| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 2, February 2025, pages 43-47
Dual Tunneled Epidural Wound Catheters for Postoperative Analgesia Following Posterior Spinal Fusion
Grant Heydingera, b, e, Allen Kadadoc, Amr Elhamrawyd, Edison Villalobosa, Joseph D. Tobiasa, b, Giorgio Venezianoa, b
aDepartment of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA
bDepartment of Anesthesiology & Pain Medicine, The Ohio State University College of Medicine, Columbus, OH, USA
cDepartment of Orthopedic Surgery, Nationwide Children’s Hospital, Columbus, OH, USA
dDepartment of Anesthesiology, Wayne State University School of Medicine, Detroit, MI, USA
eCorresponding Author: Grant Heydinger, Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH 43205, USA
Manuscript submitted September 11, 2024, accepted November 30, 2024, published online December 31, 2024
Short title: Epidural Analgesia and Spine Surgery
doi: https://doi.org/10.14740/jmc4337
| Abstract | ▴Top |
Pain management following posterior spinal fusion (PSF) in pediatric patients can present significant challenges for clinicians. Opioids continue as the primary modality for managing postoperative pain in these patients, despite well-known concerns regarding their adverse effect profile such as the risk of dependence or abuse. Therefore, there has been increased focus on multimodal analgesic approaches that incorporate non-opioid medications, non-pharmacologic techniques, and regional anesthesia. Commonly used non-opioid adjuncts include non-steroidal anti-inflammatory drugs, acetaminophen, gabapentin, ketamine, and intravenous lidocaine. Because of ongoing controversy and insufficient evidence regarding different analgesic strategies, no definitive optimum regimen has been established. We present a 14-year-old adolescent female patient with neuromuscular scoliosis scheduled for PSF. The anesthetic plan involved a unique combination of total intravenous anesthesia (TIVA) and the placement of dual epidural catheters by the orthopedic surgeon for postoperative analgesia. The basic tenets of perioperative pain management for PSF are presented, perioperative concerns are discussed, and previous reports of regional anesthesia as an adjunct to general anesthesia in pediatric patients with scoliosis are reviewed.
Keywords: Epidural anesthesia; Postoperative pain; Regional anesthesia; Spine surgery; Scoliosis
| Introduction | ▴Top |
Pain management following posterior spinal fusion (PSF) can be challenging for anesthesiologists and pain management clinicians. This difficulty is in part due to the extensive nature of the surgery and the presence of multiple sources of pain including nociceptive, inflammatory, and neuropathic etiologies. Skin, subcutaneous tissue, muscles, ligaments, vertebrae, and fascia are all considered sources of postoperative pain. Moreover, many scoliosis patients may have chronic pain, which can result in the alteration of pain perception. PSF accounts for more than 90% of surgical procedures performed for the correction of scoliosis. Inadequate pain management results in significant morbidities such as delayed postoperative recovery, ambulation, discharge, and even persistent postoperative pain. Despite a large body of literature focused on improving postoperative outcomes following pediatric PSF surgery, there remains a significant need for better analgesic options. With an ever-increasing emphasis on multimodal, opioid-sparing techniques, regional anesthesia is being relied upon more than ever in both the adult and pediatric population [1, 2].
We describe perioperative pain management regimen using dual epidural wound catheters for a 14-year-old adolescent, who underwent PSF. The basics of the perioperative pain management of PSF are presented, perioperative concerns are discussed, and previous reports of the use of regional anesthesia as an adjunct to general anesthesia in pediatric patients with scoliosis are reviewed.
| Case Report | ▴Top |
Investigations
A 14-year-old, 20 kg adolescent female patient with neuromuscular scoliosis was scheduled for PSF. Her past medical history included chromosome 13q32 deletion, epilepsy, autonomic instability, nephrolithiasis, tracheostomy, and gastrostomy tube (GT) dependence. Her mother reported that her daughter frequently experienced episodes of autonomic “storming” characterized by seizure-like activity, tachycardia, tachypnea, fevers, agitation, and increased tracheal secretions secondary to pain. The patient had a history of subglottic stenosis with tracheostomy dependence.
