| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://jmc.elmerpub.com/ |
Case Report
Volume 15, Number 12, December 2024, pages 406-410
Diffuse Type Pancreatic Ductal Adenocarcinoma: The Linitis Plastica Type of the Pancreas
Mohammad Radwana, Basel Darawshaa, Subhi Mansoura, b, Safi Khuria, b, c
aDepartment of General Surgery, Rambam Health Care Campus, Haifa, Israel
bBilio-Pancreatic Division, HPB and Surgical Oncology Unit, Rambam Health Care Campus, Haifa, Israel
cCorresponding Author: Safi Khuri, Department of General Surgery, Rambam Health Care Campus, Haifa, Israel
Manuscript submitted October 8, 2024, accepted November 6, 2024, published online November 11, 2024
Short title: Diffuse Type PDAC
doi: https://doi.org/10.14740/jmc5062
| Abstract | ▴Top |
Pancreatic malignant tumors are diverse and characterized by aggressive nature with high mortality rates. Pancreatic ductal adenocarcinoma (PDAC) is the most common type of pancreatic malignant tumors and accounts for approximately 90% of pancreatic malignancies. A subtype of PDAC, diffuse type PDAC (DTP), is a very rare and underreported tumor, known for its aggressive traits. Although little data are available about this tumor subtype characteristics, it usually presents with distinct features that are different from the known ones in PDAC. Herein, we present a case of a 61-year-old male patient, who presented with abdominal discomfort, weight loss and newly diagnosed diabetes mellitus. An abdominal computed tomography (CT) scan showed an ill-defined mass at the uncinate process with diffuse dilatation of the main pancreatic duct. Endoscopic ultrasound (EUS)-guided fine-needle biopsy showed cellular atypia suspicious for malignancy. The patient underwent total pancreatectomy with Roux-en-Y reconstruction. His postoperative course was uneventful. The final histopathological report showed well-differentiated diffuse ductal adenocarcinoma involving the pancreatic head, neck and body.
Keywords: Diffuse type pancreatic ductal adenocarcinoma; Linitis plastica; Mortality; Surgery
| Introduction | ▴Top |
Pancreatic malignant tumors are diverse and characterized by aggressive nature with high mortality rates. They are considered the 11th most common cancer in the world, with a 5-year relative survival rate of 9-12% [1]. Although it is more common in the elderly age group of patients, it can occur at any age and accounts for 4.5% of all cancer deaths. These tumors usually develop as a solitary lesion from epithelial or non-epithelial origins with different molecular, biological and prognostic characteristics. The most common type of pancreatic cancer is pancreatic ductal adenocarcinoma (PDAC), which accounts for around 90% of cases [2]. The pancreatic head is the most common part involved by PDAC, followed by the neck, body and tail in a descending order. The well-established radiological characteristics of PDAC involving the pancreatic head are ill-defined, hypovascular mass coupled with dilatation of the main pancreatic and bile ducts (double duct sign). Possible other findings compatible with borderline disease (invasion of the confluence of adjacent vessels, lymphadenopathy) or metastatic disease (liver, lung or other organ metastasis) are common as well [3].
Appropriate radiological detection and staging are key elements in patient management, taking into consideration the following factors: a retroperitoneally located pancreas, non-specific presenting signs and symptoms, and aggressive biological nature [4]. Despite the advancements in the diagnostic techniques and treatment strategies of pancreatic cancer, it remains one of the most lethal neoplasms. Due to its poor response to chemotherapy and radiotherapy, surgery has the only potential to prolong survival [5].
Compared to focal single malignant lesion, cases of multicentricity of PDAC (known as diffuse type PDAC (DTP)), are extremely rare [6, 7]. The DTP is a rare subtype of PDAC and accounts for around 1-5% of PDACs. It presents with distinct features that are different from the conventional ones in PDAC and very little data are available about its radiological, endosonographic and histological characteristics. It can be easily misdiagnosed as other pancreatic lesions (such as pancreatitis, metastasis to the pancreas or lymphoma), and thus, requires a different approach and management plan [8, 9]. Choi et al described the radiological features of DTP after examining 14 cases. Such features include among others peripheral capsule-like structure, the absence of intratumor pancreatic duct dilatation, and lack of pancreatic parenchymal atrophy [10].
