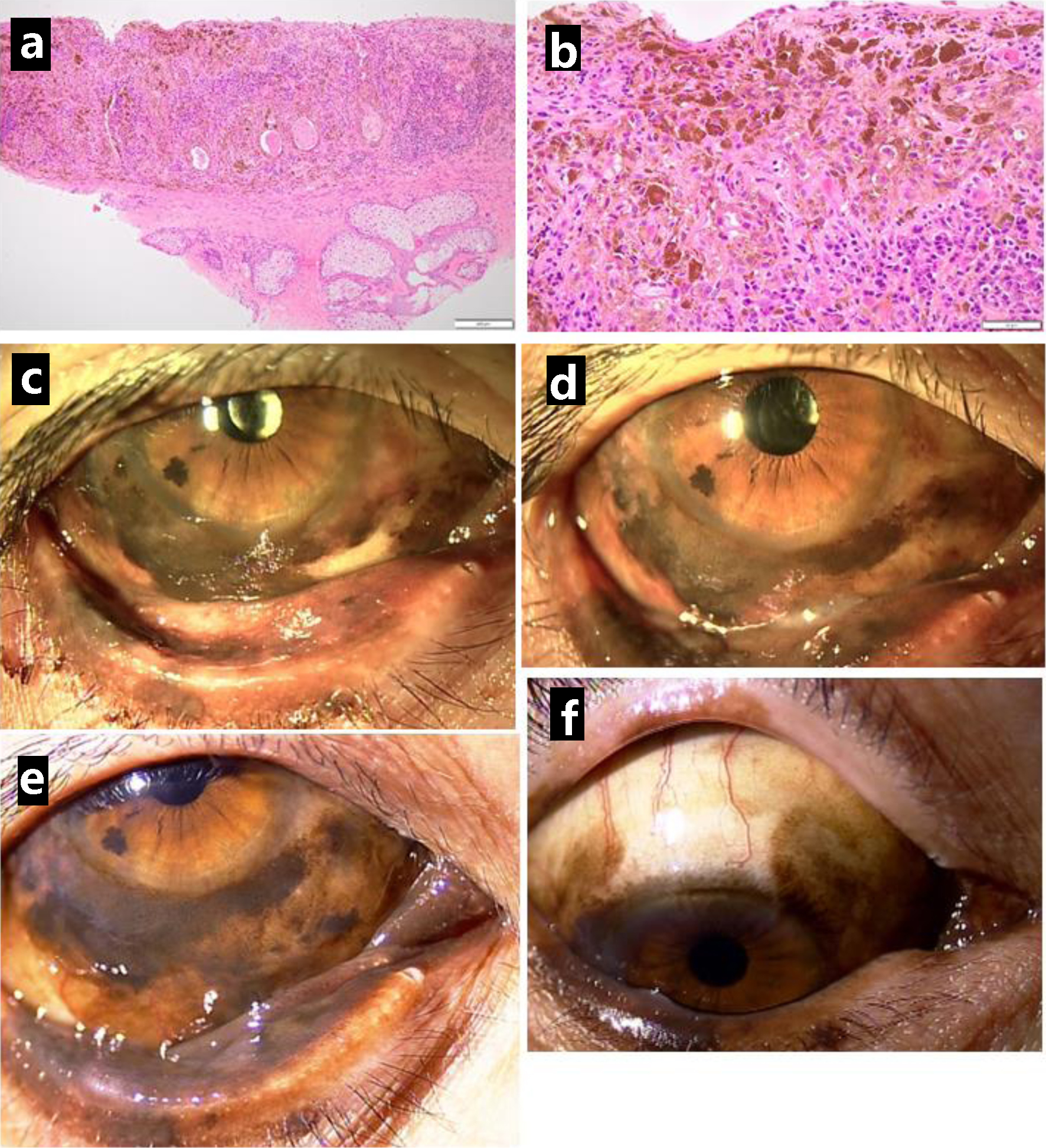
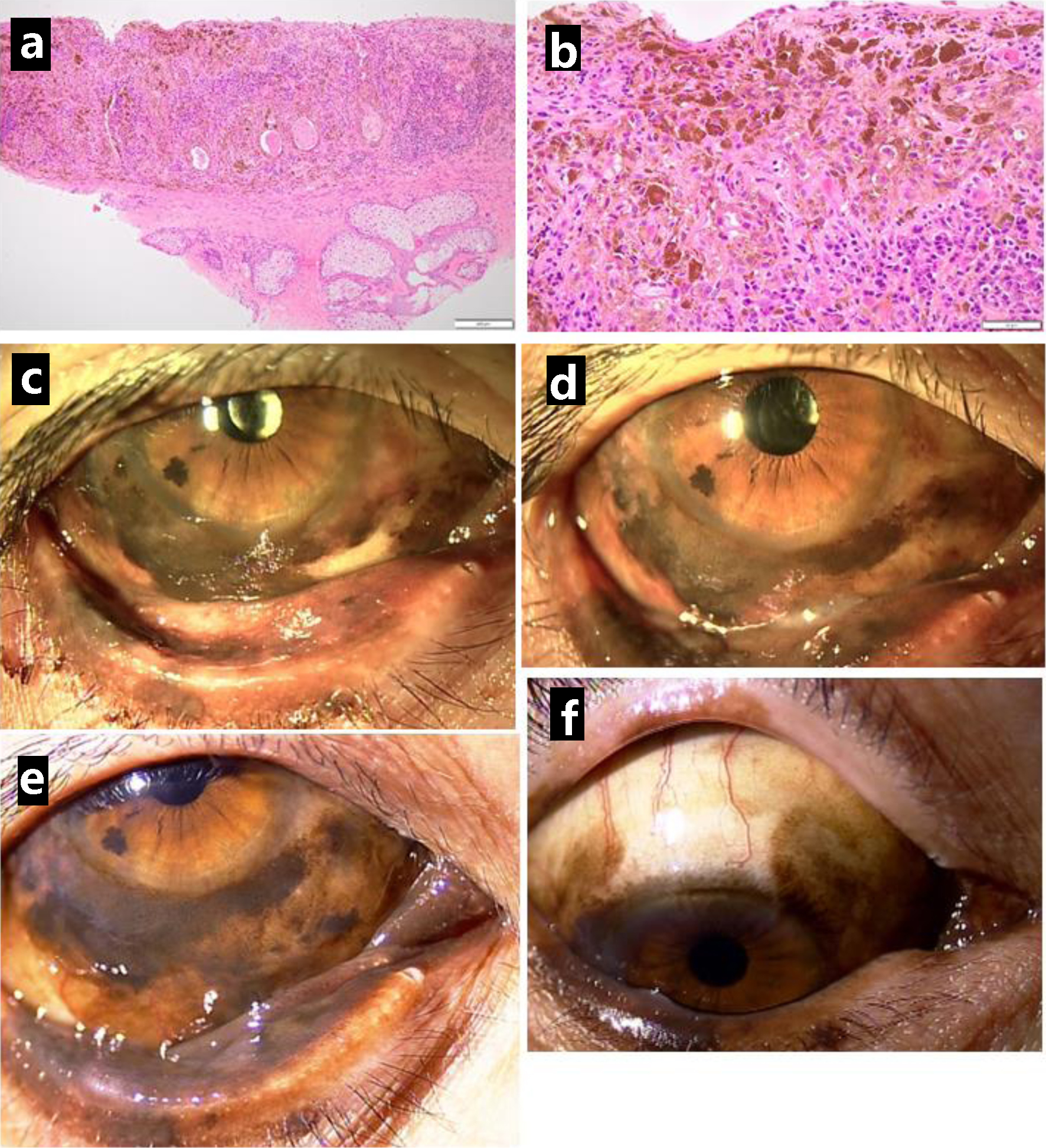
Figure 4. Resection of lower eyelid-edge pigmented lesion in the right eye, 2.5 years after the initial visit, showing malignant melanoma in situ (a in low magnification, b in high magnification). Photos just before the resection (c) and 1 year later (d), 3.5 years from the initial visit. Pigmented lesions spreading to the lower palpebral conjunctiva (e) and upper bulbar conjunctiva (f) half a year later, 4 years from the initial visit. Scale bar = 200 µm in a, 50 µm in b.
