| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 000, Number 000, October 2025, pages 000-000
Neonate With Malrotation Without Volvulus
Musab Al Shelalia, Leena Alwakeela, Khalid AlMahmouda, Lama Alfakhrib, c, Abdulrahman Alzahranic, d, e, Amal Yousifb
aPediatric Department, King Saud University Medical City, Riyadh, Saudi Arabia
bEmergency Department, Pediatric Unit, King Khalid University Hospital, King Saud University Medical City, Riyadh, Saudi Arabia
cSaudi Commission For Health Specialties (SCFHS), Riyadh, Saudi Arabia
dEmergency Department, Health Affairs, Ministry of National Guard, Riyadh, Saudi Arabia
eCorresponding Author: Abdulrahman Alzahrani, Emergency Administration, King Fahad Medical City, Second Health Cluster, Riyadh, Saudi Arabia
Manuscript submitted January 16, 2025, accepted September 23, 2025, published online October 10, 2025
Short title: Neonatal Malrotation Without Volvulus
doi: https://doi.org/10.14740/jmc5110
| Abstract | ▴Top |
Intestinal malrotation is a rare congenital anomaly that often presents as an acute surgical emergency in neonates, requiring prompt diagnosis and intervention to prevent life-threatening complications. We report the case of a 14-day-old male infant who presented with a 24-h history of bilious vomiting and bloody stools, accompanied by severe dehydration and laboratory findings suggestive of volvulus. Imaging studies confirmed intestinal malrotation, and the patient underwent an urgent open Ladd’s procedure, which revealed malrotation without volvulus. The patient successfully recovered with the resolution of symptoms and normalization of laboratory parameters. This case underscores the importance of early recognition, timely surgical management, and multidisciplinary care in ensuring favorable outcomes for neonates with intestinal malrotation.
Keywords: Neonate; Malrotation; Volvulus; Pediatric emergency
| Introduction | ▴Top |
Malrotation is a congenital anomaly resulting from abnormal or incomplete rotation of the midgut during fetal development. Though many cases remain clinically silent, malrotation carries a significant risk: complications such as ischemia, necrosis, and death have been documented when diagnosis is delayed. Its precise incidence of symptomatic cases is relatively low. Malrotation most commonly presents with volvulus (3.2% of cases), whereas isolated malrotation without volvulus is rare, occurring in only about 1.9% of cases [1-3].
The diagnosis of malrotation primarily relies on imaging modalities. The upper gastrointestinal (UGI) contrast study is considered the gold standard for defining abnormal duodenal anatomy and confirming malrotation [4]. Ultrasonography - including Doppler’s evaluation of the superior mesenteric artery and vein relationship, the “whirlpool sign”, or a transverse duodenum - has been shown in several studies to have high sensitivity and specificity and can act as an adjunct, especially where UGI contrast is delayed or inconclusive [5].
Here, we present the case of a 2-week-old male infant diagnosed with intestinal malrotation.
| Case Report | ▴Top |
A 14-day-old male neonate presented to the Pediatric Emergency Department with a 24-h history of poor feeding and bilious vomiting. The parents reported gross bloody stools and reduced urine output for 48 h but denied any fever or irritability.
The baby’s prenatal history was unremarkable, with a normal vaginal delivery at term and no complications or neonatal intensive care unit (NICU) admission.
On arrival, the neonate appeared lethargic with clinical signs of severe dehydration, including sunken eyes, poor skin turgor, cold extremities, and dry mucous membranes. Vital signs revealed tachycardia and tachypnea, with a blood pressure of 80/42 mm Hg, a rectal temperature of 37.5 °C, and oxygen saturation of 97%. Cardiovascular and respiratory examinations were unremarkable. Abdominal examination showed a soft but mildly distended abdomen, while genital examination revealed an uncircumcised male with both testicles in the scrotum and no scrotal swelling. Rectal examination identified fresh blood, and there was no evidence of lymphadenopathy, ulcers, or rashes.