Herein, we present a unique case of a 61-year-old patient who was diagnosed with DTP following total pancreatectomy.
| Case Report | ▴Top |
Investigations
A 61-year-old male patient, with new onset diabetes mellitus (DM) treated by metformin, was admitted due to upper abdominal pain of a month’s duration. In addition, he suffered of unintended weight loss of 5 kg, anorexia and heartburn. It is worthy of mention that 2 years ago an abdominal computed tomography (CT) scan, done for constipation, showed dilation of the main pancreatic duct (MPD) of up to 8 mm at the pancreatic head and neck, a finding suspected for main duct intraductal papillary mucinous neoplasm (IPMN). For unknown reasons, the patient did not complete the workup he was advised to complete.
Diagnosis
On physical examination upon his admission, the patient’s vital signs were within normal limits. An abdominal examination revealed soft, lax and non-tender abdomen. No abdominal mass was palpated. Digital rectal examination was normal. Complete blood count, liver and kidney function tests were within normal limits. An abdominal CT scan showed solitary ill-defined hypodense space occupying lesion at the uncinate process. Furthermore, diffuse dilatation of the MPD of up to 1 cm was documented. Adjacent vessels (portal vein, superior mesenteric artery (SMA) and hepatic artery) were uninvolved (Figs. 1 and 2). Based upon the clinical presentation and abdominal CT scan findings, the working diagnosis