| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com |
Case Report
Volume 16, Number 2, February 2025, pages 61-68
Partial Oculomotor Nerve Palsy as the First Presentation of Extranodal Natural Killer/T-Cell Lymphoma
Worapot Srimanana, b , Phawasutthi Keokajeea
aOphthalmology Division, Phramongkutklao Hospital, Thung Phayathai Subdistrict, Ratchathewi, Bangkok, Thailand
bCorresponding Author: Worapot Srimanan, Ophthalmology Division, Phramongkutklao Hospital, Thung Phayathai Subdistrict, Ratchathewi, Bangkok, Thailand
Manuscript submitted December 16, 2024, accepted January 16, 2025, published online January 25, 2025
Short title: Oculomotor Palsy in Extranodal NK/T-Cell Lymphoma
doi: https://doi.org/10.14740/jmc5092
| Abstract | ▴Top |
Extranodal natural killer/T-cell lymphoma (ENKTL) is a rare and aggressive subtype of non-Hodgkin lymphoma, typically involving the nasal cavity. However, it can occasionally present in extranodal sites without nasal involvement, complicating diagnosis. This report describes a 78-year-old man who presented with progressive double vision and visual loss in the right eye over 3 weeks. Examination revealed partial oculomotor nerve palsy with pupillary involvement and signs of optic neuropathy, leading to a diagnosis of orbital apex syndrome. The nasopharyngeal evaluation showed no nasal lesions. Magnetic resonance imaging (MRI) identified diffuse enhancement of the extraocular muscles, intraorbital soft tissues, and optic nerve sheath in the right orbit. A right medial rectus muscle biopsy confirmed extranodal NK/T-cell lymphoma through immunohistochemical analysis. Chemotherapy was initiated, significantly improving both ophthalmoplegia and visual acuity. This case underscores the importance of comprehensive neuro-ophthalmic evaluation and biopsy for diagnosing ENKTL, especially in atypical presentations without nasal involvement. Early detection and treatment are critical for achieving favorable outcomes in this rare disease.
Keywords: Orbital apex syndrome; Lymphoma; Ophthalmoplegia; Optic neuropathy; Visual loss; Diplopia
| Introduction | ▴Top |
Extranodal natural killer/T-cell lymphoma (ENKTL), nasal type, is a rare and aggressive lymphoma subtype most frequently associated with Epstein-Barr virus (EBV) infection [1, 2]. It typically originates in the nasal cavity or paranasal sinuses (PNS) [3], leading to destructive midline facial lesions. However, ENKTL occasionally manifests in extranodal sites without nasal pathology, posing significant diagnostic challenges due to its deviation from common clinical features. While most orbital lymphomas are non-Hodgkin B-cell lymphomas, such as mucosa-associated lymphoid tissue (MALT) lymphomas with a relatively good prognosis, T-cell and NK/T-cell lymphomas are extremely rare in this region [4, 5]. Orbital involvement usually occurs as a secondary extension of nasal ENKTL, but isolated primary orbital cases, though uncommon, have been reported [3-12].
ENKTL in the orbit is particularly aggressive and carries a poor prognosis due to its resistance to standard chemotherapy and radiotherapy. Unlike the more common low-grade B-cell malignancies typically seen in orbital lymphomas, NK/T-cell lymphomas exhibit rapid progression and high mortality rates [4, 5, 9-12]. Orbital involvement often presents as an extension from nasal lesions; however, in rare instances, the orbit may be the primary or sole site of disease manifestation. Such presentations challenge conventional diagnostic approaches, particularly when no overt nasal or anterior ocular abnormalities exist. This variability in presentation underscores the importance of maintaining a high index of suspicion in atypical cases.
Here, we present a case of primary orbital ENKTL manifesting solely as orbital apex syndrome (OAS) without nasal involvement. The patient exhibited isolated oculomotor nerve dysfunction and progressive optic neuropathy despite a normal ocular examination. This report highlights the challenges associated with diagnosing ENKTL in cases with subtle presentations and emphasizes the need for comprehensive multidisciplinary evaluation and advanced imaging to facilitate timely diagnosis and treatment.
