| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 11, November 2025, pages 440-443
Reverse Venous Arterialization Simplified Technique: A Novel Method to Correct an Inadvertently Created Femoral Artery to Peroneal Vein Bypass
Catherine C. Laia, Aldin Malkocb, Raja Gnanadevb, Brianna-Marie Riub, So Un Kimb, Mehnaaz Mohammedb, Samuel Schwartzb, d, Omar Salehc
aCalifornia University of Science and Medicine School of Medicine, Colton, CA, USA
bDivision of Vascular Surgery, Department of Surgery, Arrowhead Regional Medical Center, Colton, CA 92324, USA
cChino Vascular and Surgery Center, Chino, CA 91710, USA
dCorresponding Author: Samuel Schwartz, Division of Vascular Surgery, Department of Surgery, Arrowhead Regional Medical Center, Colton, CA 92324, USA
Manuscript submitted August 12, 2025, accepted October 15, 2025, published online October 31, 2025
Short title: Reverse Venous Arterialization Technique
doi: https://doi.org/10.14740/jmc5188
| Abstract | ▴Top |
Chronic limb-threatening ischemia (CLTI) presents a significant management challenge. We describe the case of an 80-year-old female with CLTI and dry gangrene who underwent a common femoral artery (CFA)-to-posterior tibial artery (PTA) bypass that remained patent but was inadvertently anastomosed to the peroneal vein, resulting in venous arterialization. Postoperatively, her gangrene progressed and pain worsened, prompting an offer of below-knee amputation. Upon presentation for a second opinion, angiography confirmed the patent but malpositioned bypass. Given her extensive comorbidities, she was considered a poor candidate for open revision. We report successful percutaneous correction using the venous arterialization simplified technique (VAST), which re-established flow from the bypass graft back into the arterial lumen of the PTA using a double-gunsight approach. A 5 × 100 mm Viabahn stent graft was deployed to bridge the bypass and PTA, followed by angioplasty of the PTA and plantar artery, restoring in-line perfusion to the plantar arch and digital runoff. At 2-month follow-up, the patient demonstrated marked wound healing and avoided amputation. This case underscores the role of innovative endovascular rescue techniques in high-risk patients with preserved distal runoff and limited surgical options.
Keywords: Chronic limb-threatening ischemia; Venous arterialization simplified technique; Endovascular revision; Percutaneous revascularization; Limb salvage
| Introduction | ▴Top |
Chronic limb-threatening ischemia (CLTI) is the most advanced stage of peripheral arterial disease (PAD), characterized by ischemic rest pain, non-healing ulcers, or gangrene, and carries a high risk of major amputation and mortality [1]. Prompt and effective revascularization is critical to improve limb salvage rates and quality of life in affected patients [2]. Available techniques include open surgical bypass and percutaneous endovascular therapy. Bypass surgery offers the advantage of superior long-term patency and durability, particularly in patients with suitable conduit and target vessels. However, it may be associated with significant perioperative cardiac complications, graft failure, and wound morbidity, making patient selection and perioperative management crucial [3, 4].
Inadvertent anastomosis of a bypass graft to a vein is an extremely rare complication that can lead to rapid clinical deterioration due to venous hypertension and diversion of arterial flow away from the distal arterial network. Management is particularly challenging because these patients are often poor surgical candidates, and open revision is technically demanding. In such cases, the therapeutic goal shifts from traditional revascularization to redirecting arterial flow distally, thereby restoring effective perfusion. Percutaneous endovascular techniques can therefore offer an alternative, less invasive solution to high-risk individuals [5].
