| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 8, August 2025, pages 318-322
Transcatheter Arterialization of the Deep Veins for Chronic Limb-Threatening Ischemia: A Case Series of the Direct Cost Associated With Limb Salvage
Aldin Malkoca, c, Xinfei Miaob, Lana Mamounb, Catherine Laib, Raja GnanaDeva, Michelle Leea, Samuel Leea, b, Samuel Schwartza, b
aDepartment of Surgery, Arrowhead Regional Medical Center, Colton, CA 92324, USA
bCalifornia University of Science and Medicine, Colton, CA 92324, USA
cCorresponding Author: Aldin Malkoc, Department of Surgery, Arrowhead Regional Medical Center, Colton, CA 92324, USA
Manuscript submitted June 22, 2025, accepted July 30, 2025, published online August 22, 2025
Short title: Transcatheter Arterialization for CLTI
doi: https://doi.org/10.14740/jmc5155
| Abstract | ▴Top |
Our study aims to estimate the long-term cost of procedurally successful transcatheter arterialization of the deep veins (TADV) coupled with adjunct therapy. Patients with no conventional endovascular/open options were considered for TADV. TADV index procedure cost, cost of subsequent procedures and wound care/adjuncts were collected. Cost data were obtained from Medicare claims and other published sources. All patients in the study had limb salvage 180 days after TADV. Success was defined as lime salvage with no more than a transmetatarsal amputation of the affected limb. The average cost of the procedure was $320,850. The average hospital cost (hospitalization and wound care adjuncts) was $895,546. The overall average total cost was $1,216,396. TADV and associated multidisciplinary wound care approach for “no option” chronic limb-threatening ischemia does not appear to be a cost-effective strategy, with an average total cost of over 1 million dollars per patient.
Keywords: Transcatheter arterialization of the deep veins; Deep venous arterialization; Cost; Medicare; Amputation; Limb salvage
| Introduction | ▴Top |
Chronic limb-threatening ischemia (CLTI) is an advanced stage of peripheral arterial disease (PAD), marked by pain at rest, nonhealing ulcers, and gangrene due to a lack of blood flow to the tissue. PAD affects 8.5 million individuals aged ≥ 40, with CLTI being 11.08% annual [1, 2]. The goals of treatment for CLTI include revascularization to reduce ischemic pain, promote wound healing, and preserve a functional limb. Without treatment, CLTI leads to a 1-year all-cause mortality rate of 22% and a major amputation rate of 22% [3]. Several revascularization options include open, endovascular, and hybrid options. Treatment evaluation and selection, considering the location and extent of vascular disease, is driven by shared decision making between interdisciplinary and the patient.
Up to 20% of patients with CLTI are classified as “no option” patients because of the presence of severe tibial and pedal disease that does not permit bypass or other less invasive endovascular and hybrid options [4]. For this group of patients, superficial venous arterialization (SVA) and deep venous arterialization (DVA) have been shown to improve blood flow and increase limb salvage rates. Both SVA and DVA involve creating a connection between a proximal arterial inflow and the distal venous outflow. Disrupting valves allows oxygenated blood to flow through the vein, supplying tissue perfusion to the distal extremities [4, 5]. Importantly, improvement in distal perfusion following DVA may take several weeks, as the arterialized venous network requires time to mature. Venous arterialization can be performed with an open, percutaneous, or hybrid approach using various conduit, inflow, and outflow vessels. Patients with no option anatomy for CLTI generally require multiple procedures and extensive hospital stays, and have a high hospital readmission rate, which leads to a great financial burden. More studies are needed to determine the cost-effectiveness of DVA. It is estimated that approximately $12 billion in annual costs is attributable to cases of CLTI in the United States [6]. Our study estimates the long-term cost of successful DVA coupled with adjunct therapies in a quaternary vascular center.
| Case Report | ▴Top |
A retrospective observational case-control review of all patients with CLTI who presented directly to a level-1 trauma center was performed. The facility is a level-1 trauma center and a teaching hospital that sees more than 120,000 patients in the emergency department (ED) annually. All patients who were candidates for DVA were assessed. Patients with successful venous arterialization (limb salvage and complete wound healing) were included. Cost data were obtained through hospital billing using Medicare MedPAR dataset for each inpatient service. These figures represent institutional charges and do not include professional fees from physicians or follow-up outpatient costs. During the study period, five patients underwent attempted DVA. Three patients achieved successful limb salvage and are included in this series.