The Institutional Review Board Royal Thai Army reviewed and approved this study protocol (approval number: S095h/67_Exp).
| Case Report | ▴Top |
Investigations
A 78-year-old man presented with a 3-week history of blurred vision. He had a medical history of well-controlled hypertension and cardiac arrhythmia. At his initial visit, his visual acuity was 20/100 in the right eye, improving to 20/40 with a pinhole, and 20/60 in the left eye, also improving to 20/40 with a pinhole. A diagnosis of mild cataracts in both eyes was made, and he was given a new glasses prescription. During a trial with the corrective lenses, he noticed a slight improvement in vision but experienced double vision. A second opinion was sought, and the examining ophthalmologist detected exotropia. His best-corrected visual acuity in both eyes was 20/40.
Anterior segment examination revealed nuclear sclerosis grade 2+ in both eyes, with pupils reacting to light at 3 mm. Ocular motility assessment showed a limitation in right eye movements: adduction was restricted to 80%, with mild limitations in upgaze and downgaze to 90% of the normal range. A diagnosis of partial oculomotor nerve palsy in the right eye, sparing the pupil, was made. After discussing with the patient, a follow-up was scheduled to monitor for possible pupillary involvement.
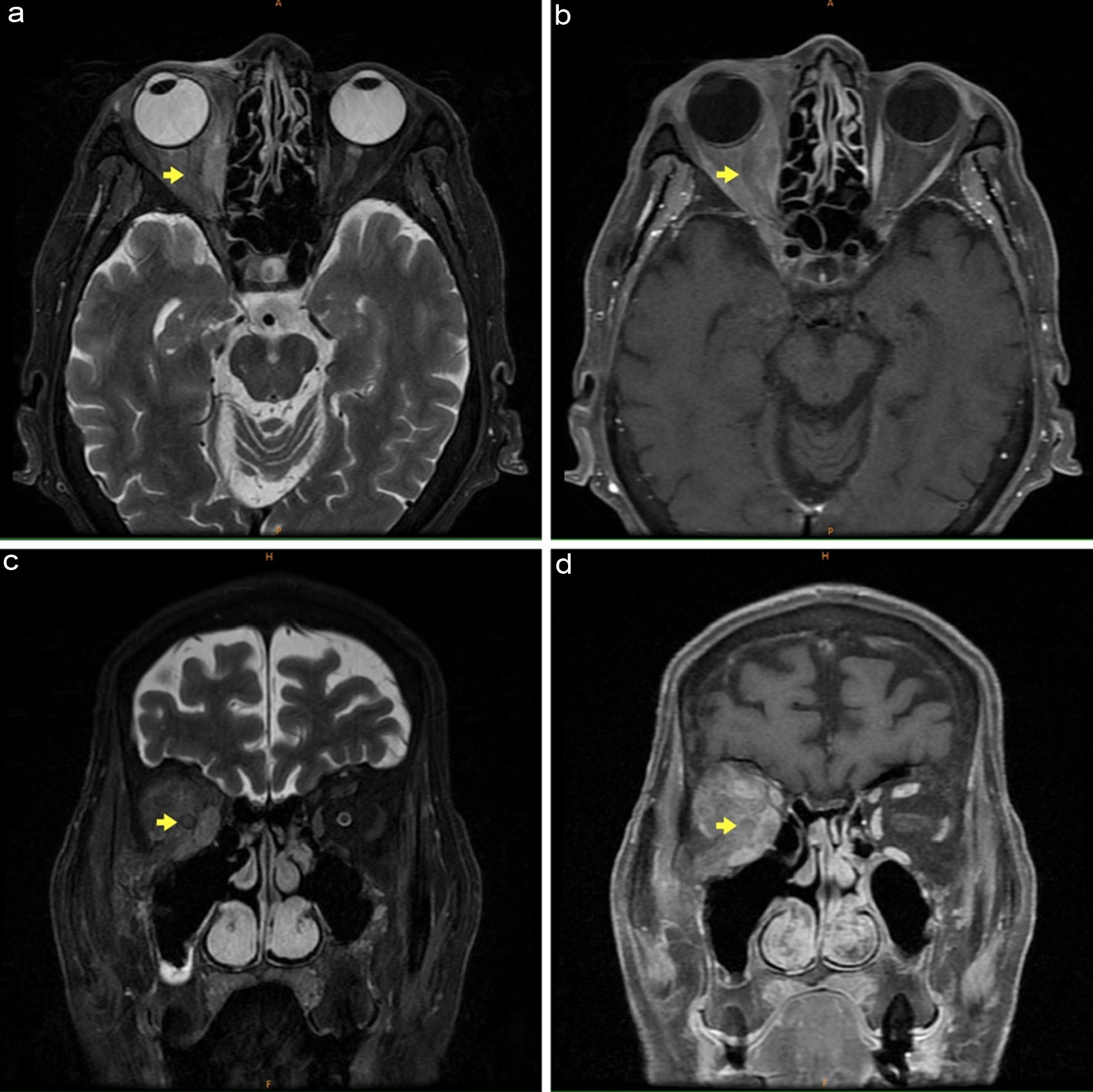
One week later, the patient’s condition worsened: best-corrected visual acuity dropped to 20/60 in the right eye and remained 20/40 in the left. His right pupil was dilated to 4 mm with a sluggish light response. There was progression in ophthalmoplegia, with adduction restricted to the midline and increased limitations in upgaze and downgaze to 80% of normal. A slight reverse relative afferent pupillary defect was noted in the right eye. The posterior segment examination showed normal optic disc cupping at 0.3, sharp and pink in color, a flat retina, and a healthy fovea. These findings, as depicted in Figure 1, suggested partial oculomotor nerve palsy with pupillary involvement and accompanying optic neuropathy, leading to a diagnosis of OAS in the right eye.