Based on clinical history and examination findings, the patient was promptly resuscitated with three fluid boluses in the Emergency Department, and laboratory investigations were conducted. Empirical treatment with triple antibiotics (cefotaxime, metronidazole, and ampicillin) was initiated. A Foley catheter was inserted, yielding a small amount of dark, concentrated urine. A nasogastric tube was inserted as well, which drained greenish bilious fluid (Fig. 1).
 Click for large image | Figure 1. A nasogastric tube drained greenish bilious fluid. |
An abdominal X-ray demonstrated a single large bubble (Fig. 2), prompting an urgent surgical consultation. Laboratory results confirmed severe dehydration, with elevated creatinine and urea levels, coagulopathy characterized by a significantly elevated international normalized ratio (INR), and elevated lactate levels with a metabolic alkalosis on venous blood gas, all suggestive of hypoperfusion and systemic compromise.
 Click for large image | Figure 2. An abdominal X-ray demonstrated a single large bubble. |
After the patient’s condition stabilized, the surgery team conducted an UGI study (Fig. 3), which was suboptimal due to the unavailability of early oblique images to assess the duodenum and duodenojejunal junction orientation. Nevertheless, the study revealed dilatation of the stomach and duodenal “C” loop, with possible narrowing at the duodenum or pylorus and jejunal loops positioned on the right, suggestive of malrotation.
 Click for large image | Figure 3. An upper gastrointestinal (UGI) study revealed dilatation of the stomach and duodenal “C” loop, with possible narrowing at the duodenum or pylorus and jejunal loops positioned on the right, suggestive of malrotation. |
The patient was subsequently admitted to the NICU for further resuscitation and preparation for surgery. A central line was placed in the internal jugular vein, allowing the administration of factor VII and fresh frozen plasma (FFP) to lower the INR and correct his coagulopathy. A preoperative echocardiogram revealed a functional bicuspid aortic valve as an incidental finding, with no other abnormalities. Outpatient follow-up was advised after 6 months.
The patient underwent surgery after his condition had been optimized and stabilized. Intraoperatively, a midgut malrotation without volvulus was identified and the bowel was viable with no signs of necrosis (Fig. 4). The midgut detorsion had been performed counterclockwise for three rotations, Ladd bands were excised, and the mesentery was widened to prevent recurrence. The duodenum was straightened and mobilized, and an appendectomy was performed.
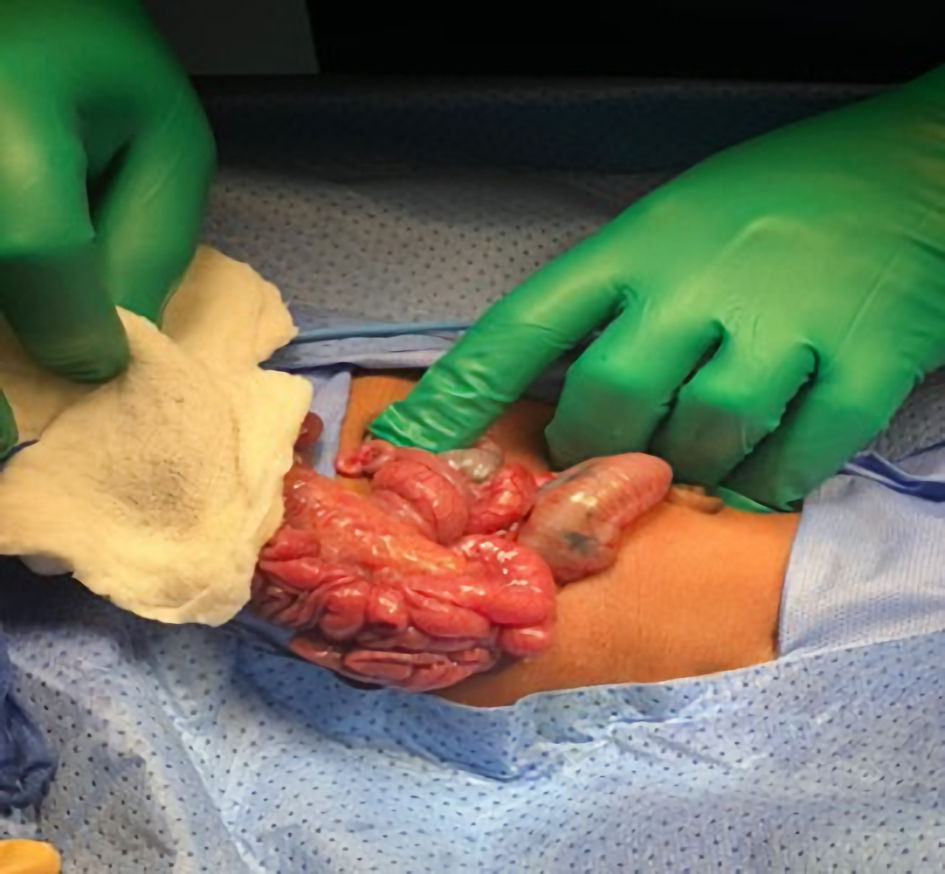 Click for large image | Figure 4. Intraoperatively, a midgut malrotation without volvulus was identified and the bowel was viable with no signs of necrosis. |
The patient was admitted to the NICU following surgery and extubated on the first postoperative day. Over a week, he transitioned from parenteral to enteral nutrition, with meconium passage occurring by postoperative day 4. Imaging confirmed the resolution of the intestinal obstruction. He was discharged on postoperative day 10 with normal bowel function and adequate feeding, and follow-up was arranged with pediatric surgery and high-risk neonatal clinics.