The general approach used for transcatheter arterialization of the deep venous system at our institution is as follows: 6-French sheath is placed antegrade from the ipsilateral common femoral artery. The sheath is advanced to the popliteal artery (P3). If needed pre-treatment with plain balloon angioplasty is performed on the tibial peroneal trunk to allow advancement of the Pioneer Plus system. A Pioneer Plus re-entry catheter is used to cross from the posterior tibial artery (PTA) to the posterior tibial vein (PTV) using a 0.014" command wire. Over a Spartacore wire (0.014"), balloon angioplasty of the artery and valvuloplasty of the vein is then performed using a 2.5- and 4-mm balloon. This then allows delivery of two overlapping Viabahn stents (5 × 250 mm, 5 × 2.5 mm) from the crossing point of the posterior tibial artery down to the level of the distal ankle. The proximal stent is post-dilated to 5 mm and the distal stent is post-dilated to 4 mm. Additional follow-up angiography is performed about 2 weeks later to assess maturation of the arterialized venous network in the foot. Further debridement and digital amputation are delayed until at least 6 - 12 weeks after the index procedure. The LimFlow system was not available at our institution during the study period. Therefore, all cases used Viabahn stents for venous arterialization.
Three patients were identified as having CLTI requiring DVA within the last 5 years. The average length of hospital stay for these three patients was 135 days. The average procedure cost, including that of endovascular and operative procedures, was $320,850. The average hospital cost for all initial and repeat hospitalizations was $895,546. Table 1 shows the overall average total cost of the four procedures and hospital length of stay (LOS) was $1,215,396. Table 2 breaks down per patient the total cost for procedures and hospital LOS including the overall cost per patient. The range of total procedures and hospital LOS cost was $861,079.20-$1,772,663.00. Table 3 considers the individual procedures that were included in the initial and repeat procedures and their associated costs. This is the generalized procedure that a patient would have. Lower extremity DVA was $44,755.00. The venogram and angiogram costs are $5,126 and $8,256, respectively. The remaining costs are listed in Table 3.
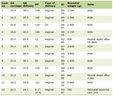 Click to view | Table 1. Average Hospital LOS, Cost, and Total Costs for the Three Patients |
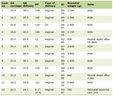 Click to view | Table 2. Breakdown of Each Patient’s Costs for Procedures and Hospital Stay |
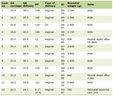 Click to view | Table 3. Estimated Costs of Revascularization Procedures and Associated Treatments |
| Discussion | ▴Top |
PAD affects millions of adults and increases the risk of heart attack, stroke, and limb-threatening ischemia. Multilevel atherosclerotic disease results in chronic limb-threatening ischemia, and patients experience rest pain, non-healing ulcers, and reduced quality of life [7, 8]. Patients with CLTI are possible candidates for multiple complex endovascular interventions including: atherectomy, angioplasty, drug-eluting stents, and balloons; however, they are often treated with life-altering amputations [9, 10]. “No-option” patients have an increased risk of amputation, which ultimately results in increased mortality, prolonged hospital stay, additional healthcare costs, and reduced quality of life [7-11]. DVA is an alternative surgical approach to amputation for patients with “no-option” CLTI by using the venous system in an arteriovenous fistula to reperfuse the extremity [12]. DVA has the potential to reduce the morbidity and mortality rates of CLTI [13].
