Nephronophthisis and Retinitis Pigmentosa (Senior-Loken Syndrome) After Living-Donor Kidney Transplantation: Twelve-Year Follow-Up in a Young Woman
DOI:
https://doi.org/10.14740/jmc4356Keywords:
Retinitis pigmentosa, Nephronophthisis, Senior-Loken syndrome, Kidney transplantation, Living donor, Kidney biopsy, Pathology, Computed tomography scan, Ciliopathy, Optical coherence tomographyAbstract
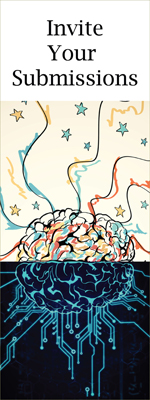
Senior-Loken syndrome is a hereditary ciliopathy with recessive trait that manifests as nephronophthisis and retinitis pigmentosa. This report described an 18-year-old woman who was referred to a University Hospital to set up a treatment plan for chronic renal failure of an unknown cause. She had experienced nocturnal polyurea from the age of 12 years and was found to have an elevated level of serum creatinine at 3 mg/dL at the age of 15 years. She underwent renal biopsy at a hometown regional hospital which showed global glomerulosclerosis in six of the 13 glomeruli examined, renal tubular dilation in irregular shape, and marked interstitial fibrosis with lymphocytic infiltration. At the age of 19 years, she received a living-donor kidney transplant from her 46-year-old father as a preemptive therapy. At surgery, biopsy of the father’s donor kidney showed two glomeruli with global sclerosis out of 24 glomeruli examined, in association with minimal interstitial fibrosis and lymphocytic infiltration. She began to have extended-release tacrolimus 4 mg daily and mycophenolate mofetil 1,000 mg daily. According to the standard protocol, she underwent biopsy of the transplanted donor kidney to reveal interstitial fibrosis and lymphocytic infiltration, in addition to no sign of rejection and no glomerular deposition of immunoglobulins and complements, both 4 weeks and 14 months after the kidney transplantation. At the age of 23 years, 4 years after the kidney transplantation, she was, for the first time, diagnosed retinitis pigmentosa, and hence, Senior-Loken syndrome. She was followed up in the stable condition with basal doses of tacrolimus 5 mg daily, mycophenolate mofetil 1,000 mg daily, and prednisolone 5 mg daily up until now in 12 years after the kidney transplantation. The interstitial fibrosis with lymphocytic infiltration in the donor kidney might be a milder presentation of the disease with recessive inheritance.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.