| Discussion | ▴Top |
This case illustrates an uncommon presentation of neonatal intestinal malrotation without volvulus. The infant presented with severe symptoms, including bilious vomiting, bloody stools, marked dehydration, and significant metabolic and coagulation abnormalities, strongly suggestive of midgut volvulus. However, intraoperative findings revealed isolated malrotation without volvulus, underscoring the diagnostic challenges when clinical and laboratory features mimic a more complicated pathology.
Malrotation is a congenital anomaly of the intestines that most commonly manifests during the neonatal period. It results from incomplete or improper rotation of the midgut during fetal development, which can lead to complications such as volvulus, intestinal obstruction, and bowel necrosis [6, 7]. Bilious vomiting and bloody stools are classic red flags and usually raise concern for malrotation with volvulus until proven otherwise [8]. In our patient, this presentation was compounded by severe dehydration, coagulopathy, and acute kidney injury, highlighting the potential severity of isolated malrotation. Similar findings have been described in literature where laboratory abnormalities reflect systemic compromise [9, 10].
The diagnostic approach typically begins with abdominal X-ray, followed by UGI contrast, which is the gold standard [8]. However, UGI can be inconclusive in up to 15% of cases, as occurred here, where the duodenojejunal junction was difficult to assess [11]. Ultrasound has emerged as a useful adjunct, particularly when UGI results are unclear, though its accuracy remains operator-dependent [11, 12].
Definitive management of malrotation is surgical, with the Ladd’s procedure remaining the standard of care [13]. Both open and laparoscopic approaches are effective, with comparable outcomes, though laparoscopy may require longer operating times [14]. In our case, an open approach was chosen to minimize operative duration given the patient’s unstable condition. Notably, despite severe presentation and metabolic derangements, surgery revealed malrotation without volvulus, emphasizing the importance of proceeding with intervention based on clinical suspicion rather than waiting for definitive imaging or intraoperative confirmation.
In conclusion, early recognition and intervention for malrotation, even without volvulus, in neonates with bilious vomiting and bloody stools, is crucial. While imaging is critical, inconclusive studies should not delay surgery when clinical suspicion is high. Prompt surgical management, guided by patient’s stability, remains key to favorable outcomes.
Learning points
Isolated malrotation can present with severe features that closely mimic volvulus.
Bilious vomiting and bloody stools in neonates should always trigger urgent evaluation for malrotation.
UGI contrast remains the gold standard for diagnosis, but inconclusive results require reliance on clinical judgment and, where available, adjunct ultrasound.
Ladd’s procedure is the definitive treatment; the choice of open versus laparoscopic approach should be guided by patient’s stability.
Maintaining high clinical suspicion is essential, as intraoperative findings may differ from initial expectations.