The current literature shows varying degrees of successful clinical outcomes following DVA. In a follow-up study of CLTI patients, percutaneous DVA had a technical success rate of 88%, but amputation rates of 22%, 55.6%, and 49.4% at 1, 6, and 12 months postoperatively, respectively [14]. Multiple studies have shown high technical success rates but decreasing rates of amputation-free survival within the postoperative period [13-17]. DVA success is not yet consistent and frequently depends on repeat interventions. A systematic review of 233 patients with DVA had a median follow-up time of 12 months and showed a 21.8% amputation rate, a 97% technical success rate, a 13.8% complication rate, and a 37.4% reintervention rate [18]. Schmidt et al found DVA circuit obstruction in 65% of patients with CLTI within 3 months of surgery and required surgical reintervention. However, the DVA outcomes may be highly dependent on the surgical technique used. In a systematic review comparing open, percutaneous, and hybrid DVA strategies, limb salvage rates varied tremendously, ranging from 60% to 71% for percutaneous and 25% to 100% for open procedures [13]. Similarly, a study on over 400 CLTI patients with DVA showed a 3.7% mortality rate, a 15.5% morbidity rate, and a 79% limb-salvage rate within 1 month [19]. The lack of consistently high amputation-free survival rates beyond the 1-year post-op suggests that DVA is not a perfect solution, as it delays eventual limb loss, and imposes additional costs on the patient and hospital LOS, and overall risks a worsened quality of life.
Our results show that the overall cost of DVA is approximately $44,000 and with additional procedures and common interventions the cost increases tremendously. Totaling the procedures prior to DVA, the DVA, and re-interventions, it costs our patients over $300,000. Additionally, reinterventions result in an increased hospital LOS and a greater financial burden on the patient. When we included the prolonged LOS, the varying costs in placement, such as telemetry, medical-surgical unit care, and intensive care unit (ICU) stays, the CTLI management course cost our three patients $861,079, $1,772,663, and $1,015,448.40, respectively.
In this study, we described three patients undergoing long-term DVA limb salvage with an average total cost of over 1 million dollars per patient. This demonstrates that DVA is not a cost-effective treatment due to prolonged hospital stays and repeated re-intervention such as wound debridement. The lack of use of LimFlow devices at our center may contribute to the increased cost compared with the cost reported in a study conducted by Pietzsch et al, where percutaneous DVA with the LimFlow system was found to be cost-effective [20].
In comparison to limb salvage, lower limb amputation serves as the definitive treatment for non-reconstructible CLTI and may provide benefits of better pain control, wound healing, and shorter hospital stays [12]. Young patients with fewer comorbidities are expected to have functional outcomes comparable to those of patients who have successfully received revascularization [21]. In contrast, lower-limb amputation remains a risk factor for perioperative and long-term mortality [22]. In addition to mortality, Reed et al reported that most amputees in their study were willing to undergo everything possible to salvage the leg even if major amputation was the eventual result [23], while some patients in Columbo et al’s study preferred early amputation in their clinical course [24]. The total costs for primary below the knee amputation were upwards of $185,955 USD. Comparatively to limb salvage, these costs are lower [25]. The exact effectiveness of complex limb salvage using DVA remains unclear when considering psychosocial and functional outcomes. These factors need to be further investigated.
This study has several limitations. First, due to the retrospective nature of the chart review, there may have been inaccurate or incomplete documentation by medical professionals that may not capture all the measures necessary for cost analysis. Limb salvage cost can also be multifactorial and affected by comorbidities that patients might have. This may create uncertainty when calculating the total cost of limb salvage using DVA. Second, as a case series, our study did not include a comparative group. All three cases were from a single quaternary vascular center. It should be noted that our series only includes patients with successful limb salvage following DVA. Two additional patients underwent the procedure during the study period but progressed to major amputation and were removed the cost analysis. It is difficult to compare DVA cases conducted under other settings and available resources, and to provide generalizability to a larger population. Therefore, future studies should focus on multicenter investigations to better understand and identify the benefits and disadvantages of DVA limb salvage.
