Treatment of Invasive Fungal Disease During Therapy for Acute Lymphoblastic Leukemia
DOI:
https://doi.org/10.14740/jmc5066Keywords:
Invasive fungal infection, ALL, Antifungal prophylaxisAbstract
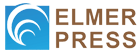
Invasive fungal diseases (IFDs) are one of the leading causes of death in acute leukemia (AL) patients. Because of the possibility of fungal relapse, patients who survive IFDs may have difficulty in completing the whole chemotherapy plan. Our case report presents two cases of IFD with aspergillosis in children with precursor B-cell acute lymphoblastic leukemia (pre-B-ALL). Two 9-year-old female patients were diagnosed with pre-B-ALL that were on the pre-B-ALL protocol: CALL08, Arm-C (high-risk arm), and the supportive therapy. They were both on Arm-C of the CALL08 protocol (high risk based on COG232). Then, the patients experienced severe febrile neutropenia. Patient 1 was during consolidation, and patient 2 was during interim maintenance I. Both experienced prolonged febrile neutropenia. As febrile neutropenia continued for more than 5 days, a fungal workup was conducted, including computed tomography (CT) scans of the sinuses, chest, and abdomen, as well as serum tests for galactomannan and (1→3)-β-D-glucan (BDG). Caspofungin treatment was started. Fungal workup results showed lung and liver nodules in one patient and lungs, liver, and spleen in the other. There were about 4 weeks of severe fevers and neutropenia, despite the use of broad-spectrum antibiotics. A decision was taken to interrupt chemotherapy for both patients. Voriconazole was added to caspofungin. Biopsies confirmed the diagnosis to be severe fungal infection with invasive aspergillosis. After that, high fevers and neutropenia slowly recovered, and a repeated CT scan of abdomen showed good improvement in the lesion’s number and size. After 6 - 8 weeks of interruption, chemotherapy was resumed. We observed that with the implementation of combination antifungal therapy with voriconazole and caspofungin for 6 weeks and then single antifungal therapy (voriconazole orally) for another 6 weeks, both patients recovered and became clinically stable and afebrile. Chemotherapy was on hold till they became better. In conclusion, primary and secondary antifungal prophylaxis are recommended for ALL patients. Chemotherapy discontinuation is decided on an individual basis according to the severity of the fungal infection and disease status.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.