| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 17, Number 1, January 2026, pages 37-40
Acute Compartment Syndrome Following Non-Displaced Proximal Ulnar and Distal Radial Fractures in a Four-Year-Old Girl
Khalid Aloqeelya, Amal Yousifb, d, Fatima Aljaziric
aDepartment of General Pediatrics, King Saud University Medical City, Riyadh, Saudi Arabia
bDepartment of Emergency Medicine - Pediatric Emergency Unit, King Saud University Medical City, Riyadh, Saudi Arabia
cPediatric Emergency Department, Maternity and Children Hospital, Dammam, Saudi Arabia
dCorresponding Author: Amal Yousif, Department of Emergency Medicine - Pediatric Emergency Unit, King Saud University Medical City, Riyadh, Saudi Arabia
Manuscript submitted October 14, 2025, accepted December 12, 2025, published online December 24, 2025
Short title: ACS Following Non-displaced Forearm Fractures
doi: https://doi.org/10.14740/jmc5223
| Abstract | ▴Top |
Acute compartment syndrome (ACS) is a rare but limb-threatening emergency in children, usually associated with displaced fractures, crush injuries, or high-energy trauma. Prompt recognition and fasciotomy are essential to prevent permanent disability. An unusual case of ACS after non-displaced fractures is presented, challenging traditional risk factors. A healthy 4-year-old girl presented 12 h after a 2-m fall with severe forearm pain, swelling, an absent radial pulse, delayed capillary refill (3 - 4 s), and cold digits. Radiographs showed non-displaced proximal ulna and distal radius fractures. Emergency fasciotomy was performed based on clinical findings of ACS. ACS can occur in children after non-displaced fractures, even without conventional risk factors. Clinicians should rely on careful neurovascular assessment and clinical suspicion rather than fracture type or mechanism alone. Early recognition and surgical intervention are critical to preserve limb function.
Keywords: Acute compartment syndrome; Non-displaced fractures; Early recognition; Intervention; Children
| Introduction | ▴Top |
Acute compartment syndrome (ACS) is a medical emergency characterized by elevated interstitial pressure within a closed osteofascial compartment, leading to decreased tissue perfusion and ischemia [1]. The pathophysiological cascade typically begins with edema or bleeding in a fixed-volume compartment, raising venous and tissue pressure. When compartment pressure exceeds capillary perfusion pressure, muscle and nerve ischemia ensue [1]. Although this model presents a plausible, linear cascade of events, it is important to recognize that more complex mechanisms for this pathophysiology have also been described in the literature [2].
In the upper extremity, ACS involves several anatomical considerations. The forearm contains three main compartments: the volar compartment, the dorsal compartment, and the mobile wad (brachioradialis, extensor carpi radialis longus, and brevis), which primarily contains muscles involved in elbow flexion and wrist extension. The hand alone has ten distinct fascial compartments [1].
Fractures are the principal cause of ACS [3, 4], although iatrogenic causes have also been reported [5]. Atraumatic causes including hereditary angioedema, cellulitis, and osteomyelitis have also been reported [4, 6-9]. The incidence is fortunately rare, affecting 0.3% of pediatric patients after trauma [10]. The median age at presentation is 12 years, with girls accounting for 20% of cases compared to boys [11]. The upper limb is involved in 40% of cases compared to the lower limb [12], and the hand is affected in 35% of cases compared to the forearm [4].
Supracondylar fracture (SCF) is classically associated with pediatric ACS, most often involving the volar forearm compartment, but its incidence is still only 0.1-0.3% [13, 14]. Reported risk factors include male sex, high-energy trauma, and concomitant humeral and forearm fractures [15, 16].
Diagnosis of ACS is primarily clinical, based on findings such as severe pain, pain with passive movement, swelling, paresthesia, and diminished pulses [3]. Ancillary investigations may help when findings are equivocal [17]. Diagnosing ACS in children under 3 years is particularly challenging due to limited ability to verbalize symptoms [18]. Increased analgesic requirements and irritability have been reported as early indicators in this age group [19].
The prognosis of ACS depends on etiology and time to diagnosis [20]. Outcomes are generally favorable in pediatric cases, with one study reporting 74% excellent outcomes and 22% fair outcomes even when treatment was delayed [4]. No previous reports were identified describing ACS developing in a pediatric patient as a consequence of non-displaced forearm fractures [21, 22].
| Case Report | ▴Top |
This case report was prepared in accordance with institutional ethical guidelines and the CARE checklist for case report standards.