Diagnosis
Preoperative vital signs revealed temperature 36.7 °C (98.1 °F), pulse 88 beats/min, respiration 30 breaths/min, and oxygen saturation 100%. The patient had a tracheostomy in place, but cardiac and respiratory examinations were otherwise unremarkable. Preoperative laboratory evaluation including a complete blood count, electrolytes, and renal function was obtained. The hemoglobin was 9.2 g/dL with a hematocrit of 29%. Echocardiogram showed mildly impaired right ventricular relaxation with a small posterior pericardial effusion. The anesthetic plan was total intravenous anesthesia (TIVA) and regional anesthesia (dual epidural catheters placed intraoperatively by the orthopedic surgeon). We determined that this patient would benefit from epidural anesthesia in addition to our institution’s multimodal pharmacologic approach to postoperative analgesia following PSF due to her complicated pain history. Premedication included oral midazolam and aprepitant via the gastrostomy, administered preoperatively. She was held nil per os and transported to the operating room. Routine American Society of Anesthesiologists monitors were applied. Anesthesia was induced by the inhalational of incremental concentrations of sevoflurane in 100% O2. Peripheral intravenous (PIV) access was obtained with a 22-gauge catheter followed by the administration of IV fentanyl (25 µg) and a small dose of rocuronium (10 mg) to facilitate smooth endotracheal intubation. After removal of tracheostomy tube, the patient’s trachea was intubated orally with 6.0 mm cuffed endotracheal tube without difficulty. Additional IV access was obtained, and a left ulnar arterial line was inserted under ultrasound guidance. To facilitate intraoperative neurophysiologic monitoring (somatosensory and motor evoked potentials (MEPs)), maintenance anesthesia included sufentanil (0.1 - 0.3 µg/kg/h), remimazolam (5 - 10 µg/kg/min), and desflurane (0.5 minimum alveolar concentration (MAC)). Neuromuscular blockade reversal was not needed at this time due to satisfactory baseline MEPs. Tranexamic acid (loading dose 50 mg/kg and maintenance 5 mg/kg/h) was administered to decrease blood loss. Cefazolin (50 mg/kg) and gentamicin (5 mg/kg) were administered for prophylaxis against a surgical site infection. Multimodal intraoperative pain management included methadone (2 mg), acetaminophen (15 mg/kg), hydromorphone (0.4 mg in two divided doses), and fentanyl (75 µg in three divided doses). Additionally, dual epidural wound catheters were placed into the epidural space and surrounding vertebral space prior to closure of the incision. To ensure adequate coverage, two wound catheters were placed in the epidural space, essentially spanning the entire length of the surgical incision. Two 19-gauge wound catheters (InfiltraLong 600 wound catheters, Pajunk, Geisingen, Germany) were used, each with 60 fenestrations at the distal 150 mm of the catheter to provide an even spread of the local anesthetic solution along the epidural space (Fig. 1). The epidural space was accessed at the T10-11 interspace. One catheter was threaded in a cephalad direction and the second catheter was threaded caudally. Both catheters were tunneled to exit the skin a few centimeters to the right of the surgical incision (Fig. 2). A Tegaderm dressing with a chlorhexidine gel pad was placed over the site where the catheters exited the skin. The epidural solution included 0.2% ropivacaine with 0.4 µg/mL clonidine at a rate of 5 mL/h. A Y-connector was used to allow a single epidural infusion pump to deliver the solution equally to both catheters. Intraoperative fluids included Normosol®-R electrolyte solution (750 mL), albumin 5% (400 mL), cell saver autotransfusion (150 mL), and one unit of packed red blood cells (283 mL). There were no intraoperative anesthetic concerns or complications. The procedure lasted for 6 h. At the completion of the procedure, any possible residual neuromuscular blockade was reversed with sugammadex (100 mg) and the patient’s tracheostomy tube was replaced. The patient was transported to the post-anesthesia care unit and then admitted to the pediatric intensive care unit postoperatively. The postoperative course was unremarkable. In addition to the epidural infusion, the postoperative pain regimen included an IV, demand only hydromorphone caregiver-controlled analgesia (CCA) pump, scheduled IV acetaminophen (300 mg TID), IV ketorolac (10 mg BID) and IV diazepam as needed.