was a main duct IPMN that presumably underwent neoplastic transformation to PDAC at the uncinate process. The patient was admitted to the General Surgery Ward with a diagnosis of pancreatic head space occupying lesion for further investigation.
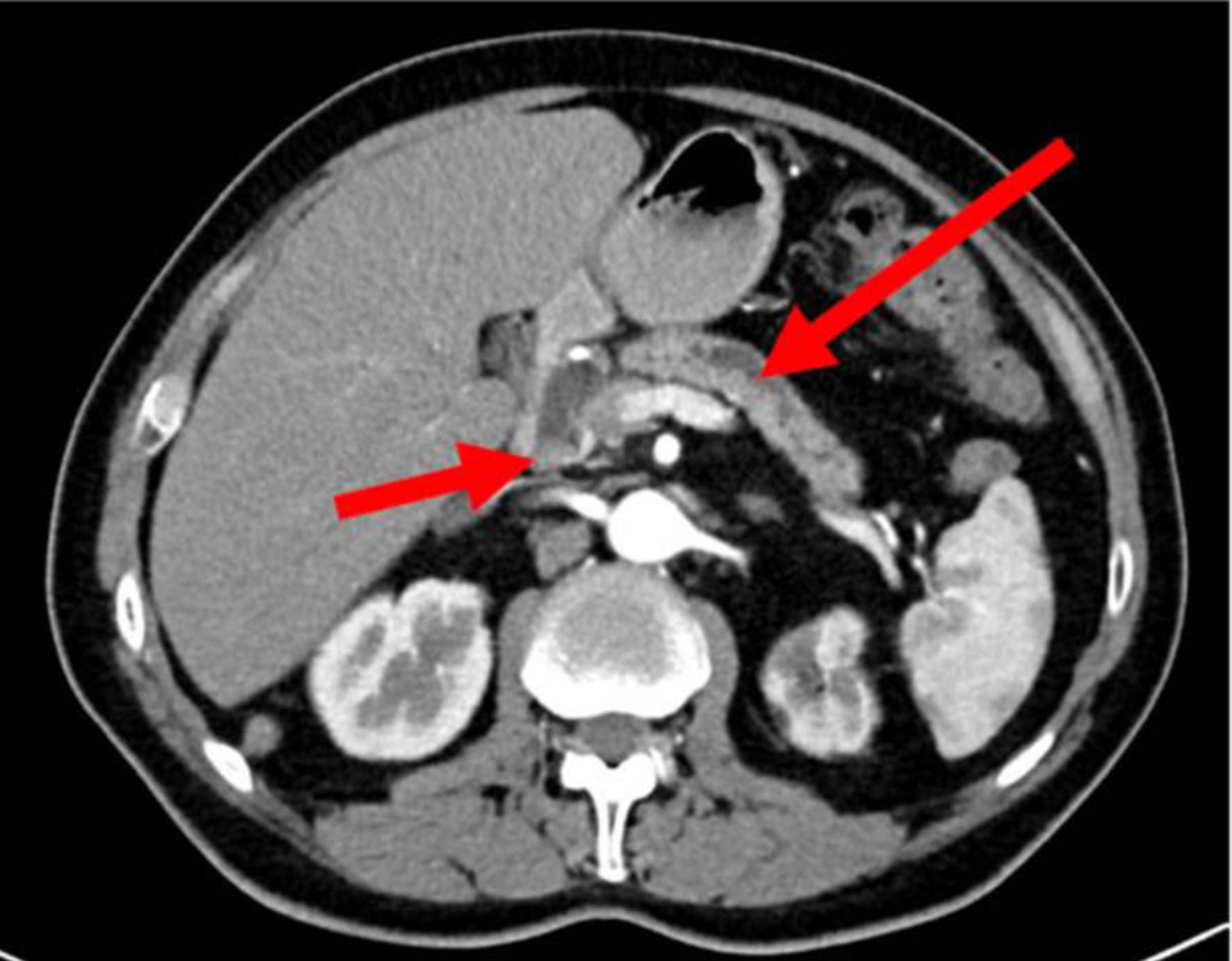 Click for large image | Figure 1. An axial cross-sectional CT scan of the abdomen showing hypodense lesion at the head of pancreas (short arrow) with a dilated main pancreatic duct (long arrow). CT: computed tomography. |
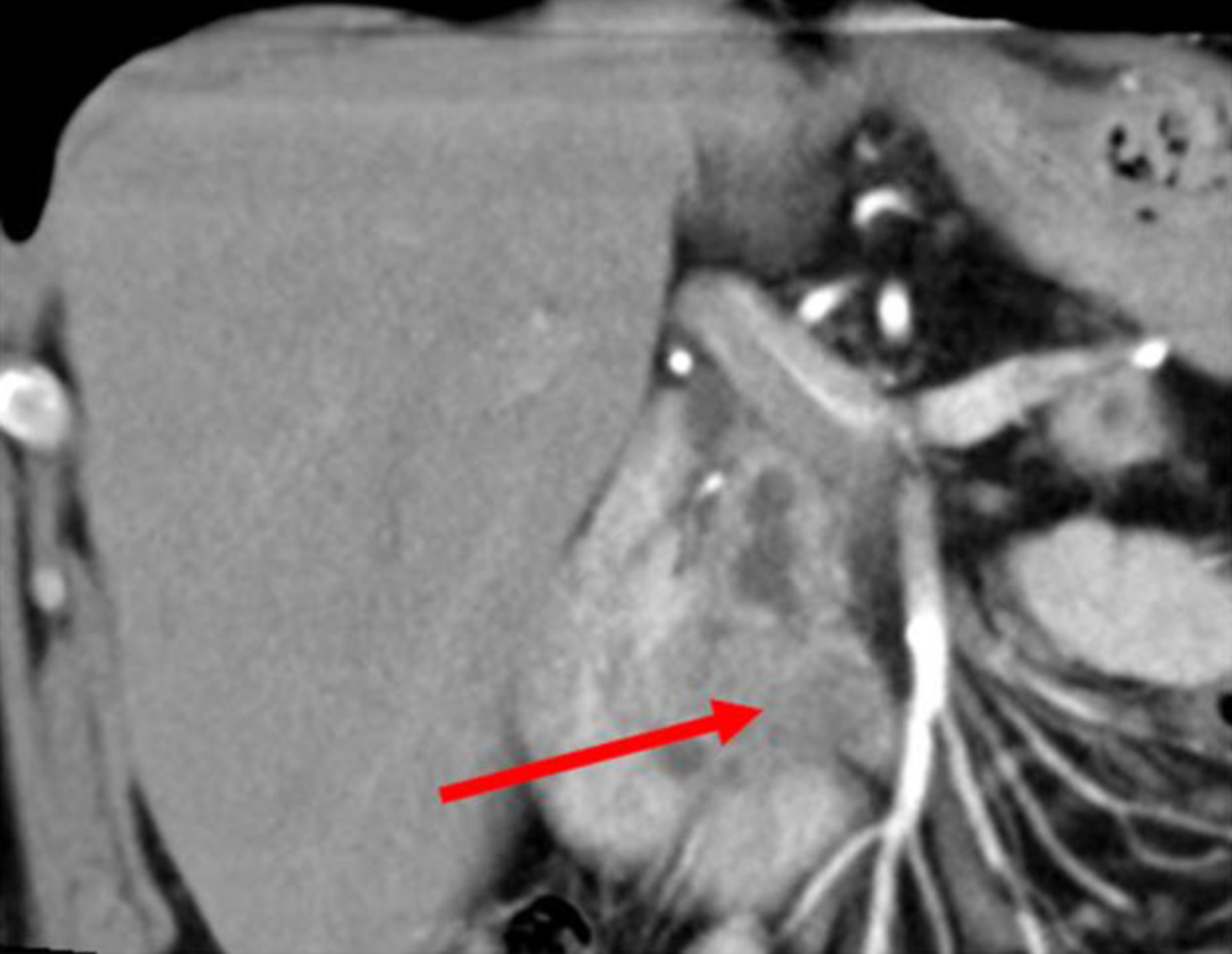 Click for large image | Figure 2. A coronal sectional abdominal CT scan showing an ill-defined hypodense lesion at the uncinate process of the pancreas (arrow). CT: computed tomography. |
During his admission, the patient underwent an endoscopic ultrasound (EUS), which revealed heterogeneous solid and cystic finding at the pancreatic head and uncinate process and a simple cyst at the pancreatic body. EUS-guided intracystic fluid aspiration showed findings compatible with IPMN (high levels of carcinoembryonic antigen (CEA) and amylase), while a fine-needle aspiration (FNA) of the solid component revealed cells with atypia highly suspicious for malignancy. Tumor markers including cancer antigen 19-9 (CA 19-9) and CEA were within normal limits. Positron emission tomography (PET)-CT scan revealed considerable FDG uptake at the pancreatic head without signs of metastasis.
Treatment