A previously healthy 4-year-old girl presented to the emergency department with acute left forearm pain following trauma sustained 12 h earlier. On the evening before presentation, she jumped from a cabinet approximately 2 m in height and landed on a carpeted floor. She primarily struck her left elbow and wrist, experiencing immediate severe pain while retaining the ability to move her hand freely. No other injuries were sustained, and there were no signs of trauma to other body regions.
Due to logistical constraints, the family could not seek immediate medical evaluation. About 3 h post-injury, the patient was assessed at a nearby primary care center. Since radiological imaging was unavailable, her family returned home. Over the next several hours, the pain progressively worsened. Approximately 1 h later (4 h post-injury), her left hand became swollen, and she experienced significant sleep disturbance overnight.
The following morning, about 12 h post-injury, her mother brought her to the emergency department, where she was triaged as Canadian Triage and Acuity Scale (CTAS) 2.
On physical examination, the patient appeared in severe distress with pain unrelieved by oral analgesics given earlier. She was unable to follow commands due to intense pain, making examination difficult. Marked swelling was noted over the distal third of the left forearm, wrist, and hand, with erythema and discoloration around the wrist. The hand was cold, with diffuse severe tenderness. She attempted to move her digits, wrist, and elbow but with extreme difficulty due to pain and was unable to be consoled.
Capillary refill was delayed (3 - 4 s), and the radial pulse was absent on palpation and undetectable by Doppler. However, pulse oximetry readings were obtainable from the left thumb, middle, and ring fingers. She was afebrile and hemodynamically stable except for tachycardia (heart rate 120 beats per minute (bpm)). Urgent radiographs demonstrated non-displaced proximal ulnar and distal radial fractures of the left forearm (Figs. 1, 2).
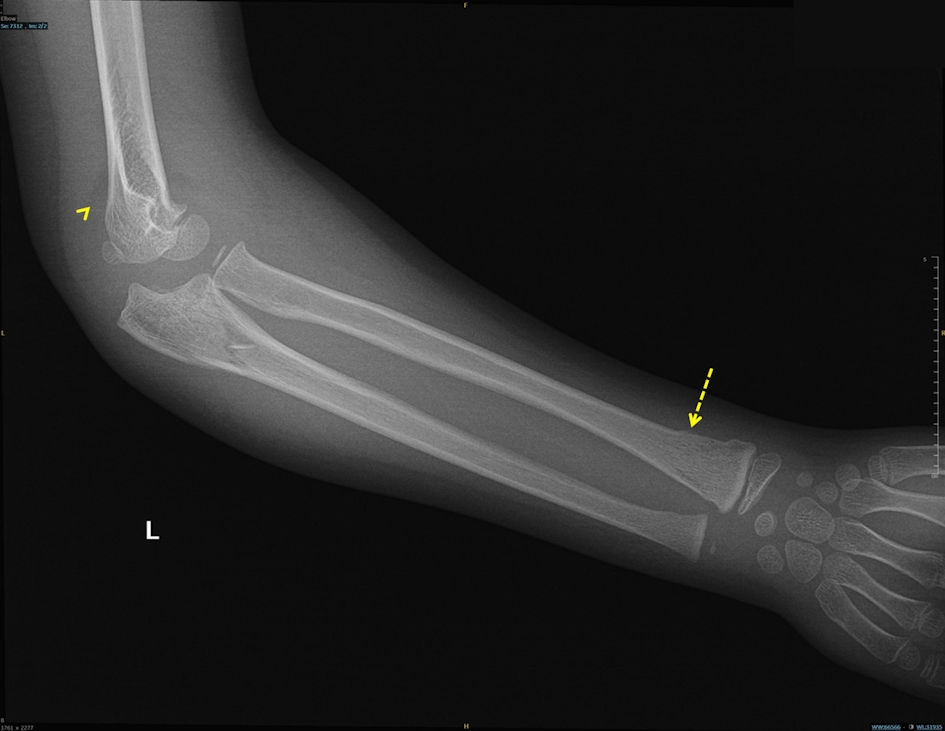 Click for large image | Figure 1. Lateral elbow radiograph demonstrating the posterior fat pad sign (arrowhead) and distal radial fracture (dashed arrow). |
 Click for large image | Figure 2. Anteroposterior forearm radiograph demonstrating proximal ulnar fracture (arrow). |
Preoperative laboratory studies were obtained immediately (complete blood count, coagulation profile, urea and electrolytes), and the patient received intravenous fluids and analgesia. Both the orthopedic and vascular surgery teams evaluated her immediately upon arrival, and she was transferred to the operating room for emergency fasciotomy. Multidisciplinary fasciotomies of the hand and forearm were performed under the care of orthopedic, vascular, and plastic surgery teams. Post-decompression assessment with Doppler confirmed intact ulnar and radial pulses.