Acknowledgments
We would like to thank Dr. Husam Sakkijha, Chairman, Institutional Review Board (IRB), King Fahad Medical City, for his valuable guidance and support regarding the ethical instructions and review process.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from the patient’s parents for the publication of this case report, including any accompanying images.
Author Contributions
M. Al Shelali, L. Alwakeel and K. AlMahmoud wrote the manuscript. L. Alfakhri and A. Alzahrani reviewed the manuscript, with A. Alzahrani also overseeing logistics and publication. A. Yousif was the supervisor.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Eshel Fuhrer A, Doyev R, Koppelmann T, Shiran SI, Herzlich J, Mandel D, Sukhotnik I, et al. Upper gastrointestinal series in healthy neonates with bilious vomiting-is it still obvious? A retrospective observational study. Acta Paediatr. 2023;112(9):1870-1876.
doi pubmed - Srinivas S, Reddy KR, Balraj TA, Gangadhar A. Neonatal small bowel obstruction due to malrotation: a clinical study. Int Surg J. 2017;4(8):2727-2729.
doi - Bostanci SA, Oztorun CI, Erten EE, Akkaya F, Akbas I, Cayhan VS, Abay AN, et al. Clinical management of intestinal malrotation in different age groups. Pediatr Surg Int. 2024;40(1):204.
doi pubmed - Karaman I, Karaman A, Cinar HG, Erturk A, Erdogan D, Ozguner IF. Is color Doppler a reliable method for the diagnosis of malrotation? J Med Ultrason (2001). 2018;45(1):59-64.
doi pubmed - Zhou LY, Li SR, Wang W, Shan QY, Pan FS, Liu JC, Xie XY. Usefulness of sonography in evaluating children suspected of malrotation: comparison with an upper gastrointestinal contrast study. J Ultrasound Med. 2015;34(10):1825-1832.
doi pubmed - Menghwani H, Piplani R, Yhoshu E, Jagdish B, Sree BS. Delayed presentation of malrotation: case series and literature review. J Indian Assoc Pediatr Surg. 2023;28(4):271-277.
doi pubmed - Applegate KE, Anderson JM, Klatte EC. Intestinal malrotation in children: a problem-solving approach to the upper gastrointestinal series. Radiographics. 2006;26(5):1485-1500.
doi pubmed - Satrio K, Sari FP, Jonathan J, Putra Johansyah TK, Andhika Yogiswara MD, Darmajaya IM. Neonatal intestinal malrotation: A diagnostic pitfall. Neurol Spinal Med Chir. 2022;5:115-117.
- VanVooren DM, Bradshaw WT, Blake SM. Disseminated intravascular coagulation in the neonate. Neonatal Netw. 2018;37(4):205-211.
doi pubmed - Nwokoro CC, Emmanuel EA, Olatunji AA, Salami BA, Amosu LO, Ogundele IO. Malrotation of the midgut associated with horseshoe kidney presenting as gastric outlet obstruction in a 15-year-old boy. Afr J Paediatr Surg. 2020;17(3 & 4):122-126.
doi pubmed - Low YX, Teo YM, Lee YY, Nyo YL, Loh DL, Mali VP. Navigating inconclusive upper-gastrointestinal series in infantile bilious vomiting: a case series on intestinal malrotation. Am J Case Rep. 2024;25:e943056.
doi pubmed - Fukuhara M, Yamaguchi Y, Izaki T. Intestinal reversed rotation in neonates: A case report and review of the literature. Journal of Pediatric Surgery Case Reports. 2023;97:102708.
doi - Yang X, Wang W, Wang K, Zhao J, Sun L, Jiang S, Wang Y, et al. Identification and treatment of intestinal malrotation with midgut volvulus in childhood: a multicenter retrospective study. Front Pediatr. 2024;12:1390856.
doi pubmed - Xie W, Li Z, Wang Q, Wang L, Pan Y, Lu C. Laparoscopic vs open Ladd's procedure for malrotation in neonates and infants: a propensity score matching analysis. BMC Surg. 2022;22(1):25.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.