Learning points
DVA offers a potential limb salvage option for “no-option” CLTI patients, but multiple operations and extended hospitalizations are often required for its success. This case series emphasized the significant cost per person, mainly driven by reoperation and prolonged hospital stay. While we acknowledge the growing literature supporting DVA’s clinical and economic utility in selected settings, our goal is to contribute real-world cost data from a public hospital context and emphasize the importance of multidisciplinary decision-making. These findings highlight the need for further evaluation in its cost-effectiveness and long-term surgical and psychological outcomes of patients in comparison to primary amputation.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was not obtained due to the retrospective nature of this study. A review exemption for research was obtained from the local institutional review board (IRB) prior to initiating study procedures (IRB approval #24-01).
Author Contributions
Aldin Malkoc, Xinfei Miao, Lana Mamoun, Catherine Lai, Raja GnanaDev, Michelle Lee, Samuel Lee, and Samuel Schwartz: conceptualization, methodology, and writing - original draft. Aldin Malkoc, Xinfei Miao, Lana Mamoun, and Samuel Schwartz: writing - review and editing.
Data Availability
The authors declare that data supporting the findings of this study are available in the article.
Abbreviations
DVA: deep venous arterialization; PAD: peripheral arterial disease; SVA: superficial venous arterialization
| References | ▴Top |
- Allison MA, Ho E, Denenberg JO, Langer RD, Newman AB, Fabsitz RR, Criqui MH. Ethnic-specific prevalence of peripheral arterial disease in the United States. Am J Prev Med. 2007;32(4):328-333.
doi pubmed - Nehler MR, Duval S, Diao L, Annex BH, Hiatt WR, Rogers K, Zakharyan A, et al. Epidemiology of peripheral arterial disease and critical limb ischemia in an insured national population. J Vasc Surg. 2014;60(3):686-695.e682.
doi pubmed - Abu Dabrh AM, Steffen MW, Undavalli C, Asi N, Wang Z, Elamin MB, Conte MS, et al. The natural history of untreated severe or critical limb ischemia. J Vasc Surg. 2015;62(6):1642-1651.e1643.
doi pubmed - Ilyas S, Powell RJ. Management of the no-option foot: Deep vein arterialization. Semin Vasc Surg. 2022;35(2):210-218.
doi pubmed - Hardman RL, Jazaeri O, Yi J, Smith M, Gupta R. Overview of classification systems in peripheral artery disease. Semin Intervent Radiol. 2014;31(4):378-388.
doi pubmed - Mustapha JA, Katzen BT, Neville RF, Lookstein RA, Zeller T, Miller LE, Jaff MR. Determinants of long-term outcomes and costs in the management of critical limb ischemia: a population-based cohort study. J Am Heart Assoc. 2018;7(16):e009724.
doi pubmed - Lawall H, Zemmrich C, Bramlage P, Amann B. Health related quality of life in patients with critical limb ischemia. Vasa. 2012;41(2):78-88.
doi pubmed - Monaro S, West S, Gullick J. An integrative review of health-related quality of life in patients with critical limb ischaemia. J Clin Nurs. 2017;26(19-20):2826-2844.
doi pubmed - Hammad TA, Shishehbor MH. Advances in chronic limb-threatening ischemia. Vasc Med. 2021;26(2):126-130.
doi pubmed - Luders F, Bunzemeier H, Engelbertz C, Malyar NM, Meyborg M, Roeder N, Berger K, et al. CKD and acute and long-term outcome of patients with peripheral artery disease and critical limb ischemia. Clin J Am Soc Nephrol. 2016;11(2):216-222.
doi pubmed - Duff S, Mafilios MS, Bhounsule P, Hasegawa JT. The burden of critical limb ischemia: a review of recent literature. Vasc Health Risk Manag. 2019;15:187-208.