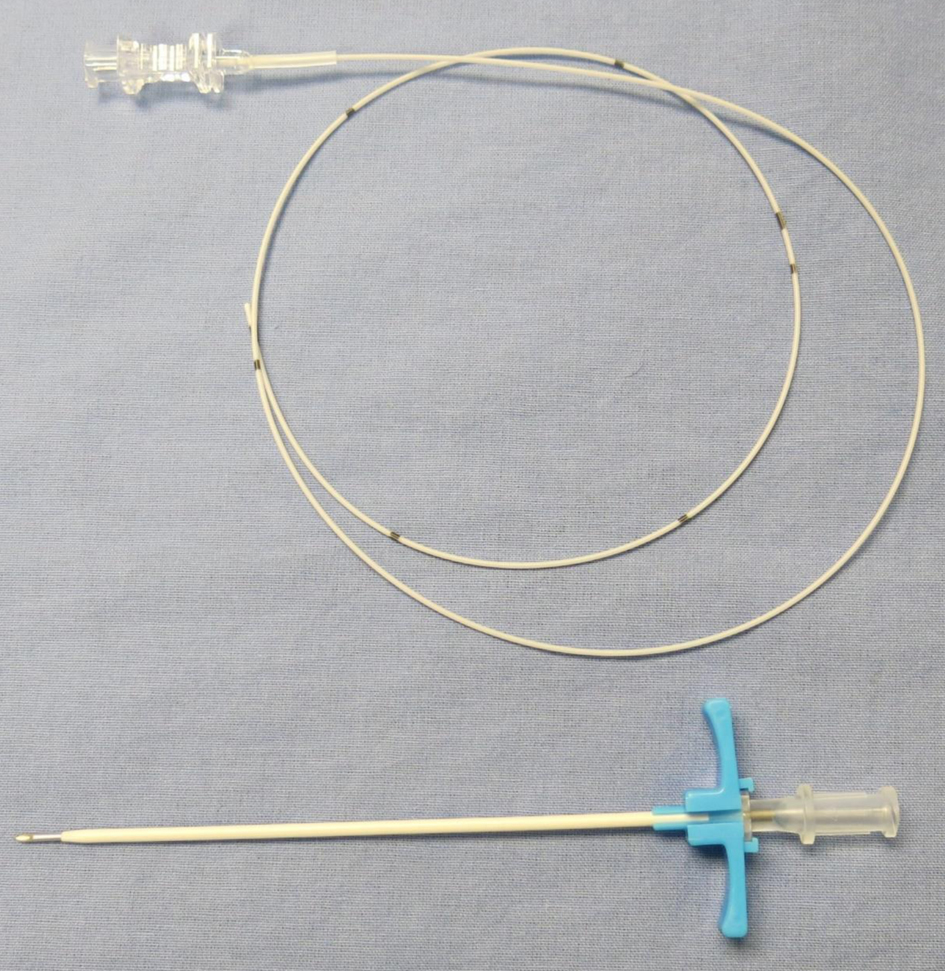 Click for large image | Figure 1. Photograph of a 19-gauge wound catheter with 60 fenestrations at the distal 150 mm of the catheter and break-away needle used for insertion/skin tunnelling. The fenestrations allow an even spread of the local anesthetic solution along the course of the catheter. |
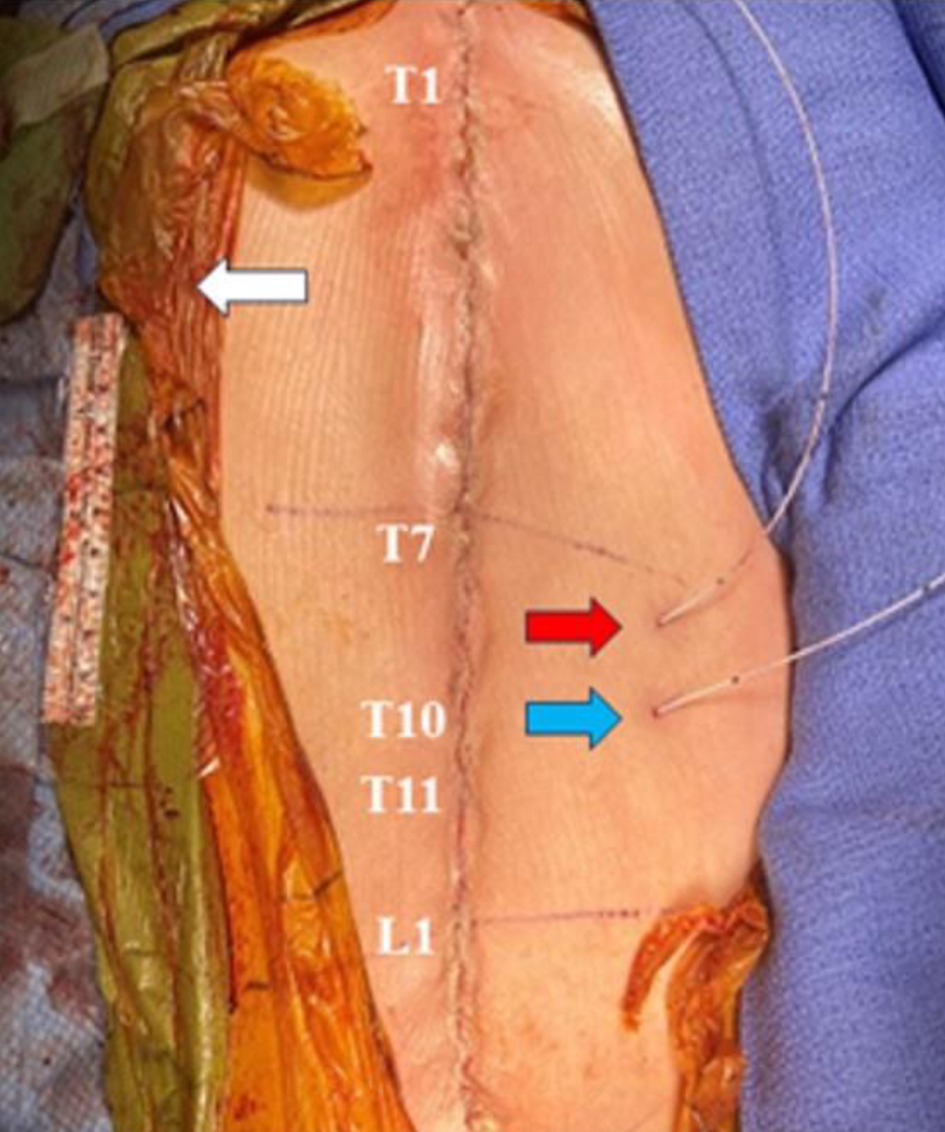 Click for large image | Figure 2. Postoperative photograph after wound closure. One catheter (red arrow) was threaded cephalad in the epidural space, while the second catheter (blue arrow) was threaded caudally. Both catheters exited the skin to the right of the surgical incision. The surgical site is surrounded by a transparent antimicrobial drape. Anatomic landmarks are labeled. |
Follow-up and outcomes
CCA usage was minimal for the first 5 postoperative days (POD) while the epidural catheters were in place (Table 1). The patient’s median Face, Legs, Activity, Cry, and Consolability (FLACC) scores were 0 every day postoperatively (Table 1). The maximum FLACC score was 5 on POD 1, but ≤ 2 on other days while the epidural catheters were in place. The patient experienced no episodes of autonomic storming following surgery. Both epidural catheters were removed without complications on POD 5 by the Acute Pain Service following a trial pause of the epidural infusion. Oxycodone was ordered to be given through the patient’s GT to mitigate potential increased pain following catheter removal, but this medication was discontinued in less than 2 days, and the patient’s pain remained well controlled. The CCA was only utilized twice following catheter removal, and no additional opioids were required during hospitalization. The patient was discharged home on POD 19 due to other comorbid conditions with prolonged postoperative course.