 Click for large image | Figure 1. Gaze positions demonstrating partial oculomotor nerve palsy with pupillary involvement in the right eye. |
Diagnosis
The laboratory findings are summarized in Table 1. Blood tests revealed mild anemia and mild hyponatremia, with all other parameters within normal limits. Lumbar puncture demonstrated normal cerebrospinal fluid pressure, a white blood cell count of 2, and no malignant cells identified on cytological examination.
 Click to view | Table 1. Laboratory Test Results of the Case |
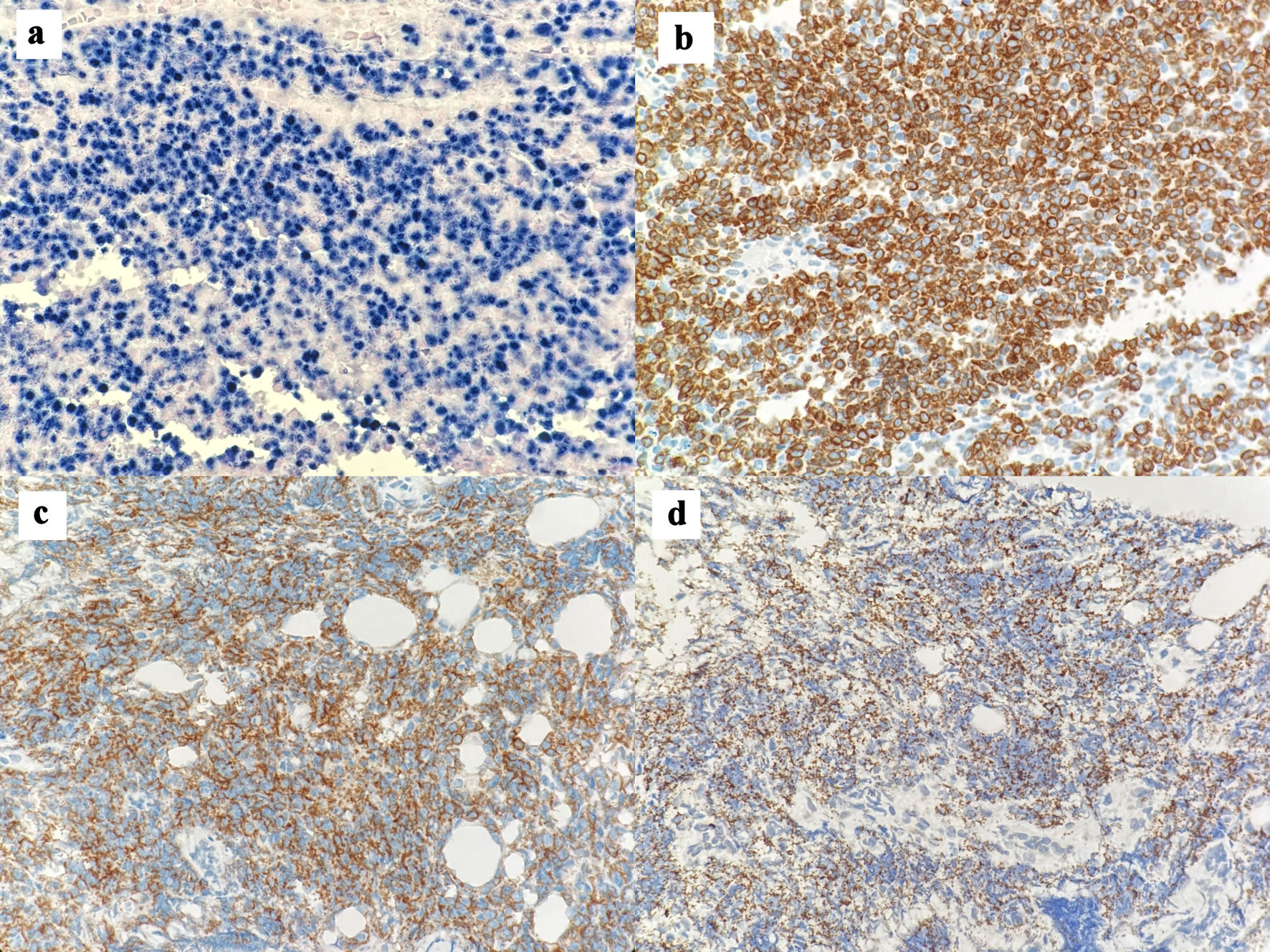
Magnetic resonance imaging (MRI) revealed diffuse, heterogeneous isointensity on T2-weighted images involving the superior, medial, and inferior rectus muscles, perioptic nerve sheath, and intraorbital fat of the right eye. These findings extended through the orbital apex region, with gadolinium enhancement, as shown in Figure 2.
 Click for large image | Figure 2. Magnetic resonance imaging (MRI) of the orbit: T2-weighted images demonstrate heterogeneous isointensity in the right superior, medial, and inferior rectus muscles, intraorbital fat, and perioptic nerve sheath complex, with post-gadolinium enhancement. No masses were detected in the paranasal sinuses (PNS). (a) Axial T2-weighted view. (b) Axial T1-weighted view with gadolinium enhancement. (c) Coronal T2-weighted view. (d) Coronal T1-weighted view with gadolinium enhancement. The yellow arrows indicate the position of the right optic nerve. |