doi pubmed - Kim TI, Mena C, Sumpio BE. The role of lower extremity amputation in chronic limb-threatening ischemia. Int J Angiol. 2020;29(3):149-155.
doi pubmed - Ho VT, Gologorsky R, Kibrik P, Chandra V, Prent A, Lee J, Dua A. Open, percutaneous, and hybrid deep venous arterialization technique for no-option foot salvage. J Vasc Surg. 2020;71(6):2152-2160.
doi pubmed - Nakama T, Ichihashi S, Ogata K, Kojima S, Muraishi M, Obunai K, Watanabe H. Twelve-month clinical outcomes of percutaneous deep venous arterialization with alternative techniques and ordinary endovascular therapy devices for patients with chronic limb-threatening ischemia: results of the DEPARTURE Japan study. Cardiovasc Intervent Radiol. 2022;45(5):622-632.
doi pubmed - Schmidt A, Schreve MA, Huizing E, Del Giudice C, Branzan D, Unlu C, Varcoe RL, et al. Midterm outcomes of percutaneous deep venous arterialization with a dedicated system for patients with no-option chronic limb-threatening ischemia: the ALPS multicenter study. J Endovasc Ther. 2020;27(4):658-665.
doi pubmed - Kleiss SF, van Mierlo-van den Broek PAH, Vos CG, Fioole B, Bloemsma GC, de Vries-Werson DAB, Bokkers RPH, et al. Outcomes and patency of endovascular infrapopliteal reinterventions in patients with chronic limb-threatening ischemia. J Endovasc Ther. 2024;31(5):831-839.
doi pubmed - Kum S, Huizing E, Schreve MA, Unlu C, Ferraresi R, Samarakoon LB, van den Heuvel DA. Percutaneous deep venous arterialization in patients with critical limb ischemia. J Cardiovasc Surg (Torino). 2018;59(5):665-669.
doi pubmed - So SE, Chan YC, Cheng SW. Efficacy and durability of percutaneous deep vein arterialization: a systematic review. Ann Vasc Surg. 2024;105:89-98.
doi pubmed - Yan Q, Prasla S, Carlisle DC, Rajesh A, Treffalls J, Davies MG. Deep venous arterialization for chronic limb threatening ischemia in atherosclerosis patients - a meta-analysis. Ann Vasc Surg. 2022;81:1-21.
doi pubmed - Pietzsch JB, Ederhof M, Geisler BP, Schneider PA. Cost-effectiveness of percutaneous deep vein arterialization for patients with no-option chronic limb-threatening ischemia: an exploratory analysis based on the PROMISE I study. J Crit Limb Ischem. 2021;1:E148-E157.
- Taylor SM, Kalbaugh CA, Blackhurst DW, Hamontree SE, Cull DL, Messich HS, Robertson RT, et al. Preoperative clinical factors predict postoperative functional outcomes after major lower limb amputation: an analysis of 553 consecutive patients. J Vasc Surg. 2005;42(2):227-235.
doi pubmed - Klaphake S, de Leur K, Mulder PG, Ho GH, de Groot HG, Veen EJ, Verhagen HJ, et al. Mortality after major amputation in elderly patients with critical limb ischemia. Clin Interv Aging. 2017;12:1985-1992.
doi pubmed - Reed AB, Delvecchio C, Giglia JS. Major lower extremity amputation after multiple revascularizations: was it worth it? Ann Vasc Surg. 2008;22(3):335-340.
doi pubmed - Columbo JA, Davies L, Kang R, Barnes JA, Leinweber KA, Suckow BD, Goodney PP, et al. Patient experience of recovery after major leg amputation for arterial disease. Vasc Endovascular Surg. 2018;52(4):262-268.
doi pubmed - Barshes NR, Kougias P, Ozaki CK, Pisimisis G, Bechara CF, Henson HK, Belkin M. Cost-effectiveness of revascularization for limb preservation in patients with marginal functional status. Ann Vasc Surg. 2014;28(1):10-17.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.