Successful Treatment of Primary Central Nervous System T-Cell Lymphoma With Induction Chemotherapy Followed by Consolidation With High-Dose Chemotherapy and Autologous Stem Cell Rescue
DOI:
https://doi.org/10.14740/jmc5130Keywords:
Primary CNS T-cell lymphoma, Autologous stem cell transplant, Complete remission, High-dose chemotherapyAbstract
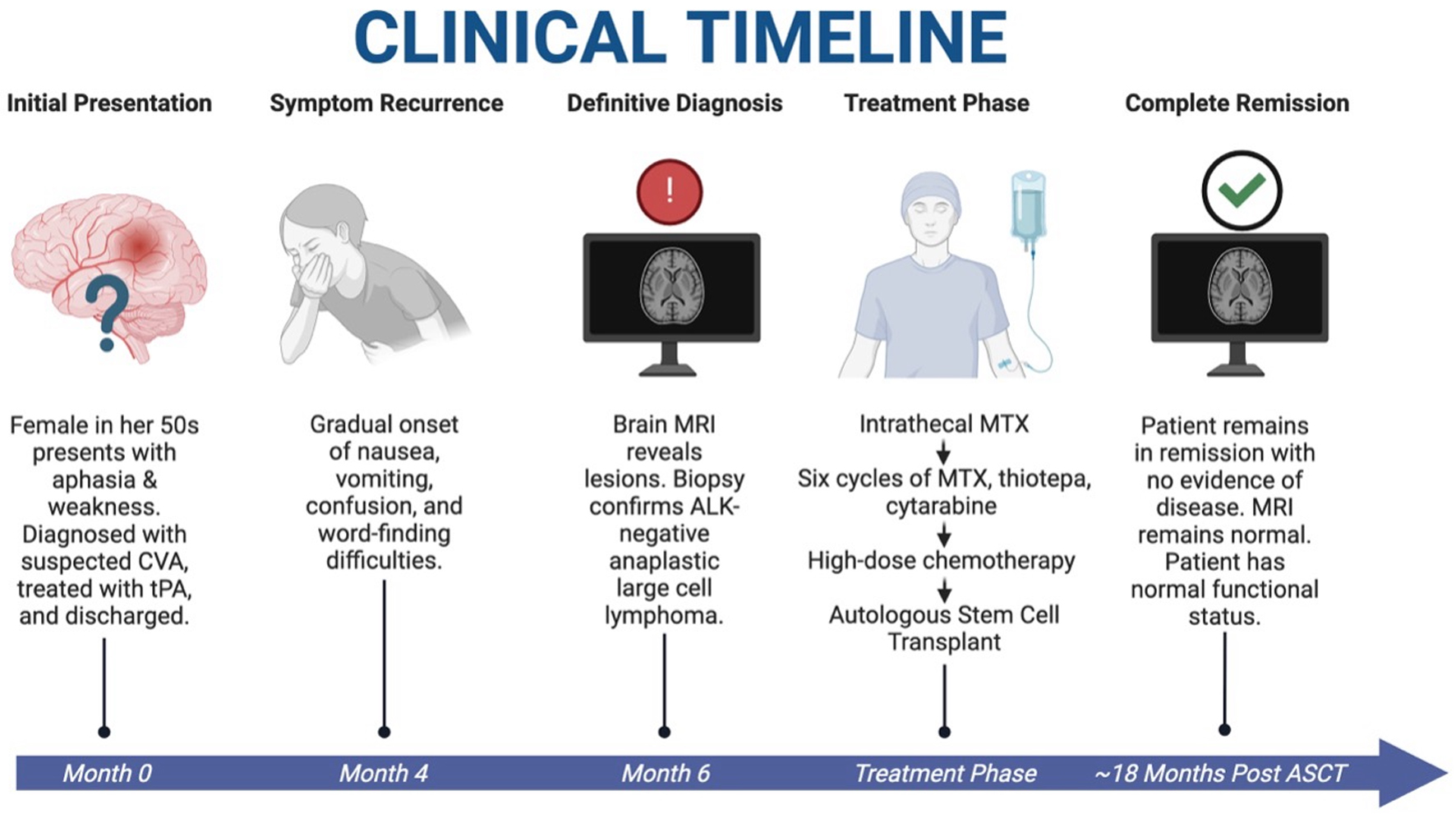
Primary central nervous system T-cell lymphoma (PCNSTL) is an exceptionally rare subtype of non-Hodgkin lymphoma, comprising only 2% of primary CNS lymphoma cases. Due to its rarity, PCNSTL is often misdiagnosed, lacks standardized treatment guidelines, and carries a poor prognosis. We present a unique case of a 59-year-old-woman with a history of hypertension and hyperlipidemia who initially presented with sudden-onset aphasia and right-sided weakness. Suspected initially of having a cerebrovascular accident (CVA), she received tenecteplase and underwent investigation of CVA, which was largely unremarkable. Six months later, she returned with progressive nausea, vomiting, confusion, and word-finding difficulties. A magnetic resonance imaging (MRI) of the brain showed lesions in the left cerebellum and frontal lobe with vasogenic edema. A suboccipital craniotomy and biopsy confirmed anaplastic lymphoma kinase (ALK)-negative anaplastic large cell lymphoma. Positron emission tomography-computed tomography (PET-CT) showed no systemic disease and cerebrospinal fluid (CSF) analysis showed lymphomatous involvement. The patient was initiated on six cycles of methotrexate, cytarabine, and thiotepa (MATRix regimen without rituximab), followed by high-dose chemotherapy (HDC) with carmustine and thiotepa and autologous stem cell transplantation (ASCT). She tolerated treatment and transplant without complications and remains in complete remission 18 months post-transplant. To our knowledge, this is the first reported case of PCNSTL treated successfully with MATRix followed by HDC-ASCT. This case highlights the importance of considering rare CNS lymphomas in patients with atypical neurologic presentations and suggests the use of HDC-ASCT as a promising approach in a disease with no established standard of care.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.