Postoperatively, the patient required additional interventions, including serial surgical debridement and subsequent skin grafting. Despite these extensive efforts, she developed profound motor deficits in the affected hand, characterized by complete loss of active wrist and digit flexion and extension. The hand remained in a non-functional position with significant stiffness limiting passive range of motion. She was subsequently transferred to a specialized rehabilitation facility for intensive physiotherapy and ongoing care.
| Discussion | ▴Top |
This patient presented with high-energy trauma to the left forearm, accompanied by classic clinical features of ACS (severe pain, swelling, and absent radial pulse) following a 12-h delay in presentation. Radiographs revealed two non-displaced fractures (proximal ulna and distal radius). No previous reports were identified describing ACS developing in a pediatric patient as a consequence of non-displaced forearm fractures.
A systematic literature review was conducted using PubMed, EMBASE, and Google Scholar from inception to December 2025 with search terms: “acute compartment syndrome,” “pediatric,” “non-displaced forearm fracture,” “radius,” and “ulna.” The search was limited to English-language publications. No prior pediatric cases of ACS from combined non-displaced proximal ulnar and distal radial fractures were identified.
A recent systematic review of combined humeral and forearm fractures confirmed that all reported cases involved displacement [21].
A plausible explanation for ACS in this case is the presence of multiple fractures within the same extremity. As previously described, bleeding and edema within a closed osteofascial compartment can elevate pressure above capillary perfusion pressure, ultimately causing ischemia [1]. Taken together, the high-energy mechanism, potential soft tissue damage, and multiple fractures within one limb likely contributed to the development of ACS in this child and highlighted the importance of obtaining a detailed history of the mechanism of injury.
This case underscores the principle that ACS is a clinical diagnosis. Radiographs and fracture morphology cannot reliably exclude ACS. Absence of classic risk factors should not delay surgical evaluation. Any delay in recognition or intervention can result in irreversible tissue injury and permanent disability, as reflected in the patient’s persistent motor deficits despite timely fasciotomy and multidisciplinary care.
While this single case report has inherent limitations, it demonstrates an important clinical principle: ACS risk assessment should prioritize mechanism of injury and clinical findings over radiographic fracture patterns, particularly in pediatric patients
Conclusions
This case highlights the importance of careful neurovascular assessment in pediatric patients with fractures. ACS can develop even after non-displaced fractures and in the absence of recognized risk factors. Clinicians should maintain a high index of suspicion and prioritize clinical findings over imaging. Taken together, the high-energy mechanism, potential soft tissue damage, and multiple fractures within one limb likely contributed to the development of ACS in this child. These factors also highlight the importance of obtaining a detailed history of the mechanism of injury. Multiple non-displaced fractures in the same limb may precipitate ACS, as demonstrated in this report. Early recognition and prompt surgical intervention remain critical to preserving limb function.
Acknowledgments
None to declare.
Financial Disclosure
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that they have no conflicts of interest related to this publication.
Informed Consent
Written informed consent was obtained from the patient’s legal guardian(s) for publication of the clinical details and any accompanying images. All efforts were made to ensure patient anonymity.
Author Contributions
Dr. Khaled Aloqeely served as the primary author, drafted the manuscript, conducted the comprehensive literature review, and collected clinical data. Dr. Amal Yosif supervised patient management, conceived the case report concept, and provided critical review of the manuscript. Dr. Fatima Aljaziri provided direct patient care, made the initial diagnosis, and contributed to manuscript revision.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Donaldson J, Haddad B, Khan WS. The pathophysiology, diagnosis and current management of acute compartment syndrome. Open Orthop J. 2014;8:185-193.
doi pubmed - Frink M, Hildebrand F, Krettek C, Brand J, Hankemeier S. Compartment syndrome of the lower leg and foot. Clin Orthop Relat Res. 2010;468(4):940-950.
doi pubmed - Gottlieb M, Adams S, Landas T. Current approach to the evaluation and management of acute compartment syndrome in pediatric patients. Pediatr Emerg Care. 2019;35(6):432-437.