 Click to view | Table 1. Postoperative Pain Scores and Analgesic Requirements |
| Discussion | ▴Top |
Achieving optimum postoperative pain management following PSF can be challenging in both adult and pediatric patient populations. Minimizing exposure to opioids in the immediate/acute postoperative phase serves to decrease the overall risk of developing dependence or abuse. Recently, there has been significant interest in exploring multimodal opioid-sparing analgesic regimens, including regional anesthesia such as epidural and intrathecal (IT) anesthesia [3, 4]. There have been previous reports regarding the use of regional anesthetic techniques for postoperative analgesia following PSF. Feltz et al retrospectively reviewed experience with IT morphine in 105 patients with adolescent idiopathic scoliosis (AIS), who received PSF with instrumentation [5]. Patients were grouped into two cohorts including PSF with a standard surgical protocol (n = 40), while the second cohort received intraoperative IT morphine in addition to the standard surgical protocol (n = 65). The second group had a shorter length of stay (LOS) and had decreased postoperative analgesic requirements. However, the relatively shorter duration of IT analgesia is cited as a major limitation to its use with analgesia lasting ≤ 24 h [6]. Ibach et al reported that following IT morphine for PSF, the opioid requirements were higher during the 13 - 24 h period compared to the 0 - 12 h period (23.0 ± 12.5 mg vs. 15.9 ± 1.7 mg morphine). As the pain following PSF may persist through the second postoperative day, continuing for up to 1 week, other options may be needed.
To provide more long-term pain control, others have employed epidural anesthesia, erector spinae blockade, or dorsal ramus catheters [7-14]. When considering epidural anesthesia, given previous clinical experience, we have generally used a dual catheter technique to provide effective coverage of the entire length of the surgical excision which may span ≥ 10 - 12 dermatomes/vertebral levels. In our retrospective experience in 14 pediatric patients with dual epidural catheters placed and left in place for 5 days following PSF (11-14 levels fused), we noted low opioid requirements, consistently low pain scores, and no clinically significant adverse effects [8]. In 2005, Blumenthal et al found that a double epidural technique provided better postoperative analgesia, earlier recovery of bowel function, fewer adverse effects, and higher patient satisfaction when compared to IV morphine [11]. In contrast, a prospective, double-blinded, randomized trial found no difference in patient-controlled analgesia (PCA) use between epidural catheters containing bupivacaine versus normal saline placebo. However, limitations such as malpositioned epidural catheters, catheter migration from the epidural space, dilutional effect from bleeding at the surgical site, or loss of the local anesthetic solution due to surgical site drainage may impact analgesia. These studies emphasize that variations in the technique of catheter placement and subsequent use can influence analgesic efficacy.
Additional novel regional techniques to provide analgesia after spinal surgery have included erector spinae and dorsal ramus catheters [9, 10]. Almeida et al reported the use of bilateral T8 erector spinae catheters placed on POD 1 in an effort to control severe pain following lumbar spinal fusion (L2-S1) in a 79-year-old female patient. Despite receiving various analgesic agents including pethidine, tramadol, paracetamol, metamizole, and ketorolac, the patient experienced severe pain (10/10 on a numeric rating scale). Pain levels decreased to 1/10 immediately after administering a bolus dose of ropivacaine 0.2% (20 mL per side). The bolus dose was followed by a continuous infusion of ropivacaine 0.2% at 5 mL/h for 48 h. This was supplemented by two additional bolus doses of ropivacaine 0.2% (15 mL per side per day). Xu et al reported the use of dorsal ramus nerve blockade in a cohort of three pediatric patients following spinal surgery [10]. The bilateral multi-orifice infusion catheters were placed intraoperatively by the surgeon at the dorsal rami, lateral to the implanted pedicle screws. A continuous infusion of 0.2% ropivacaine was started postoperatively with the catheters left in place for 48 h. Pain scores and opioid consumption were low in the three patients. These reports suggest the potential benefits of adjunctive regional anesthesia techniques to provide analgesia following spinal surgery.