This case report describes an 80-year-old female patient with CLTI who underwent a bypass procedure for revascularization complicated by inadvertent anastomosis of the bypass graft to the peroneal vein with endovascular rescue. With worsening ischemia and limited surgical options, the patient was successfully treated with a novel percutaneous bypass revision using the venous arterialization simplified technique (VAST). This case highlights the importance of careful post-procedure assessment and the expanding role of innovative endovascular solutions in high-risk patients with limited options.
| Case Report | ▴Top |
An 80-year-old woman with significant medical comorbidities of coronary artery disease, hypertension, poorly controlled diabetes mellitus, hyperlipidemia, and an over 10 year, one-pack-per-day smoking history, presented to a vascular surgeon with CLTI and dry gangrene of the second toe, who underwent planned common femoral artery (CFA) to posterior tibial artery (PTA) bypass surgery for revascularization. Immediately after surgery, the patient’s pain increased. She developed additional gangrene of her third and fourth toes, a new wound on the dorsum of her foot, and a new wound at the anastomosis site of the bypass (Fig. 1). The patient was offered a below-knee amputation after 2 months, with worsening symptoms. The patient then presented for a second opinion. Angiography demonstrated that the graft was inadvertently anastomosed to the peroneal vein near the foot (Fig. 2). Two additional vascular surgeons both deemed the patient at too high a risk for bypass revision due to her comorbid medical conditions and lack of additional venous conduit. Due to the patient’s deteriorating condition and comorbidities, percutaneous revision of the bypass was offered.
 Click for large image | Figure 1. Right foot at initial presentation with new gangrene involving the third and fourth toes, a new wound on the dorsum of the foot. |
 Click for large image | Figure 2. Angiography of the lower leg and foot was performed prior to the revision. The peroneal vein was arterialized by the bypass graft, with diminished blood flow to the forefoot. |
A 7-Fr sheath was inserted antegrade into the CFA and a snare was inserted into the bypass graft. A 6-Fr pedal sheath was inserted retrograde into the distal posterior tibial artery to allow for stable device delivery and retrieval during tract creation. The vessel diameter was adequate to accommodate this size without compromise. Using the double-gunsight technique - a fluoroscopically guided method in which two snares are aligned to target a percutaneous puncture tract - a micropuncture needle was passed through both snares to establish through-and-through access. Distal angiography confirmed a patent plantar arch with in-line flow through the lateral plantar artery and digital branches. A Command 0.018-in wire was flossed through and snared from both ends, enabling angioplasty of the tract with a 4 mm balloon (Fig. 3). A 5 × 100-mm Viabahn stent graft was deployed to bridge the bypass graft to the PTA. A 4-mm balloon was inflated in the bypass