Following the diagnosis of pancreatic head lesion highly suspicious for PDAC, the patient’s case was discussed at the tumor board meeting for treatment decision. Two surgical options were suggested: total pancreatectomy vs. pancreatoduodenectomy (PD) with intra-operative frozen section of the pancreatic remnant. Pros and cons for each option were discussed as well. Advantages for total pancreatectomy include exclusion of the main postoperative complication, postoperative pancreatic fistula (POPF) and positive pancreatic margins involved by tumor cells. On the other hand, disadvantages include pancreatic exocrine and endocrine dysfunction and life-long treatment by insulin and pancreatic enzyme replacement therapy. Advantages and disadvantages for PD include partial pancreatic exocrine and endocrine function preservation and POPF and other well-known complications, respectively. After multi-disciplinary team (MDT) discussion, the treatment options (advantages and disadvantages of every option) were discussed with the patient, and it was decided to proceed with total pancreatectomy. The intra-operative findings showed no remote intra-abdominal metastasis, atrophic pancreas with hard texture involving the entirety of its length, dilated main pancreatic and common bile ducts, a solitary occupying lesion at the uncinate process with surrounding local desmoplastic reaction involving the inferior vena cava and superior mesenteric vein. Total pancreatectomy with Roux-en-Y reconstruction was completed.