doi pubmed - Kanj WW, Gunderson MA, Carrigan RB, Sankar WN. Acute compartment syndrome of the upper extremity in children: diagnosis, management, and outcomes. J Child Orthop. 2013;7(3):225-233.
doi pubmed - Prasarn ML, Ouellette EA, Livingstone A, Giuffrida AY. Acute pediatric upper extremity compartment syndrome in the absence of fracture. J Pediatr Orthop. 2009;29(3):263-268.
doi pubmed - Malik SS, Uppal H, Sinha A, Malik SS, Katam K, Srinivasan K. Acute paediatric compartment syndrome of the hand caused by hereditary angiooedema. Ann R Coll Surg Engl. 2011;93(7):e138-140.
doi pubmed - Shaw NM, Kish A, Pensy R. Acute hematogenous osteomyelitis resulting in atraumatic pediatric forearm compartment syndrome. J Am Acad Orthop Surg Glob Res Rev. 2022;6(6):e21.00228.
doi pubmed - Torlincasi AM, Lopez RA, Waseem M. Acute compartment syndrome. In: StatPearls. Treasure Island (FL) ineligible companies. 2025.
pubmed - Warren M, Dhillon G, Muscat J, Abdulkarim A. Atraumatic bilateral acute compartment syndrome of the lower legs: a review of the literature. Cureus. 2021;13(12):e20256.
doi pubmed - Sees JA, Cutler GJ, Ortega HW. Risk factors for compartment syndrome in pediatric trauma patients. Pediatr Emerg Care. 2020;36(3):e115-e119.
doi pubmed - Grottkau BE, Epps HR, Di Scala C. Compartment syndrome in children and adolescents. J Pediatr Surg. 2005;40(4):678-682.
doi pubmed - Lin JS, Samora JB. Pediatric acute compartment syndrome: a systematic review and meta-analysis. J Pediatr Orthop B. 2020;29(1):90-96.
doi pubmed - Battaglia TC, Armstrong DG, Schwend RM. Factors affecting forearm compartment pressures in children with supracondylar fractures of the humerus. J Pediatr Orthop. 2002;22(4):431-439.
pubmed - Wu JP, Lu YT, Wei XX, Zou PX, Li YQ, Liu YZ, Canavese F, et al. Epidemiological characteristics and distribution of pediatric supracondylar fractures in South China: a retrospective analysis of 760 cases. J Pediatr Orthop B. 2024;33(2):136-141.
doi pubmed - Mortensen SJ, Orman S, Testa EJ, Mohamadi A, Nazarian A, von Keudell AG. Risk factors for developing acute compartment syndrome in the pediatric population: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2020;30(5):839-844.
doi pubmed - Blakemore LC, Cooperman DR, Thompson GH, Wathey C, Ballock RT. Compartment syndrome in ipsilateral humerus and forearm fractures in children. Clin Orthop Relat Res. 2000376):32-38.
doi pubmed - Matsen FA, 3rd, Krugmire RB, Jr. Compartmental syndromes. Surg Gynecol Obstet. 1978;147(6):943-949.
pubmed - Broom A, Schur MD, Arkader A, Flynn J, Gornitzky A, Choi PD. Compartment syndrome in infants and toddlers. J Child Orthop. 2016;10(5):453-460.
doi pubmed - Shadgan B, Pereira G, Menon M, Sanders D, Jafari S, Duffy T, O’Brien PJ. Current thinking about acute compartment syndrome of the leg. Can J Surg. 2008;51(6):358-363.
- Flynn JM, Bashyal RK, Yeger-McKeever M, Garner MR, Launay F, Sponseller PD. Acute traumatic compartment syndrome of the leg in children: diagnosis and outcome. J Bone Joint Surg Am. 2011;93(10):937-941.
doi pubmed - Baghdadi S. Pediatric floating elbow injuries are not as problematic as they were once thought to be: a systematic review. J Pediatr Orthop. 2020;40(8):380-386.
doi pubmed - Roposch A, Reis M, Molina M, Davids J, Stanley E, Wilkins K, Chambers HG. Supracondylar fractures of the humerus associated with ipsilateral forearm fractures in children: a report of forty-seven cases. J Pediatr Orthop. 2001;21(3):307-312.
pubmed
This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0), which permits unrestricted use, distribution, and reproduction in any medium, including commercial use, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.