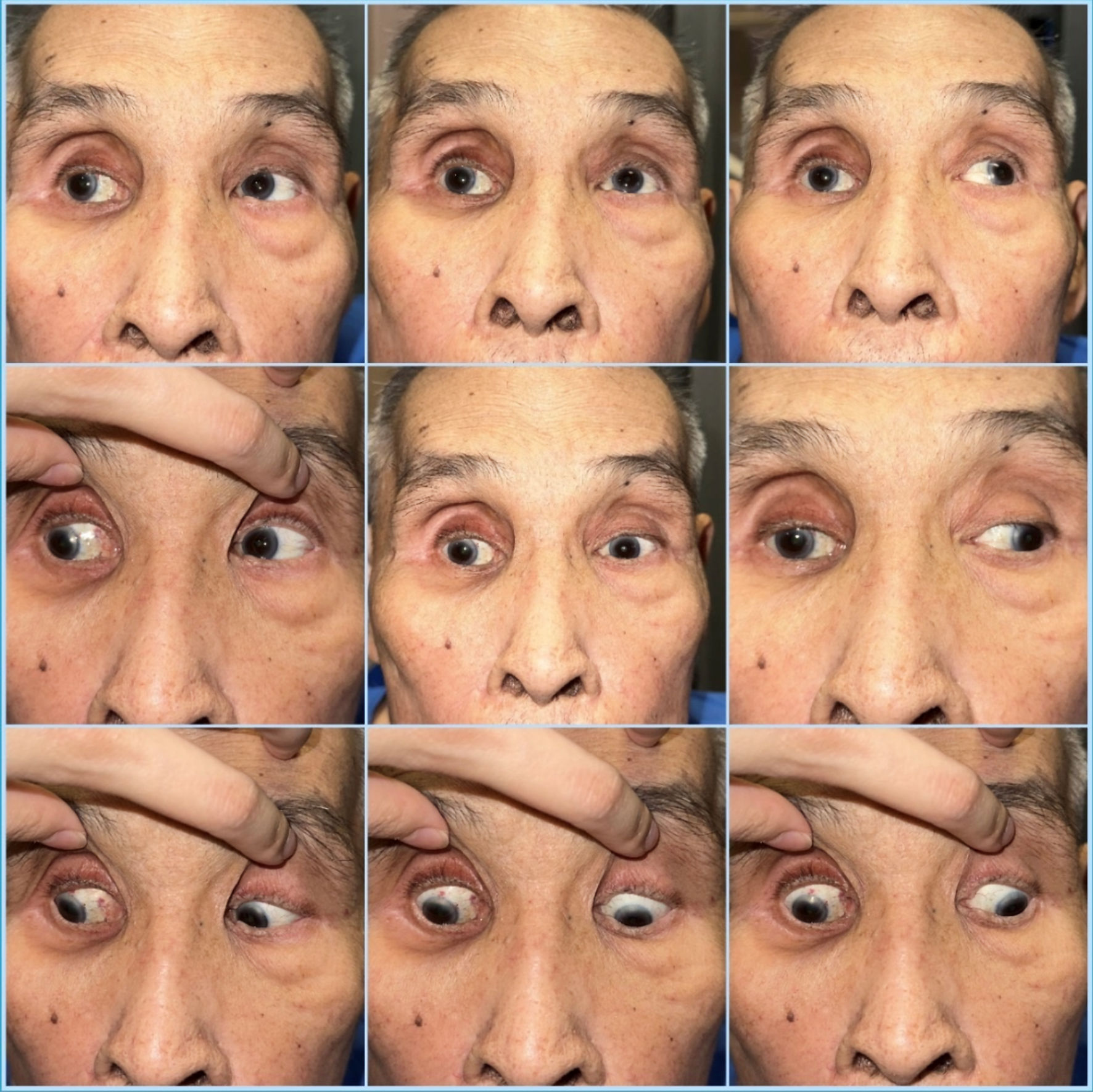
A tissue biopsy was necessary to determine the appropriate treatment plan for this case. The right medial rectus muscle was selected for biopsy. As MRI indicated, it was the most prominently involved muscle and the most accessible of the three affected recti. A limbal approach was employed to excise the medial rectus muscle tissue for histopathological examination. Pathological analysis revealed atypical round cell infiltration in the muscle. Immunohistochemical studies demonstrated that the lymphoma cells were positive for CD3 and Epstein-Barr virus-encoded RNA (EBER), but negative for CD20, CD30, and AE1/AE3. The Ki-67 proliferative index was approximately 80%. Additional staining confirmed positivity for TIA-1 and CD56, leading to extranodal NK/T cell lymphoma diagnosis. The histopathological and immunohistochemical findings are displayed in Figure 3.
 Click for large image | Figure 3. Histological and immunohistochemical images of the tumor. (a) The cells are positive for in situ hybridization for Epstein-Barr virus-encoded RNA (EBER) (× 40). (b) The cells are positive for CD3 staining (× 40). (c) The lymphocytes are positive for CD56 staining (× 40). (d) The lymphocytes are positive for TIA-1 staining (× 40). |
Treatment
A hematologist was consulted, and the diagnosis of ENKTL was confirmed through tissue pathology. Before starting treatment, his best-corrected vision was gradually worsening to the point of only being able to detect hand movements with good light projection in the right eye. The right optic disc appeared erythematous and mildly swollen, with no retinal infiltration, while the left eye remained unchanged. Additionally, the ophthalmoplegia was limited and showed no signs of progression. The treatment chosen was chemotherapy, specifically using the AspaMetDex regimen, which consists of methotrexate (MTX) at a dosage of 3 g/m2, L-asparaginase at 6,000 U/m2, and dexamethasone at 40 mg. The chemotherapy course lasted for 21 days, followed by an interval of 21 days, with plans for four to six cycles depending on the patient’s response.
Follow-up and outcomes
Upon follow-up, the patient’s vision improved to be able to count fingers at 1 foot 1 week after starting chemotherapy. His best-corrected vision gradually improved, as did his ocular movement, as shown in Figure 4. It is worth noting that only two chemotherapy cycles were administered during this report, and the long-term prognosis remains inconclusive. No systemic side effects were reported during the treatment.