portion. The tibial sheath was removed, and through antegrade access, a Command 0.014-in wire was placed into the lateral plantar artery, followed by angioplasty of the PTA with a 2.5-mm balloon and the plantar artery with a 2.0-mm balloon. Post-revision angiography revealed greatly improved blood flow into the arterial plantar arch (Fig. 4). The patient showed signs of healing. At two months post-revision, the patient had avoided amputation and no longer required medication for pain control.
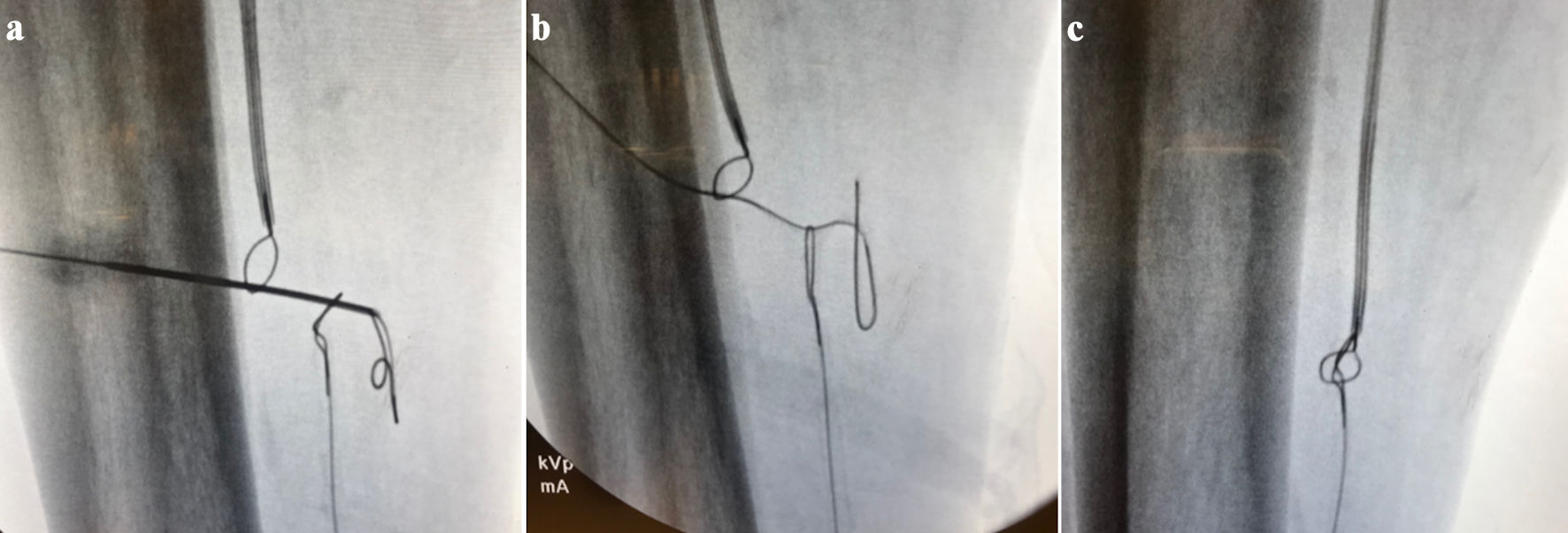 Click for large image | Figure 3. (a) Using double gunsight technique, a micropuncture needle was placed through the skin at the lower leg and through both snares. (b) Command 0.018-in floppy wire inserted in the micropuncture needle, and the needle removed. (c) Floppy wire snared from both ends establishing a tract. |
 Click for large image | Figure 4. Post-revision angiography showed improved blood flow to the arterial plantar arch. |
| Discussion | ▴Top |
This case demonstrates a rarely reported complication involving inadvertent anastomosis of a bypass graft to the peroneal vein during CFA-to-PTA bypass surgery. This led to increased pain, persistent ischemia, and progression of gangrene despite the patent bypass graft, as demonstrated by ultrasonography. These complications increase the risk of major limb loss.
The arterialized peroneal vein diverted the arterial blood flow away from the distal arterial system instead of restoring the flow to the foot. Venous arterialization can be an intentional and effective salvage technique in patients with no patent arterial plantar arch [6]. However, it can cause arterial steal and further clinical deterioration in patients with a functioning distal arterial network, as demonstrated in this patient. Although venous hypertension following venous arterialization can present in a transient phase during early remodeling, in this case the patient’s progressive ischemia, persistent pain, and worsening gangrene suggested true malperfusion rather than a benign transient response. The presence of a patent arterial plantar arch in this patient meant that venous diversion effectively stole blood from the forefoot, exacerbating ischemia and tissue loss. A patent and inline arterial plantar arch is a key predictor of limb salvage [7]. Thus, the best option for this patient was to revascularize the distal arterial target.
This case emphasizes the critical importance of additional imaging studies in the setting of unexpected postoperative deterioration. The patient’s immediate increase in pain and rapid progression of ischemic changes following surgery raises concerns of technical error or graft malfunction. Postoperative ultrasonography revealed that the bypass graft was patent. Angiography was performed, which revealed that the bypass graft was inadvertently anastomosed to the peroneal vein, allowing for an opportunity to intervene before major amputation. Timely imaging is essential not only for confirming patency, but also for identifying anatomical or technical issues that may not be evident intraoperatively.