In addition to the techniques described above, the increasing use of liposomal bupivacaine (LB) for PSF surgery for surgical site infiltration has demonstrated promising results. In a retrospective analysis, Forrester et al found that among a cohort of 105 patients undergoing elective posterior cervical or lumbar surgery, 48 patients who received LB directly injected into the paraspinal muscles and subcutaneous tissue during wound closure had a decreased LOS compared to the control group (1.8 vs. 2.7 days) [15]. Additionally, these patients reported lower pain scores after surgery (5.2 vs. 6.4 at 24 h and 4.9 vs. 6.6 at 48 - 72 h), potentially facilitating early mobilization, improved patient reported outcomes, and increased engagement with therapy. Similarly, in a retrospective cohort study of 119 patients with AIS undergoing PSF, those who received an erector spinae block with LB in addition to the standard postoperative pain protocol had decreased total opioid use, shorter LOS, and improved ambulation [16].
Although epidural anesthesia has proven to be effective, it may alter the ability to assess postoperative motor function if motor blockade or sensory changes occur related to the epidural administration of local anesthetic agent. The presence of motor or sensory changes may be attributed to the epidural anesthesia and delay the diagnosis of more serious postoperative complications such as bleeding or hematoma formation. Therefore, low concentrations of local anesthetic, in combination with adjuncts like clonidine, should be used to enhance analgesia while minimizing sensory or motor changes. Dosing may be delayed until after the initial postoperative neurologic assessment is performed to document the baseline examination. Intraoperative dosing is not recommended as it will interfere with intraoperative neuromonitoring (IONM).
In an attempt to optimize the regimen in our patient, we chose to use two multi-orifice catheters, which allowed coverage of multiple surgical dermatomes/levels. Effective analgesia was achieved with low postoperative pain scores and limited opioid requirements. However, despite increasing experience, the efficacy of regional anesthetic techniques for pain control after PSF remains a subject of controversy. Variations in technique may impact analgesic efficacy and evaluation due to various factors, including the route of delivery (IT, epidural, erector spinae, dorsal ramus catheters), mode of delivery (single dose, intermittent bolus, or continuous infusion), number of catheters used (one vs. two), medications infused (opioids, local anesthetic agents, clonidine), choice of opioid (morphine, fentanyl, hydromorphone), and analgesic regimen.
Learning points
In conclusion, this case report describes effective postoperative analgesia following PSF using a novel technique involving dual, multi-orifice wound catheters placed directly into the epidural space. By using multi-orifice wound catheters, we were able to administer the local anesthetic directly to the entire span of the surgical incision. Although the patient was discharged home on POD 19 due to other comorbid conditions, the method provided effective analgesia with a median FLACC score of 0 until catheter removal on POD 5. The technique was simple to perform and free of adverse events. Our findings align with previous reports and warrant further prospective investigations to validate the safety and efficacy of this technique in pediatric patients undergoing PSF. Each anesthetic technique has its own advantages and limitations, highlighting the need for ongoing discussions to determine the most effective approach on a case-by-case basis.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Review of this case and presentation in this format followed the guidelines of the Institutional Review Board of Nationwide Children’s Hospital (Columbus, Ohio). Informed consent was obtained for use of de-identified information for publication.