 Click for large image | Figure 4. Gaze positions demonstrating improvement of oculomotor nerve palsy in the right eye. |
| Discussion | ▴Top |
Non-Hodgkin lymphomas (NHLs) are the most common malignant tumors found in orbit. In contrast to MALT lymphoma, NK/T-cell lymphoma (NKTCL) exhibits distinct characteristics, including low incidence, rapid disease progression, and a high mortality rate. Extranodal NKTCL is a rare and highly aggressive lymphoproliferative disorder closely linked to EBV infection [1, 2]. It most commonly originates in the nasal cavity and PNS (70% of cases), but it can also affect other sites such as the skin, salivary glands, liver, lymph nodes, gastrointestinal tract, lungs, and testes [1, 5, 10-12]. The prognosis for extranodal NKTCL is generally poor, with an average survival time of 12.5 months. When the orbit is involved, the median survival decreases significantly to just 4 months [1, 10, 11].
EBV plays a critical role in developing ENKTL, nasal type, a highly aggressive malignancy. This lymphoma is notably prevalent in East Asia and among indigenous populations in Latin America, indicating a genetic predisposition. EBV’s involvement in ENKTL is linked to specific viral strains, with type A and type B showing different oncogenic potentials, particularly through variations in the latent membrane protein 1 (LMP1). Genetic analyses of ENKTL have identified recurrent mutations, such as those affecting the JAK-STAT (Janus kinase/signal transducers and activators of transcription) pathway, BCOR, DDX3X, and TP53, highlighting mechanisms like immune evasion and disruptions in tumor suppression. These findings underscore the complexity of EBV-driven lymphomagenesis in ENKTL [13].
ENKTL presenting as OAS without nasal involvement is a rare and diagnostically challenging condition. Accurate diagnosis requires a multidisciplinary approach, combining imaging and histopathological techniques. Contrast-enhanced MRI is pivotal for evaluating soft tissue involvement at the orbital apex, but as seen in this case, it may not always raise suspicion of ENKTL when external ocular examinations are normal. Other potential causes of “silent” OAS include slow-growing tumors, vascular conditions, indolent infections, or benign entities, necessitating careful differentiation [14]. A definitive diagnosis relies on obtaining sufficient tissue via biopsy, especially in cases lacking nasal involvement, with immunohistochemical markers such as CD56, granzyme B, and EBER confirming ENKTL [15, 16].
A literature review indicates that ENKTL typically involves the nasal cavity and midline facial structures; orbital involvement without nasal lesions is rare. These cases often present in advanced stages with an aggressive clinical course. Common presentations in the literature include progressive proptosis, eyelid swelling, pain, and significant chemosis, which can easily be mistaken for inflammatory or infectious conditions. Partial oculomotor nerve palsy as an initial symptom, progressing to OAS, is particularly unusual, as it generally results from local spread from the nasal region rather than presenting as a primary orbital condition.
Since the initial report from Coupland et al [4], several case studies have documented this atypical manifestation [3, 5-12]. Previous case reports highlight the diagnostic challenges of ENKTL when it resembles other orbital conditions like idiopathic orbital inflammation, sarcoidosis, or other lymphoproliferative disorders. Diagnostic delays sometimes occur due to normal anterior segment findings, with only subtle symptoms such as isolated cranial nerve involvement or optic neuropathy. Notably, Meel et al [7] described a similar case with a “quiet eye” appearance that obscured early detection. This case contributes to the limited literature on primary orbital ENKTL and underscores the importance of heightened clinical awareness for this rare presentation.
The case presented here is unique in several respects. Firstly, the patient exhibited isolated oculomotor nerve dysfunction along with progressive optic neuropathy, despite having a normal ocular examination - a highly unusual scenario for ENKTL. Secondly, the absence of nasal lesions, typically characteristic of ENKTL, further distinguishes this case as rare. These features underscore the potential for ENKTL to manifest in subtle and atypical ways that can complicate conventional diagnostic approaches.
Additionally, it is important to exclude nonspecific inflammatory diseases due to the positive neuroimaging findings, which show hypersignal T2 and gadolinium enhancement. This is particularly relevant when there are significant orbital signs of inflammation, such as ophthalmoplegia, chemosis, and proptosis, as noted in previous case reports [6, 8, 12]. However, our case does not present any orbital signs suggesting these conditions.