His postoperative course was uneventful, and the patient was discharged home on postoperative day 10. The histopathological report showed well-differentiated PDAC involving the pancreatic head, neck and body, invading to the muscularis propria of the duodenum in the ampulla, to the fat around the pancreas and to lymphatic vessels. Numerous foci of IPMN with low-grade dysplasia at the tail were described as well. Surgical margins of the common hepatic duct were free of tumor. Two out of 22 lymph nodes were positive for PDAC.
Follow-up
On an outpatient clinic follow-up at 2, 6 and 12 weeks following operation, the patient was in good general condition with no remarkable physical examination findings. His blood glucose levels were within normal range. He was evaluated by an oncologist and treated with chemotherapy (FOLFIRINOX) for 12 cycles. Six months following operation, a PET-CT scan showed postoperative changes without any evidence of tumor recurrence.
| Discussion | ▴Top |
Approximately 90% of all pancreatic tumors are of ductal phenotype and the most frequent site is the pancreas head (60-70%) [10]. Three lesions in the pancreas can be a precursor for development of PDAC: pancreatic intraepithelial neoplasia (PanIN), IPMN and mucinous cystic neoplasia (MCN). PanIN is the most common precursor type. Multifocal invasion was rarely reported in patients with strong family history of pancreatic cancer. On the other hand, IPMN and MCN can be precursors for multifocal invasion [11]. In this case, a definite mass in the uncinate process was described along with diffuse IPMN, but a multifocal invasion was not confirmed before the operation.
Multiple pancreatic masses are a rare entity with a broad differential diagnosis: multifocal autoimmune pancreatitis, metastasis or neuroendocrine neoplasms [1]. Due to its rare incidence, DTP presentation and endoscopic findings are still not well known, nevertheless, as has been mentioned before, Choi et al described the largest series of DTP with radiological features including peripheral capsule-like structure, the absence of intratumor pancreatic duct dilatation, and lack of pancreatic parenchymal atrophy [12]. In his study, abdominal CT scan showed a solitary tumor in 11 patients and a tumor involving virtually the entire pancreas in the remaining three patients. No patients presented with multiple pancreatic masses.
Three theories were proposed regarding the pathogenesis of DTP: 1) rapid evolution from a focal PDAC; 2) delayed diagnosed pancreatic cancer; and 3) a synchronous multifocal tumor development. Although documented cases support the first and last theory, there are no reported cases that support the second one [6]. In our case, the most acceptable theory is the synchronous multifocal tumors deriving out of main duct IPMN.
In contrast to PDAC, DTP lacks the radiological feature of pancreatic atrophy. In addition, DTP lacks pancreatic enlargement, which is more associated with autoimmune pancreatitis. Both of the previously mentioned differential diagnoses require entirely different treatment regimen and have different prognosis [6]. Thus, a biopsy should be performed before initiating treatment of autoimmune pancreatitis in case of suspected malignancy.
Our patient had a unique radiological change between the two abdominal CT scans performed within 2 years. His last CT scan showed a single mass, with solid and cystic component, at the head of pancreas. The FNA was consistent with IPMN and cellular atypia. However, the pathology result after total pancreatectomy showed features of DTP which illustrates the importance of taking several samples and examining the whole pancreas. The histopathological features with diffuse involvement of the MPD by PDAC resemble the diffuse involvement of the stomach wall by gastric adenocarcinoma, known as linitis plastica.
In conclusion, although DTP is a rare entity, in cases of suspected multiple lesions within the pancreas, such as main duct IPMN involving the entire MPD, the entire pancreas must be evaluated. An MDT approach is warranted to discuss treatment options, with surgical resection (when feasible) carrying the best therapeutic outcomes. Total pancreatectomy is highly recommended in such cases.