Author Contributions
Patient care, case review and preparation of the manuscript including drafts and final version: GH AE, and EV; patient care and review of final manuscript: AK; intraoperative care of the patient and review of the final manuscript: GH; manuscript preparation, review, and editing: GV, JDT, and EV.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Seki H, Ideno S, Ishihara T, Watanabe K, Matsumoto M, Morisaki H. Postoperative pain management in patients undergoing posterior spinal fusion for adolescent idiopathic scoliosis: a narrative review. Scoliosis Spinal Disord. 2018;13:17.
doi pubmed pmc - Bajwa SJ, Haldar R. Pain management following spinal surgeries: an appraisal of the available options. J Craniovertebr Junction Spine. 2015;6(3):105-110.
doi pubmed pmc - Tobias JD. A review of intrathecal and epidural analgesia after spinal surgery in children. Anesth Analg. 2004;98(4):956-965.
doi pubmed - Daud K, Wariach S, Maqsood M, Sarraj M, Gaber K, Ewusie J, Khurshed A, et al. Effectiveness and safety of intrathecal morphine for pediatric patients undergoing scoliosis surgery: a systematic review and meta-analysis. Cureus. 2024;16(1):e51754.
doi pubmed pmc - Feltz KP, Hanson N, Jacobson NJ, Thompson PA, Haft GF. Intrathecal morphine use in adolescent idiopathic scoliosis surgery is associated with decreased opioid use and decreased length of stay. Iowa Orthop J. 2022;42(1):53-56.
pubmed pmc - Ibach BW, Loeber C, Shukry M, Hagemann TM, Harrison D, Johnson PN. Duration of intrathecal morphine effect in children with idiopathic scoliosis undergoing posterior spinal fusion. J Opioid Manag. 2015;11(4):295-303.
doi pubmed - O’Hara JF, Jr., Cywinski JB, Tetzlaff JE, Xu M, Gurd AR, Andrish JT. The effect of epidural vs intravenous analgesia for posterior spinal fusion surgery. Paediatr Anaesth. 2004;14(12):1009-1015.
doi pubmed - Tobias JD, Gaines RW, Lowry KJ, Kittle D, Bildner C. A dual epidural catheter technique to provide analgesia following posterior spinal fusion for scoliosis in children and adolescents. Paediatr Anaesth. 2001;11(2):199-203.
doi pubmed - Almeida CR, Oliveira AR, Cunha P. Continuous bilateral erector of spine plane block at T8 for extensive lumbar spine fusion surgery: case report. Pain Pract. 2019;19(5):536-540.
doi pubmed - Xu JL, Tseng V, Delbello D, Pravetz MA. Thoracolumbar dorsal ramus nerve block using continuous multiorifice infusion catheters: a novel technique for postoperative analgesia after scoliosis surgery. Int J Spine Surg. 2020;14(2):222-225.
doi pubmed pmc - Blumenthal S, Min K, Nadig M, Borgeat A. Double epidural catheter with ropivacaine versus intravenous morphine: a comparison for postoperative analgesia after scoliosis correction surgery. Anesthesiology. 2005;102(1):175-180.
doi pubmed - Turner A, Lee J, Mitchell R, Berman J, Edge G, Fennelly M. The efficacy of surgically placed epidural catheters for analgesia after posterior spinal surgery. Anaesthesia. 2000;55(4):370-373.
doi pubmed - Halpern LM, Velarde AR, Zhang DA, Bronson W, Kogan C. Continuous epidural analgesia (CEA) via single catheter providing profound analgesia for pediatric patients following posterior spinal fusion (PSF) in adolescent idiopathic scoliosis (AIS). Cureus. 2023;15(4):e37066.
doi pubmed pmc - Hong RA, Gibbons KM, Li GY, Holman A, Voepel-Lewis T. A retrospective comparison of intrathecal morphine and epidural hydromorphone for analgesia following posterior spinal fusion in adolescents with idiopathic scoliosis. Paediatr Anaesth. 2017;27(1):91-97.
doi pubmed - Forrester DA, Miner H, Shirazi C, Kavadi N. Liposomal bupivacaine in posterior spine surgery: a piece of the puzzle for postoperative pain. J Orthop. 2022;33:55-59.
doi pubmed pmc - Changoor S, Giakas A, Sacks K, Asma A, Lang RS, Yorgova P, Rogers K, et al. The role of liposomal bupivacaine in multimodal pain management following posterior spinal fusion for adolescent idiopathic scoliosis: faster and farther with less opioids. Spine (Phila Pa 1976). 2024;49(2):E11-E16.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.