In our case, we selected the AspaMetDex regimen - comprising L-asparaginase, methotrexate, and dexamethasone - to treat extranodal NK/T-cell lymphoma (ENKTL) that presented as OAS. Traditional anthracycline-based regimens, such as cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP), have shown poor outcomes in treating ENKTL due to the inherent resistance of NK/T cells to anthracyclines. Previous case reports have emphasized the ineffectiveness of CHOP in achieving durable responses [5, 10, 11]. L-asparaginase-based regimens, like AspaMetDex and SMILE, have demonstrated superior efficacy by targeting the metabolic vulnerabilities of ENKTL, significantly improving survival rates [7, 8]. This choice aligns with the National Comprehensive Cancer Network (NCCN) guidelines, which recommend L-asparaginase-based therapies as the first-line treatment for ENKTL [17]. We specifically chose AspaMetDex for its balance of efficacy and reduced toxicity compared to the more intensive SMILE regimen, reflecting the evolution of evidence-based treatment strategies for ENKTL.
In this case, the normal findings in the external eye and the isolated cranial nerve involvement created a diagnostic blind spot where standard ophthalmic examinations may not reveal any abnormalities. This highlights the necessity for a thorough neuro-ophthalmic assessment and advanced imaging techniques when clinicians encounter unexplained cranial neuropathies, even when the anterior segment appears unremarkable. This case enhances our understanding of the disease spectrum of ENKTL, emphasizing that a high index of suspicion is essential when evaluating rare forms of orbital involvement.
Limitations
This case is not without its limitations. First, the lack of nasal symptoms led to an initial diagnostic delay, highlighting the challenges of early recognition in such atypical presentations. While biopsy remains the gold standard for diagnosis, the small sample size from a targeted orbital biopsy could result in a missed or inconclusive diagnosis if the tissue is not representative of the disease. Furthermore, the rarity of ENKTL presenting without nasal lesions limits the generalizability of this case, as it is an uncommon manifestation that may not reflect the broader clinical spectrum of the disease.
Another limitation is the difficulty in ruling out other potential orbital pathologies, such as idiopathic orbital inflammation or other malignancies, which can present with similar neuro-ophthalmic symptoms. This diagnostic overlap requires careful interpretation of histopathological findings and close follow-up to monitor disease progression. Additionally, the aggressive nature of ENKTL underscores the importance of timely diagnosis. Still, the subtlety of clinical findings in this case suggests that current diagnostic algorithms may need refinement to include such atypical presentations.
Future research on ENKTL should prioritize enhancing early diagnostic methods, particularly for atypical cases without nasal involvement. Advances in molecular imaging and genetic profiling could aid in early detection and targeted therapies. A deeper understanding of genetic mutations, like those in the JAK-STAT pathway, may lead to more personalized treatments and improved survival outcomes for this aggressive lymphoma.
Conclusions
This case of NK/T-cell lymphoma presenting as OAS without nasal involvement adds valuable insights to the rare presentations of ENKTL. It emphasizes the need for high clinical suspicion, detailed neuro-ophthalmic assessment, and the use of advanced imaging and biopsy when progressive optic neuropathy and cranial nerve palsies occur without clear ocular or nasal signs. Standard clinical exams may not always reveal subtle abnormalities, underscoring the importance of thorough evaluation.
Learning points
A diagnostic challenge is NK/T-cell lymphoma with OAS, especially with normal ocular appearance. Reduced vision may mask signs of double vision, making clinical examination crucial. A tissue biopsy is recommended in all cases of OAS to facilitate accurate diagnosis and guide management.
Acknowledgments
We are grateful to Dr. Thitiporn Ratanapojnard for her invaluable guidance. Her expertise and insights shaped our study. We also thank the Ophthalmology Division of Phramongkutklao Hospital for their generous resources and support. Moreover, we thank Dr. Kantang Satayasoontorn for being an immunohistopathology tissue reviewer consultant and providing the tissue staining figure.
Financial Disclosure
This study was not supported by any sponsor or funder.
Conflict of Interest
The authors have no conflict of interest to declare.
Informed Consent
Written informed consent was obtained from the patient to publish the details of their medical care and any accompanying images.