Learning points
The main takeaway points from this case report: DTP, especially the linitis plastica type, is an extremely rare disease and is usually overlooked. In cases of PDAC development from main duct IPMN, it is recommended to localize the primary tumor and rule out any involvement of the MPD in its entirety before proceeding with any surgical treatment. An MDT approach is advisable and total pancreatectomy is the surgical option of choice.
Acknowledgments
None to declare.
Financial Disclosure
There was no specific funding source to be mentioned.
Conflict of Interest
The authors have no conflict of interest to declare.
Informed Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author Contributions
Mohammad Radwan and Basel Darawsha contributed to the writing of the manuscript. Subhi Mansour contributed to the design. Mohammad Radwan and Subhi Mansour contributed to literature research and editing of the manuscript. Safi Khuri was the mentor, and contributed to critical revision of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
CT: computed tomography; DTP: diffuse type pancreatic ductal adenocarcinoma; EUS: endoscopic ultrasound; IPMN: intraductal papillary mucinous neoplasm; PDAC: pancreatic ductal adenocarcinoma
| References | ▴Top |
- Nguyen HQ, Pham NTT, Hoang VT, Van HAT, Huynh C, Hoang DT. Diffuse pancreatic carcinoma with hepatic metastases. Case Rep Oncol Med. 2020;2020:8815745.
doi pubmed pmc - Mostafa ME, Erbarut-Seven I, Pehlivanoglu B, Adsay V. Pathologic classification of "pancreatic cancers": current concepts and challenges. Chin Clin Oncol. 2017;6(6):59.
doi pubmed - Kalra MK, Maher MM, Mueller PR, Saini S. State-of-the-art imaging of pancreatic neoplasms. Br J Radiol. 2003;76(912):857-865.
doi pubmed - Rawla P, Sunkara T, Gaduputi V. Epidemiology of pancreatic cancer: global trends, etiology and risk factors. World J Oncol. 2019;10(1):10-27.
doi pubmed pmc - Kanji ZS, Gallinger S. Diagnosis and management of pancreatic cancer. CMAJ. 2013;185(14):1219-1226.
doi pubmed pmc - Chow KW, Hu S, Sikavi C, Bell MT, Gisi B, Chiu R, Yap CG, et al. Diffuse-type pancreatic ductal adenocarcinoma mimicking autoimmune pancreatitis. ACG Case Rep J. 2023;10(6):e01070.
doi pubmed pmc - Izumi S, Nakamura S, Mano S, Suzuka I. Resection of four synchronous invasive ductal carcinomas in the pancreas head and body associated with pancreatic intraepithelial neoplasia: report of a case. Surg Today. 2009;39(12):1091-1097.
doi pubmed - Miyoshi H, Kano M, Kobayashi S, Ito T, Masuda M, Mitsuyama T, Nakayama S, et al. Diffuse pancreatic cancer mimicking autoimmune pancreatitis. Intern Med. 2019;58(17):2523-2527.
doi pubmed pmc - Choi EK, Park SH, Kim DY, Kim KW, Byun JH, Lee MG, Ha HK. Unusual manifestations of primary pancreatic neoplasia: radiologic-pathologic correlation. J Comput Assist Tomogr. 2006;30(4):610-617.
doi pubmed - Balci NC, Semelka RC. Radiologic diagnosis and staging of pancreatic ductal adenocarcinoma. Eur J Radiol. 2001;38(2):105-112.
doi pubmed - Goong HJ, Moon JH, Choi HJ, Lee YN, Choi MH, Kim HK, Lee TH, et al. Synchronous pancreatic ductal adenocarcinomas diagnosed by endoscopic ultrasound-guided fine needle biopsy. Gut Liver. 2015;9(5):685-688.
doi pubmed pmc - Choi YJ, Byun JH, Kim JY, Kim MH, Jang SJ, Ha HK, Lee MG. Diffuse pancreatic ductal adenocarcinoma: characteristic imaging features. Eur J Radiol. 2008;67(2):321-328.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.