The successful use of the VAST in this case underscores the importance of exploring minimally invasive and creative endovascular interventions in high-risk patients who are poor surgical candidates for open revision. VAST has been demonstrated as an effective technique for creating a fistula between an artery and a vein, arterializing the vein for patients with no-option CLTI for limb salvage [8]. In this case, reverse VAST was adapted to connect the bypass graft to an artery, the PTA, in order to restore in-line arterial flow to the plantar arch. This minimally invasive strategy stabilized the patient’s condition, enabled wound healing, and allowed the patient to avoid major amputations.
Learning points
This case demonstrates the critical role of technical innovation in the management of complex CLTI. The inadvertent venous anastomosis represents a rare but serious complication that, if unrecognized, may lead to rapid clinical deterioration and limb loss. Our successful salvage using the VAST not only averted major amputation but also facilitated substantial wound healing, reinforcing the potential of endovascular approaches in high-risk, surgically ineligible patients.
Acknowledgments
None to declare.
Financial Disclosure
The research presented in this manuscript received no specific funding from any agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that there is no conflict of interest.
Informed Consent
Informed consent was obtained for the use of deidentified information for publication in accordance with our Institutional Review Board policy.
Author Contributions
Catherine C. Lai, Aldin Malkoc, Raja Gnanadev, Brianna-Marie Riu, So Un Kim, Mehnaaz Mohammed, Samuel Schwartz, Omar Saleh: Conceptualization, methodology, writing-original draft, writing-review and editing. All authors read and approved the final manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available in this article.
Abbreviations
CLTI: chronic limb-threatening ischemia; CFA: common femoral artery; PTA: posterior tibial artery; VAST: venous arterialization simplified technique; PAD: peripheral arterial disease
| References | ▴Top |
- Abu Dabrh AM, Steffen MW, Undavalli C, Asi N, Wang Z, Elamin MB, Conte MS, et al. The natural history of untreated severe or critical limb ischemia. J Vasc Surg. 2015;62(6):1642-1651.e3.
doi pubmed - Menard MT, Farber A, Doros G, McGinigle KL, Chisci E, Clavijo LC, Kayssi A, et al. The impact of revascularization strategy on clinical failure, hemodynamic failure, and chronic limb-threatening ischemia symptoms in the BEST-CLI Trial. J Vasc Surg. 2024;80(6):1755-1765.e4.
doi pubmed - Siracuse JJ, Menard MT, Rosenfield K, Conte MS, Powell R, Hamburg N, Doros G, et al. Characterization of cardiovascular serious adverse events after bypass or endovascular revascularization for limb-threatening ischemia in the BEST-CLI trial. J Vasc Surg. 2024;80(3):774-779.
doi pubmed - Miah MMR, Avabde D, Ghahramani I, Hemanth R, Abbas R, Maha Q, Beech A, et al. Graft failure after revascularization for chronic limb-threatening ischaemia (CLTI) patients: the role of graft surveillance. Cureus. 2024;16(1):e53036.
doi pubmed - Abouzid MR, Vyas A, Kamel I, Anwar J, Elshafei S, Subramaniam V, Bennett W, et al. Comparing the efficacy and safety of endovascular therapy versus surgical revascularization for critical limb-threatening ischemia: A systematic review and Meta-analysis. Prog Cardiovasc Dis. 2025;88:126-135.
doi pubmed - Schmidt A, Schreve MA, Huizing E, Del Giudice C, Branzan D, Unlu C, Varcoe RL, et al. Midterm outcomes of percutaneous deep venous arterialization with a dedicated system for patients with no-option chronic limb-threatening ischemia: the ALPS multicenter study. J Endovasc Ther. 2020;27(4):658-665.
doi pubmed - Lundell A, Bergqvist D, Cederholm C. Patency of the plantar arch as a prognostic indicator in patients with critical leg ischaemia; a retrospective study. Eur J Surg. 1993;159(11-12):625-629.
pubmed - Ysa A, Lobato M, Mikelarena E, Arruabarrena A, Gomez R, Apodaka A, Metcalfe M, et al. Homemade device to facilitate percutaneous venous arterialization in patients with no-option critical limb ischemia. J Endovasc Ther. 2019;26(2):213-218.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.