Author Contributions
WS: study concept and design, manuscript drafting, and study supervision. PK: interpretation of imaging data and critical revision. All authors approved the final version of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
ENKTL: extranodal natural killer/T-cell lymphoma; MRI: magnetic resonance imaging; EBV: Epstein-Barr virus; MALT: mucosa-associated lymphoid tissue; AST: aspartate transaminase; ALT: alanine transaminase; EBER: Epstein-Barr virus-encoded RNA; MTX: methotrexate; JAK-STAT: Janus kinase/signal transducers and activators of transcription
| References | ▴Top |
- Au WY, Weisenburger DD, Intragumtornchai T, Nakamura S, Kim WS, Sng I, Vose J, et al. Clinical differences between nasal and extranasal natural killer/T-cell lymphoma: a study of 136 cases from the International Peripheral T-Cell Lymphoma Project. Blood. 2009;113(17):3931-3937.
doi pubmed - Suzuki R, Takeuchi K, Ohshima K, Nakamura S. Extranodal NK/T-cell lymphoma: diagnosis and treatment cues. Hematol Oncol. 2008;26(2):66-72.
doi pubmed - Kwong YL. Natural killer-cell malignancies: diagnosis and treatment. Leukemia. 2005;19(12):2186-2194.
doi pubmed - Coupland SE, Foss HD, Assaf C, Auw-Haedrich C, Anastassiou G, Anagnostopoulos I, Hummel M, et al. T-cell and T/natural killer-cell lymphomas involving ocular and ocular adnexal tissues: a clinicopathologic, immunohistochemical, and molecular study of seven cases. Ophthalmology. 1999;106(11):2109-2120.
doi pubmed - Hon C, Kwok AK, Shek TW, Chim JC, Au WY. Vision-threatening complications of nasal T/NK lymphoma. Am J Ophthalmol. 2002;134(3):406-410.
doi pubmed - Jing D, You D, Liu Z, Wang W. Primary orbital extranodal natural killer/T-cell lymphoma, nasal type, without nasal involvement. J Clin Med. 2022;11(23):7010.
doi pubmed - Meel R, Dhiman R, Wadhwani M, Kashyap S, Sharma S, Gogia A. Isolated extranodal natural killer T-cell lymphoma of the orbit in a young patient: complete regression with the SMILE regimen. Ocul Oncol Pathol. 2017;3(1):45-48.
doi pubmed - Okada A, Harada Y, Inoue T, Okikawa Y, Ichinohe T, Kiuchi Y. A case of primary extranodal natural killer/T-cell lymphoma in the orbit and intraocular tissues with cerebrospinal fluid involvement. Am J Ophthalmol Case Rep. 2018;11:37-40.
doi pubmed - Woog JJ, Kim YD, Yeatts RP, Kim S, Esmaeli B, Kikkawa D, Lee HB, et al. Natural killer/T-cell lymphoma with ocular and adnexal involvement. Ophthalmology. 2006;113(1):140-147.
doi pubmed - Ely A, Evans J, Sundstrom JM, Malysz J, Specht CS, Wilkinson M. Orbital involvement in extranodal natural killer T cell lymphoma: an atypical case presentation and review of the literature. Orbit. 2012;31(4):267-269.
doi pubmed - Marchino T, Ibanez N, Prieto S, Novelli S, Szafranska J, Mozos A, Graell X, et al. An aggressive primary orbital natural killer/T-cell lymphoma case: poor response to chemotherapy. Ophthalmic Plast Reconstr Surg. 2014;30(5):e131-134.
doi pubmed - Dai W, Zhong M, Shen W, Zou K, Bai CG. Natural killer T-cell lymphoma originating from the orbit. Chin Med J (Engl). 2012;125(9):1677-1680.
pubmed - Montes-Mojarro IA, Fend F, Quintanilla-Martinez L. EBV and the pathogenesis of NK/T cell lymphoma. Cancers (Basel). 2021;13(6):1414.
doi pubmed - Badakere A, Patil-Chhablani P. Orbital apex syndrome: a review. Eye Brain. 2019;11:63-72.
doi pubmed - Pongpruttipan T, Sukpanichnant S, Assanasen T, Wannakrairot P, Boonsakan P, Kanoksil W, Kayasut K, et al. Extranodal NK/T-cell lymphoma, nasal type, includes cases of natural killer cell and alphabeta, gammadelta, and alphabeta/gammadelta T-cell origin: a comprehensive clinicopathologic and phenotypic study. Am J Surg Pathol. 2012;36(4):481-499.
doi pubmed - Schwartz EJ, Molina-Kirsch H, Zhao S, Marinelli RJ, Warnke RA, Natkunam Y. Immunohistochemical characterization of nasal-type extranodal NK/T-cell lymphoma using a tissue microarray: an analysis of 84 cases. Am J Clin Pathol. 2008;130(3):343-351.
doi pubmed - NCCN [Internet]. [cited Jan 11, 2025]. Guidelines Detail. Available from: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1483.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.