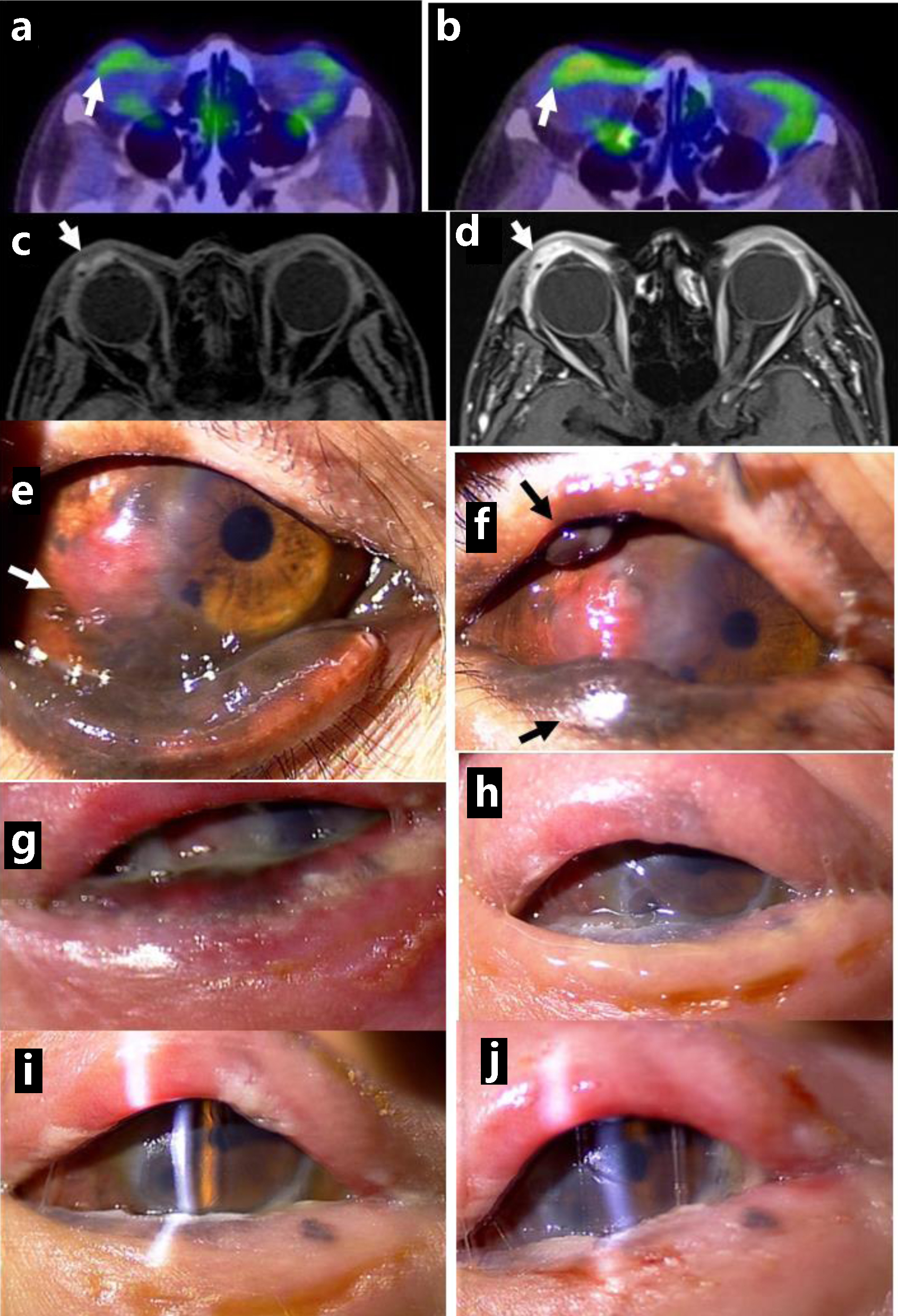
Figure 5. Positron emission tomography, showing no abnormal uptake in ocular surface of the right eye at the initial visit (arrow, a) and mildly increased uptake 5 years from the initial visit (arrow, b). Magnetic resonance imaging with enhancement, showing saucer-like ocular surface lesion on the right side (arrow, c) with marked enhancement in arterial phase (arrow, d), 5.5 years from the initial visit. Non-pigmented nodular lesion on the temporal bulbar conjunctiva along the corneal limbus (arrow, e), 5 years from the initial visit, and pigmented nodular lesions in the upper and lower eyelids (arrows, f). 3 months later. No pigmented lesion in the eyelids and ocular surface immediately after the completion of proton beam therapy (g), 1 month later (h), 3 months later (i), and 5 months later (j). Note clear cornea with slit-lamp examination (i, j).